There is limited knowledge about determinants of chronic bronchitis (CB) among Aboriginal children and adolescents in Canada. The objective of the study was to determine the prevalence and associated risk factors of chronic bronchitis in Aboriginal children (6-11 yrs.) and adolescents (12-19 yrs.).
Canadian Aboriginal Peoples Survey (APS)-2012 data were analyzed. Logistic regression analysis with appropriate weight variable to estimate regression coefficient and the balanced repeated replication method (to account for stratification and clustering) to compute robust standard errors were used. The outcome of interest for children was self-reported response by a parent/guardian to the question: 'Has your child ever had bronchitis?' and for adolescents self-reported response to the question 'Do you have chronic bronchitis?' Individual, environmental, and contextual factors were investigated for an association with CB.
Results are presented for (weighted numbers) 1,09,030 children 6-11 years old and 1,66,730 adolescents 12-19 years old. The prevalence of CB was 4.49% for boys (0.74% for adolescent boys) and 4.16% for girls (2.38% for adolescent girls).
The significant risk factors of CB were: age [odds ratio (OR) (95% confidence interval (CI) = 0.75 (0.66-0.86) for age group 9-11 years compared to age group 6-8 years]; household income (1.82 [1.56-2.13] for $25,000-$44,999 income category compared to income group ≥ 85,000), body mass index (1.54 [1.28-1.85] for overweight compared to normal), allergies (2.24 [1.96-2.56] for allergies compared to no allergies), asthma (5.69 [5.00-6.49] for asthma compared to no asthma), and location of residence (rural vs. urban). The relationship between the prevalence of CB and (i) Body mass index, and (ii) Location of residence, was modified by sex. There was significant increase in the prevalence of CB for obese boys (5.4%) comped to (i) Neither overweight nor obese boys (3%) and girls (4%) and (ii) Obese girls (3.5%). Girls residing in rural areas had the significantly increased prevalence (5.6%) of CB compared to boys irrespective of their location residence and girls who live in urban areas.
The significant risk factors of CB were: age (4.25 [3.58-5.04] for 15-19 years compared to 12-15 years), household income (3.22 [2.42-4.29] for income category < $25,000 compared to income category ≥ $85,000), parent's education (1.60 [1.20-2.17] for 'less than or some high school' compared to 'university education'), smoking in house (1.80 [1.53-2.13] for 'smoking house' compared to 'non-smoking house'), and the location of residence. The relationship between the prevalence of CB and (i) Body mass index, and (ii) Location of residence was modified by sex. Boys (2.5%) and girls (2.2%) with BMI > 30 had significantly higher prevalence compared to boys (0.57%) and girls (1.4%) with BMI < 25 and boys with BMI category 25-30.
Also, overweight girls had significantly higher prevalence with boys with normal weight and overweight boys. Contrarily to findings of effect of gender*location of residence on prevalence of CB, adolescents girls living in urban areas had significantly higher probability of CB (1.7%) compared to boys (1.25%) and girls (1.2%) living in rural areas and boys (0.39%) living in urban areas.
The prevalence of CB was related to modifiable risk factors age, household income, parental education, and environmental smoking, and location of residence.
Chronic bronchitis, Aboriginal, Children, Adolescents, Risk factors
COPD: Chronic Obstructive Pulmonary Disease; CB: Chronic Bronchitis; FN: First Nation; APS: Aboriginal Peoples Survey; WHO: World Health Organization; OR: Odds Ratio; CI: Confidence Interval; BMI: Body Mass Index; CCHS: Canadian Community Health Survey; ETS: Environmental Tobacco Smoke
In 2010, it was reported that the economic burden of chronic lung disease in Canada was $12 billion, which is estimated to double by 2030 for lung cancer, chronic obstructive pulmonary disease (COPD), and asthma [1]. "Chronic bronchitis occurs as part of the disease complex known as chronic obstructive pulmonary disease (COPD) which also includes emphysema and small airways disease" [2], and is a significant cause of morbidity and an underlying condition for the development of COPD [3]. According to the American Thoracic Society, CB is a respiratory disease defined as "cough productive of sputum for at least 3 months of the year for at least 2 years" [4]. The known and important risk factors for the prevalence and incidence of CB are smoking (personal smoking and exposure to secondhand smoke) [5-10] and indoor and outdoor air quality [6-12]. The poor indoor environment of homes in First Nation (FN) communities could be due to the prevalence of smoking inside the homes, houses in need of repairs, and the presence of dampness and mold/mildew inside the homes [6-10]. Other known risk factors of CB involve obesity [6-10,13] and socioeconomic status [6-9,14,15].
