Background: Measuring overall dietary nutritional value necessary for wellness is complex for healthy individuals, and even more so for patients suffering from complex diseases such as Crohn's Disease. Clinical dieticians are challenged to provide beneficial dietary advice balanced against using incremental changes in patients' selected diets to increase long-term adherence to dietary improvements. The My Nutrition Index (MNI) is a validated, personalized nutritional scale based on personal characteristics and dietary needs. In this study, we evaluated and adapted the MNI for use in an inflammatory bowel disease (IBD) patient population and validated it against the recommended diets suggested by a certified dietician.
Methods: This is a cross-sectional study with patients' pre-consultation diets based on 24-hour recall of dietary intake and post dietary consultation diets as recommended by a certified dietician. Participants were Crohn's disease patients seen in the IBD subspecialty medical home at an academic IBD center, selected to represent the range of patients for whom a nutritional index would be most impactful. The primary outcome variable was the MNI for pre and post-consultation diets. Four focused subscales are also available: Vitamin Index, Mineral Index, Electrolyte Index, Macro Nutrient Index. In addition, consideration of Energy Ratio (observed calories relative to target calories) is important for IBD patients. The MNI and its subscales were calculated for each patient's diet pre and post-consultation with the certified dietician and presented graphically.
Results: The MNI and its subscales correctly marked the improved nutrient values of the recommended diets.
Conclusions: The MNI tool, while not a substitute for dietitian advice, can inform both patients and their nutrition providers with numeric feedback around the nutritional value of their diet and reinforce small, customized, incremental changes to reach their goals.
Personalized nutrition, Nutrition index, Crohn's disease, Dietary consultation, Incremental changes
Growing evidence supports the use of "food as medicine", with data supporting its benefits in preventing disease, managing chronic mental and physical symptoms and improving overall wellness. One barrier to understanding the full impact of nutrition on health is the lack of validated assessment tools that consider an individual's nutritional needs and status in context (e.g. age, gender, weight, food accessibility, cultural preferences, presence of medical conditions, dietary goals) and over time.
This gap has implications for both research and practice. Clinical dietitians often make incremental changes to patients' diets to improve their intake, and seek feedback to promote long-term adherence, but have little way of tracking how these expert-recommended and incremental changes improve diet quality. Cardiometabolic intervention trials have largely relied on the USDA's Healthy Eating Index (HEI) [1] as a way to capture change in diet quality associated with a specific dietary recommendation (e.g. low fat, low carbohydrate) [2]. While the HEI can capture multiple dietary changes simultaneously to determine improvement in diet quality, it does not capture more subtle changes to diet that might be necessary in conditions or settings in which dietary goals are more heterogeneous or less understood, such as Crohn's Disease.
Crohn's Disease is an immuno-inflammatory condition of the gastrointestinal tract, typically diagnosed in the second decade of life. The disease is incurable and lifelong and therefore disease self-management skills including nutrition are critical to outcome. Given nutrient absorption concerns, acute and chronic inflammation and unpleasant symptoms associated with eating, malnutrition rates in IBD range from 20-85%, and are associated with the poorest clinical outcomes, response to therapy and, therefore, quality of life [3]. Micronutrient depletion (primarily of calcium, vitamin B12, vitamin D, folate, iron, magnesium, vitamin B6, and zinc) and protein-energy malnutrition are of clinical concern in IBD patients [4]. A highly symptomatic condition, including urgent diarrhea, nausea, abdominal discomfort, fatigue, poor appetite and weight loss, food choices and eating behavior are often problematic and, when not addressed, can contribute to further decline. Further complicating its symptom profile, IBD itself is a highly heterogeneous disease, varying with respect to disease activity (e.g. flare vs. remission), disease behaviors (e.g. stricturing), disease location (e.g. small bowel, colon, esophagus, perianal) and surgical history (e.g. ostomy, short-bowel)- therefore one diet or approach does not fit all and nutritional goals often change over time. For example, individuals with stricturing Crohn's disease may need to follow a liquid or reduced particle size diet and a patient with small bowel Crohn's may require nutritional supplementation [5]. A patient with diarrhea may require changes to fiber intake, and or require increased hydration. Individuals with ostomies may need support with managing the thickness of output and maintaining hydration. In other words, dietitians working with these patients must be creative in how they alter a person's diet to optimize their nutrition without increasing their risk for an adverse outcome (e.g. bowel obstruction, dehydration).
Nutrition scientists working in IBD also struggle to capture nutrition in this population given the disease's heterogeneity and baseline differences in individual's eating behaviors and preferences. Successful diet trials require meals to be shipped to patients in order to control for micro and macronutrients across participants, but long-term adherence to a successful diet is limited when this is the case. Further, in other IBD research, nutrition is rarely evaluated as a co-variate, despite its likely contribution to outcome. Thus, a standardized metric of nutrition could improve both diet and other clinical research in IBD.
The My Nutrition Index (MNI) is a personalized dietary nutional metric which considers an individual's personal nutritional needs and status in context (i.e., based on patient characteristics and dietary preferences and goals) over time. The MNI incorporates 34 macro and micronutrients into a single score [6]. MNI is personalized by targeting nutrient ranges based on subject-specified characteristics and context such as age, sex, body size, activity level, behavior (e.g., smoking), and dietary restrictions and preferences. In this study, we evaluated and adapted the MNI and related subscales for use in Crohn's Disease. We hypothesized 1) The MNI would accurately capture the full range of nutrients and their value in an IBD patient diet; and 2) The MNI and its 5 subscales (Macronutrient Index, Energy-Ratio Index, Vitamin Index, Mineral Index, Electrolyte Index) would reflect small incremental changes in a patient's personal food choices and can be customized to the patient's needs and context to drive improved nutrient value.