Based on the Aboriginal Peoples Survey (APS) 2006 data, the prevalence of CB was 3.1% among off-reserve boys and 2.8% among off-reserve girls aged 6-14 years [6]. Based on the 2002-2003 regional health survey, CB was more prevalent among First Nations youth (2.4%) than among youth in the general population (1.4%) [16]. Adverse respiratory health among Aboriginal children and youth may be associated with alarmingly high rates of smoking; as reported by the Public Health Agency of Canada, 26% of FN children and 70% FN of young adults living on-reserve report smoking, compared with 15% of Canadian youth in general [17]. It was reported that in Canada in 2012, current smoking rates among youth 15-19 years of age were: 11% of non-Aboriginal 33% in First Nations youth, 31% in Métis youth, and 56% in Inuit youth [18].
There are many reports which have looked at the prevalence of CB and associated risk factors among children and adults [6,9], but there is a lack of research on comparison of determinants of CB among children and adolescents. WHO identifies "adolescence as the period in human growth and development that occurs after childhood and before adulthood, from ages 10 to 19" [19,20]. Adolescence is a critical transition in the human lifespan, with the onset of puberty marking the passage from childhood to adolescence and biological processes initiating many aspects of growth and development [20].
To our knowledge, research on the prevalence of CB and about the determinants associated with CBs in Canadian Aboriginal children and adolescents in Canada is limited and has not been well established. The current manuscript based on analysis of the APS-2012 will augment our previous work [6] about off-reserve Aboriginal peoples based on APS 2006 and will complement our ongoing work based on the CIHR-funded research [8,9] with on-reserve First Nations people. The overall goal of this report is to evaluate demographic variables, environmental variables, socio-economic status, educational attainment of parents/guardian, and household income on the outcome of CB among Aboriginal people in Canada [off-reserve First Nations, Métis, and Inuit]. This manuscript reports findings on the prevalence of CB and risk factors associated with this disease among First Nations children (6-11 years old) and adolescents (12-19 years old) in Canada.
The APS-2012 was a national cross-sectional postcensal survey conducted from February, 2012 to July, 2012 [21]. The first APS survey was conducted in 1991 by Statistics Canada, and the APS-2012 was the fourth cycle. The APS-2012 was designed to follow and complement the census population and post-National Household Survey (which was conducted by Statistics Canada between May and August of 2011) [21].
The target population of the APS was Aboriginal peoples (First Nations people, Métis, and Inuit) living off-reserve throughout Canada, 6 years of age and over as of February 1, 2012. For the Aboriginal population, the survey consisted of the Aboriginal population belonging to either the "Aboriginal identity" population or the "Aboriginal ancestry" population.
"Aboriginal identity" refers to those persons who report identifying with at least one Aboriginal group (North American Indian, Métis or intuit, and /or those who report being a Treaty Indian or a Registered Indian, as defined by the Indian Act of Canada, and/or those who report being members of an Indian band or First Nation). "Aboriginal ancestry" refers to those persons who report at least one Aboriginal ancestry (North American Indian, Métis or Inuit)" [22,23].
Aboriginal people living on Indian reserves and settlements and in certain First Nations communities in Yukon and the Northwest Territories were excluded from this survey. The survey included information on: Aboriginal identity and ancestry, education, employment, language, income, health, communication technology, mobility, housing, and family background [21]. The survey provides these valuable data on Aboriginal children (6-11 years old), Aboriginal youth and adults (> 12-years-old; ref).
Questions for selected children and youth (aged 6 to 11) were completed by the person most knowledgeable (proxy interview) about the selected child/youth. For individuals between the ages of 12 and 17, interviews were conducted directly with the youth with prior approval of the youth's parent or guardian, and if the approval was not given by the youth, the data were collected from the parent/guardian [21]. Individuals 18 and 19 years old completed the questionnaires themselves. In some special circumstances proxy interviewees were obtained. These special circumstances included respondent's (i) Mental or physical wellness; (ii) Language restriction; or (iii) Absence during the survey period [21].
For this report, we considered Aboriginal children (6-11 years) and adolescents (12-19 years). Univariable association of prevalence of CB with each of the various risk factors was computed. Dichotomous logistic regression [24] was used to model the probability of chronic bronchitis in children (6-11 years) and in adolescents (12-19 years). An appropriate weight variable computed by methodologists of Statistics Canada was used at the analysis stage to account for the unequal probability of selection. Stratification and clustering (inherited in the study design) design effects of the cross-sectional complex survey design were accounted by computing robust standard errors of regression coefficients using the balance repeated replication method [10]. Analysis of this report is based on Aboriginal Peoples Survey-2012 conducted by Statistics Canada. For complex surveys conducted by Statistics Canada, sample size calculations based on appropriate formulae are completed prior to commencement of such surveys. Detailed information on sample size calculations, weighting (required for complex surveys) and response rates can be found in [21].
All potential scientifically important two-way interactions were examined. The strength of associations are presented as odds ratios (ORs) with associated 95% confidence intervals (95% CIs). STATA version 13 (Stata Corp, USA) were used to conduct all analyses [25].
The APS defined a "chronic condition" as a long-term condition that is expected to last or has already lasted at least six months and that was diagnosed by a health professional [21].
In the present study, we investigated the risk factors of CB for children 6-11 years old and adolescents 12-19 years (as defined by WHO) [19,20].
The APS included a set of questions designed to determine/investigate the chronic conditions of its Aboriginal participants. The variables used for the analysis are defined below.
The outcome variable in the present study was the presence or absence of CB. For children 6-11 years old, under the section listing chronic conditions, there was a statement: "In the following question, 'long-term conditions' refer to conditions that have lasted or are expected to last six months or more and have been diagnosed by a health professional", and under the list of chronic conditions "bronchitis", was listed as an option and was as the outcome variable.
For participants aged 12-19 (referred to as adolescents, according to the WHO definition), under the section listing chronic conditions, there was a statement:
Now I'd like to ask about certain chronic health conditions which you may have. I am interested in "long-term conditions" which are expected to last or have already lasted six months or more and that have been diagnosed by a health professional.
In the list of chronic conditions, there was a question: "Do you have chronic bronchitis, emphysema or chronic obstructive pulmonary disease or COPD?" Henceforth, we will call it chronic bronchitis because it was listed under the list of chronic conditions.
The prevalence of CB involves an interplay among several factors, such as demographic, socioeconomic and environmental variables, and the interactions between them. Thus, covariates of interest were demographic variables (which consisted of age and sex), environmental variables (which consisted of location of residence, size of residence, and geographical area), and enabling resources (such as socio-economic status, education level, and income). Age for children was divided into two groups: 6-8 years and 9-11 years. Age for adolescents was also divided into two categories: 12-14 years and 15-19 years. Location of residence had two categories: Rural or urban. Geographical area was a nominal variable with five categories: Atlantic (Halifax, Newfoundland and Labrador, New Brunswick, and Prince Edward Island) and Quebec, Ontario, Manitoba and Saskatchewan, Alberta, and British Columbia. Health-related variables consisted of chronic health conditions, including the absence or presence of asthma and allergies and body mass index (BMI). For children, we used Cole's method to calculate BMI categories: Neither obese nor overweight, overweight, and obese. For adolescents, we used three BMI categories: less than 25, 25-29.99, and ≥ 30.
Presence or absence of allergies was based on the following question:
Has a health professional diagnosed any of the following long-term conditions for: (i) Food or digestive allergies?; (ii) Respiratory allergies such as hay fever? ; and (iii) Any other allergies? Each with option 'Yes' 'No' 'Not applicable' 'Don't know/refusal'.
Questions on presence or absence of allergies used in statistical analysis was derived from the above three questions.
Presence or absence of asthma was based on the participant's age as follows:
If participant's age < 12 years:
Ever had asthma that was diagnosed by a health professional? With four options: 'Yes' 'No' 'Not applicable' 'Don't know/refusal'
If participant's age ≥ 12 years:
Do you have asthma? With four options: 'Yes' 'No' 'Not applicable' 'Don't know/refusal'
Socioeconomic status variables consisted of the education and income of the parent or guardian completing the form. Education had five categories: (a) Completed university certificate or diploma or degree; (b) Completed college or non-university certificate or diploma; (c) Some post-secondary or diploma; (d) Completed high school, and (e) Completed some high school.
Annual household income consisted of five categories: < $25,000, $25,000 to $44,999, $45,000 to $64,999, $65,000 to $84,999, and ≥ $85,000.
If the respondent was < 15-years-old, the question regarding residential school was asked in the following manner: Were any of the following members of your family ever a student at a residential school or a federal industrial school?
- Any of your grandparents?; Your mother?; Your father?
- Any of your brothers or sisters?
- Any of your other relatives?
Each question had four options: Yes; No; Not applicable; or don't know/refusal. If the respondent said "Yes" to the last question, he/she was asked to specify the relatives who attended the residential school.
If the respondent was < 20-years-old and ≥15 years, the questions about attendance at residential school were asked in the following manner: "Were any of the following members of your family ever a student at a residential school or a federal industrial school?"
- Any of your grandparents?; Your mother?; Your father?
Each question had four options: Yes; No; Not applicable; or don't know/refusal.
Question related to attendance at residential school used in the statistical analysis was derived based on the above relevant questions.
APS-2012 is a multi-stage complex survey. Hence, results are presented in term of weighted numbers (percentages) by using appropriate weights as mentioned under the Statistical Analysis section. Results are presented for (weighted numbers) 1,09,030 children 6-11 years old and 1,66,730 adolescents 12-19 years old. The prevalence of CB was 4.49% for boys 6-11 years old (0.74% for adolescent boys 12-19 years old) and 4.16% for girls 6-11 years old (2.38% for adolescent girls 12-19 years old).
The crude prevalence of bronchitis was 4.27% (4.37%) among children aged 6-8 (9-11) years old. The prevalence of bronchitis was highest in the region of Quebec (7.13%) and lowest in Alberta (2.83%). The prevalence of bronchitis was highest among children with the lowest household income (6.11%). A high prevalence of bronchitis (12.8% and 9.5%) was observed among children diagnosed with asthma and allergies, respectively. Overweight (5.22%) and obese children (4.76%) had a higher prevalence of bronchitis than the neither overweight nor obese group. Corresponding to each of the risk factor, unadjusted odds ratio (ORunadj) and 95% CI are given in Table 1.
Table 1: Characteristics of Aboriginal children and adolescents in Canada stratified according to presence/absence of chronic bronchitis, and unadjusted odds ratio estimates with 95% confidence intervals. View Table 1
Four different models were fitted, and the results are shown in Table 2. These models were based on the bivariable analysis, and all predictors significant at p < 0.20 were included in the multivariable analysis. These four models were as follows: (a) Model I-all predictors significant at p < 0.20 for children data (selected from Table 1) excluding allergies and asthma, (b) Model II-with all selected predictors including asthma but excluding allergies, (c) Model III-all selected variables including allergies but excluding asthma, and (e) Model IV-all selected variable including both allergies and asthma. Based on the multivariable model IV, the significant risk factors (p < 0.05) of CB were: Age (OR; 95% CI = 0.75 [0.66-0.86] for age group 9-11 years compared to age group 6-8 years); income (1.82 [1.56-2.13]) for the 25,000-44,999 income category compared to income group ≥ 85,000), body mass index (1.54 [1.28-1.85] for overweight compared to normal), allergies (2.24 [1.96-2.56] for allergies compared to no allergies), asthma (5.69 [5.00-6.49] for asthma compared to no asthma), and location of residence (rural vs. urban). Results for model IV were discussed here, because all variables in this model were significant at p < 0.05. Two interactions were significant indicating sex modified the relationship between (i) Body mass index and the prevalence of CB (Figure 1), and (ii) Location of residence and the prevalence of CB (Figure 2). There was significant increase in the prevalence of CB for obese boys (5.4%) comped to (i) Neither overweight nor obese boys (3%) and girls (4%) and (ii) Obese girls (3.5%) (Figure 1). Girls residing in rural areas had the significantly increased prevalence (5.6%) of CB compared to (i) Boys irrespective of their location residence and (ii) Girls who live in urban areas. Boys who live in urban areas have significantly higher prevalence of CB for boys who live in rural and girls who live in urban areas (Figure 2).
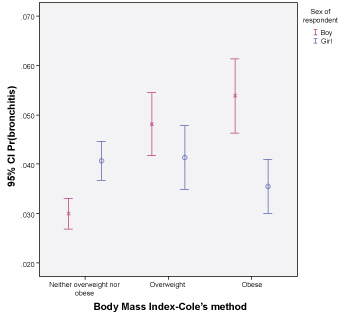 Figure 1: Mean predicted probabilities of chronic bronchitis for the interaction between body mass index and sex (for children 6-11 years old). View Figure 1
Figure 1: Mean predicted probabilities of chronic bronchitis for the interaction between body mass index and sex (for children 6-11 years old). View Figure 1
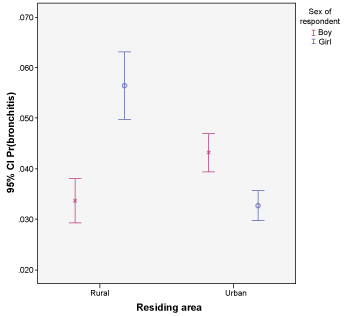 Figure 2: Mean predicted probabilities of chronic bronchitis for the interaction between location of residence and sex (for children 6-11 years old). View Figure 2
Figure 2: Mean predicted probabilities of chronic bronchitis for the interaction between location of residence and sex (for children 6-11 years old). View Figure 2
Table 2: Children (6-11 years old): Adjusted odds ratios (ORadj) and their 95% confidence interval (95% CI) based on logistic regression of the prevalence of chronic bronchitis (CB). View Table 2
The crude prevalence of bronchitis was 0.60% (2.06%) among adolescents aged 12-14 (15-19) years old. The prevalence of bronchitis among adolescents was highest in Alberta (3.24%) and lowest in Manitoba/Saskatchewan (2.83%). The prevalence of bronchitis was highest among adolescents with the lowest household income (3.38%). A high prevalence of bronchitis (6.70%) was observed among children diagnosed with asthma. Obese adolescents (2.96%) had a higher prevalence of bronchitis than the neither overweight nor obese group and overweight adolescents. Corresponding to each of the risk factor, unadjusted odds ratio (ORunadj) and 95% CI are given in Table 1.
Information on allergies was not available for adolescents. Hence, the two models were fitted, and the results are shown in Table 3. These two models are: Model I-all selected variables from Table 1 significant at p < 0.20 and excluding asthma-and Model II-all selected variables including asthma . For statistical analysis of the adolescents' data, steps similar to those taken for the children's data were followed. BMI: Compared to normal-weight adolescents, obese adolescents were significantly at a high risk of CB prevalence (5.25 [3.72-7.43]), and this association was less strong (although significant) when asthma was included in the model; exposure to secondhand smoke was significantly associated with the risk of CB, and asthma was significantly associated with the prevalence of CB. Similar to children, for adolescents as well gender modified the relationship between (i) Body mass index and the prevalence of CB (Figure 3), and (ii) Location of residence and the prevalence of CB (Figure 4). Boys (2.5%) and girls (2.2%) with BMI >30 had significantly higher prevalence compared to boys (0.57%) and girls (1.4%) with BMI < 25 and boys with BMI category 25-30. Also, overweight girls had significantly higher prevalence with boys with normal weight and overweight boys (Figure 3). Contrarily to findings of effect of gender*location of residence on prevalence of CB, adolescents girls living in urban areas had significantly higher probability of CB (1.7%) compared to boys (1.25%) and girls (1.2%) living in rural areas and boys (0.39%) living in urban areas (Figure 4).
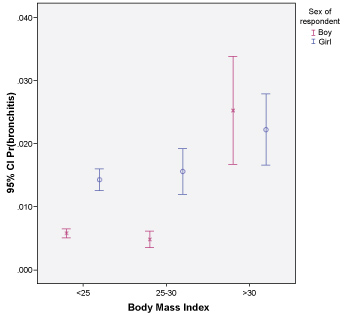 Figure 3: Mean predicted probabilities of chronic bronchitis for the interaction between body mass index and sex (for adolescents 12-19 years old). View Figure 3
Figure 3: Mean predicted probabilities of chronic bronchitis for the interaction between body mass index and sex (for adolescents 12-19 years old). View Figure 3
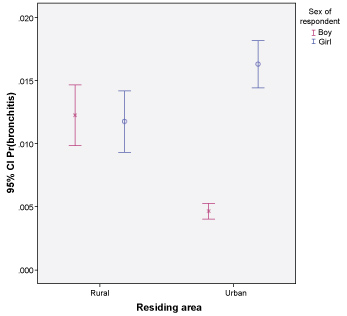 Figure 4: Mean predicted probabilities of chronic bronchitis for the interaction between location of residence and sex (for adolescents 12-19 years old). View Figure 4
Figure 4: Mean predicted probabilities of chronic bronchitis for the interaction between location of residence and sex (for adolescents 12-19 years old). View Figure 4
Table 3: ADOLESCENTS (12-19 years)-Adjusted odds ratios (ORadj) and their BRR 95% confidence interval (95% CI) based on logistic regression of the prevalence of chronic bronchitis (CB). View Table 3
By using the 2012 APS data, we determined the prevalence of CB and examined the associated risk factors in the First Nations children and adolescents residing off-reserve across Canada. We also compared the results based on the 2012 APS children's data with the findings we reported earlier [6] based on the APS-2006 children's data. While comparing the results from two APS surveys, we kept in mind the difference in age cut-offs between the 2006 APS (6-14 years for children) and the APS-2012 (6-11 years for children). To our knowledge, there is limited research on the prevalence and risk factors of CB among Aboriginal children and especially for Aboriginal adolescents.
We observed that the prevalence of CB was 4.49% for boys and 4.16% for girls 6-11 years old. Based on the 2006 APS data, we reported the prevalence of CB as 3.1% for boys and 2.8% for girls. We observed a greater prevalence of CB among boys and girls based on the 2012 APS data compared to the 2006 APS data, keeping in mind that age cut-offs defining children were different for boys and girls in these surveys. The differences in prevalence could be due to different age ranges used to define children in two surveys. The prevalence of CB was 0.74% for adolescent boys and 2.38% for adolescent girls. Based on the APS-2012 data, the prevalence of CB among boys (6-11 years) was six times the prevalence among (0.74%) adolescent boys, while the prevalence among girls (6-11 years) was 1.75 times the prevalence among adolescent girls (2.38%). In the 2012 APS survey, the survey question related to the presence/absence of chronic bronchitis was slightly different for children and adolescents. Based on our baseline survey of the First Nations Lung Health Project [26], the prevalence of bronchitis in children 6-17 years old residing in two reserve communities was 17.9% [9].
The trend of prevalence of CB among different regions of Canada was similar, based on the 2006 and 2012 APS data. The prevalence was slightly higher in all regions in 2012. The prevalence of bronchitis was highest among children in the two lowest household income categories (6.11%, based on the APS-2012 data, and 3.54% and 4.32% based on the APS-2006 data). A high prevalence of bronchitis (12.8% and 9.5%) was observed among children diagnosed with asthma and allergies, respectively. Overweight (5.22%) and obese children (4.76%) had a higher prevalence of bronchitis compared to the neither overweight nor obese group.
We fitted four multivariable models for children and two multivariable models for adolescents. Based on the models for children, we observed that male sex, lower education attainment for the parent/guardian, lower household income, the presence of allergies and/or asthma, rural residence, and residential school attendance were significantly associated with self-reported CB for children. Our findings based on APS-2006 that children aged 9-11 years were at lower risk for the prevalence of CB compared to those aged 6-8 years were in disagreement with the results we observed for the APS-2012 data (i.e., children in the age group 9-11 years were at higher risk compared to the 6-8-year-old children). We observed that girls (aged 6-11 years) had significantly higher prevalence of CB compared to (i) Boys (6-11 years) who live in rural areas and (ii) Girls who live in urban areas.
We observed that low income and poor educational attainment of the guardian were independently associated with the prevalence of CB, which were consistent with our earlier findings on off-reserve [6] and on-reserve [9] Aboriginal children, in Inuit children, and the results reported by other researchers on adult data [7,8].
We observed that allergies and asthma were associated with the prevalence of CB in off-reserve Aboriginal children, which supports our earlier findings of association between allergies and CB and asthma and CB [6]. Our previous work has shown strong positive association between asthma and CB, with ORs of 7.61 and 95% CI (6.91-8.37) and as well as positive association between allergies and CB with OR = 1.96 and 95% CI (1.78-2.16). The strong association between asthma and CB has been also shown by Pierre, et al. [27] and Cartel, et al. [28]. Pierre, et al. [28] reported the significant association of the prevalence of allergies (5.6% among Inuit children aged 0-14) and current asthma. Carter, et al. reported that the presence of CB increased the odds of asthma with OR of 6.4 (95% CI: 4.5-9.0).
The link between obesity and chronic bronchitis has been shown for Aboriginal children and youth [6,9] and for Aboriginal adults [8,10]. Similar associations have been reported for adolescents [29] for the general Canadian population [7,13,30]. We observed that sex modified the relationship between body mass index body mass index and the prevalence of CB among children. We observed that overweight and obese boys [6-11] had significantly higher prevalence of CB compared to girls who were neither overweight nor obese. Girls who were neither overweight nor obese had significantly higher prevalence of CB compared to boys in the same BMI category, however, obese girls had significantly lower prevalence of CB compared to obese boys. No significant difference was observed in the prevalence of CB (i) Between overweight and neither overweight nor obese girls, and (ii) Between overweight and obese boys. Normal weight and overweight adolescents girls had significantly higher prevalence compared to boys in these two BMI categories. Obese boys had significant higher prevalence of CB compared to normal and overweight boys. Lee, et al. (date) reported a strong association between obesity and the occurrence of bronchitis among adolescents [29].
Based on Canadian Community Health Survey (CCHS 2005) data, it was reported that exposure to ETS inside the home (adjusted odds ratios of 2.30 [95% CI; 1.46-3.63]) and vehicle (2.25 [1.42-3.58]) was significantly associated with chronic bronchitis in children and adolescents aged 12-19 years [30]. Personal smoking, exposure to environmental tobacco smoke (ETS), and indoor air quality are the most important and preventable risk factors for CB. Research has shown that many Aboriginal children are exposed to ETS because both parents and visitors smoke inside the home [8,9]. We observed ETS was a significant predictor of CB for adolescents, which supported the findings earlier published by other researchers regarding the association of personal smoking and second hand smoke with CB in children and youth [12,31,32].
Based on APS-2012 data we observed that gender was an effect modifier in the relationship between location of residence and the prevalence of CB. We observed that girls (6-11 yrs old) who lived in rural areas had significantly higher prevalence of CB compared to girls who lived in urban areas and to boys who lived either in rural or urban areas. Boys (6-11 yrs old) who lived in urban areas had significantly higher prevalence than boys who lived in rural areas. An opposite trend was observed for adolescents. Adolescent girls who lived in urban areas had significantly higher prevalence of CB compared to girls (6-11 yrs old) who lived in rural areas and to boys who lived either in rural or urban areas. There were no significant differences in the prevalence of CB among boys (6-11 yrs old) and girls (6-11 yrs old) who lived in rural areas. Based on APS-2006, rural location of residence was reported to have protective effect on the prevalence of CB compared to urban residents (OR, 0.72; 95% CI, 0.67-0.78) [6].
Based on APS-2012, we observed that residential school experience (either personally or by family members) was positively associated with the risk of CB for both children and adolescents who live off-reserve, which supports the earlier findings of association between attendance at a residential school, smoking, and CB [16,33]. However, based on our recent ongoing study of respiratory health of on-reserve First Nations people, we did not find a significant association between either of the variables related to residential school and the prevalence of CB [8].
There were several limitations related to this report. The major limitation was associated with the definition of CB. CB was defined as self-reported doctor diagnosed CB.
A similar definition has been used in several other studies [6-9,30]. In such definitions, there is a lack of clinical definition, which introduces the misclassification bias [6]. Accurate diagnosis of CB in childhood is difficult because there is a clinical overlap of symptoms associated with asthma and CB [6]. In APS-2012, for adolescents Definition for adolescents is a combination of CB, emphysema, and COPD. Therefore CB prevalence should be less than what we observed in this report. Another limitation was that information on allergies was not collected for adolescents, hence we were not able to investigate the association between allergies and prevalence of CB among adolescents.
To our knowledge, this is the first report that compared the risk factors of CB between Canadian Aboriginal children and adolescents residing off-reserve. Our results suggests that modifiable determinants of CB prevalence among Canadian Aboriginal children and adolescents living off-reserve are: obesity, household income, personal smoking and exposure to environmental tobacco smoke. Other significant risk factors, which are non-modifiable or difficult to modify are self-reported allergies and self-reported doctor-diagnosed asthma. Improving the respiratory health of Aboriginal children and adolescents in Canada will be addressing the social issues of respiratory health such as reducing smoking rates which will also turn into reduced environmental tobacco smoke, improving education which could result into better employment and consequently better income.
"This research was supported by funds to the Canadian Research Data Centre Network (CRDCN) from the Social Science and Humanities research Council (SSHRC), the Canadian Institute for Health Research (CIHR), the Canadian Foundation for Innovation (CFI) and Statistics Canada".
"Although the research and analysis are based on data from Statistics Canada, the opinions expressed donot represent the views of Statistics Canada or the Canadian Research Data Centre Network (CRDCN)".
Statistics Canada Research Data Centre at the University of Saskatchewan has obtained a Certificate of Approval from the University of Saskatchewan's Research Ethics Board, which allows researchers to conduct secondary analysis of data.
Not applicable.
Not Applicable.
All authors declare that they have no competing interests.
Not Applicable.