Participants were Crohn's disease patients seen in the IBD subspecialty medical home at an academic IBD center. They were selected by the research team to represent the range of patients for whom a nutritional index would be most impactful. Each patient was newly diagnosed (within 1 year) with ileal Crohn's Disease. To be eligible, participants were required to meet two of the following criteria: 1) Disease or nutritional complexity; 2) At risk for malnutrition; 3) Impact of diet on quality of life. All patients worked with the dietitian for an evaluation of their nutritional status and guidance for symptom management through diet. The study was approved by the institutional ethics board [GCO#: 20-1036].
During their baseline dietitian consult, patients provided a 24-hour recall of food intake. This methodology has been shown to be valid and reliable for measuring nutritional value [7]. The dietitian then entered the 24-hour recall results into a validated digital tool, Cronometer®, which derives nutritional value from the USDA data bank of foods among other international databases. Data was also extracted from each patient's electronic medical record, including Montreal classification of Crohn's Disease [8], last office visit Harvey Bradshaw Index [9], most recent laboratory values [CBC (Hgb, Hct), chemistry (Na, Cl, Ca, K), anemia panel (B12, Ferritin), vitamins C, D, folate, zinc, magnesium] and inflammatory markers (CRP, ESR, fecal calprotectin)]. Based on the output of the Cronometer®, the dietitian (LM) then created an updated diet for the patient, recommending incremental changes in either food type, portion size or texture to the individual's 24-hour recall, while considering the patient's personal nutritional needs and preferences, disease state, bowel length and psychosocial context.
Pre and post diets were then submitted, along with patient characteristics including sex, age, height, weight, smoking status, alcohol and caffeine consumption, need for a low-fat/high protein diet, hypertension and activity level to the My Nutrition Index (MNI) calculator to determine whether the MNI would detect improvements in overall nutrition status based on small, incremental dietary changes recommended by an expert dietitian and whether subscales would also reflect these changes.
The MNI is comprised of 34 dietary components: Total fat, saturated fat, monounsaturated and polyunsaturated fat, energy, dietary protein, dietary carbohydrates, alcohol, caffeine, sugar, dietary fiber, vitamin E as alpha-tocopherol, vitamin C, cholesterol, potassium, sodium, calcium, magnesium, iron, phosphorus, zinc, thiamin, riboflavin, niacin, vitamin B5, vitamin B6, vitamin B12, vitamin A, vitamin D, vitamin K, manganese, chloride, folate, and selenium. It is a metric of how close each component is to guideline values based on the appropriateness of the response for the characteristics of the subject. It assigns higher scores for nutrient concentrations that fall within the published dietary guidelines recommended concentration range and assigns lower scores if intake for a given nutrient deviates from this optimal range (i.e., deficient or excess intake). It provides an overall index score ranging from 0 to 100, with higher scores reflecting a more nutritious diet. Thus, a perfect MNI score would be obtained if adequate intake of all nutrients is met. Four focused subscales are also available: Vitamin Index, Mineral Index, Electrolyte Index, Macro Nutrient Index. Each are on the same scale as the MNI (0 to 100) with higher scores indicating a more nutritious diet. In addition, consideration of Energy Ratio (observed calories relative to target calories) is important for IBD patients. Values for the MNI and subscales above roughly 90 indicate adequate nutrition on each scale. Given some of the unique nutritional concerns of Crohn's Disease patients, the MNI was also subjected to changes based on the patient IBD status. For example, during an IBD flare the MNI was altered to require higher electrolyte levels with focus on soluble fiber instead of any fiber (Table A1).
Table A1: Nutrient values per diet with recommendation indication for average adult (age 19-50 years-old). View Table A1
Five patients with Crohn's disease (60% female; 60% White, Non-Hispanic mean age 31, range 24-48, Mean BMI = 26, range 17-38) participated Table 1. All participants provided baseline diets and worked with the dietician (LM) to improve the nutritional value of the patient's diet through small, incremental achievable goals. The dietician based her diet recommendations on a variety of factors including disease characteristics, severity, activity and behavior, personal characteristics, patient preferences (e.g. kosher, vegan) and psychosocial determinants (See Table 2, Table 3, Table 4, Table 5 and Table 6).
Table 1: Patient characteristics for the five case studies. View Table 1
Table 2: Reported pre-consultation diet and recommended post-consultation diet for Subject 1. View Table 2
Table 3: Reported pre-consultation diet and recommended post-consultation diet for Subject 2. View Table 3
Table 4: Reported pre-consultation diet and recommended post-consultation diet for Subject 3. View Table 4
Table 5: Reported pre-consultation diet and recommended post-consultation diet for Subject 4. View Table 5
Table 6: Reported pre-consultation diet and recommended post-consultation diet for Subject 5. View Table 6
The MNI and its subscales correctly marked the improved nutrient value of the recommended diets by a certified dietician compared to the pre-consultation diets, demonstrating it's internal and construct validity as well as its sensitivity to change. The indices changed in the expected direction after post-consultation and provided a clearer picture of the personalized recommendations made by the dietitian for each patient. Figure 1 reflects changes in overall index and subscales from baseline to post-consultation.
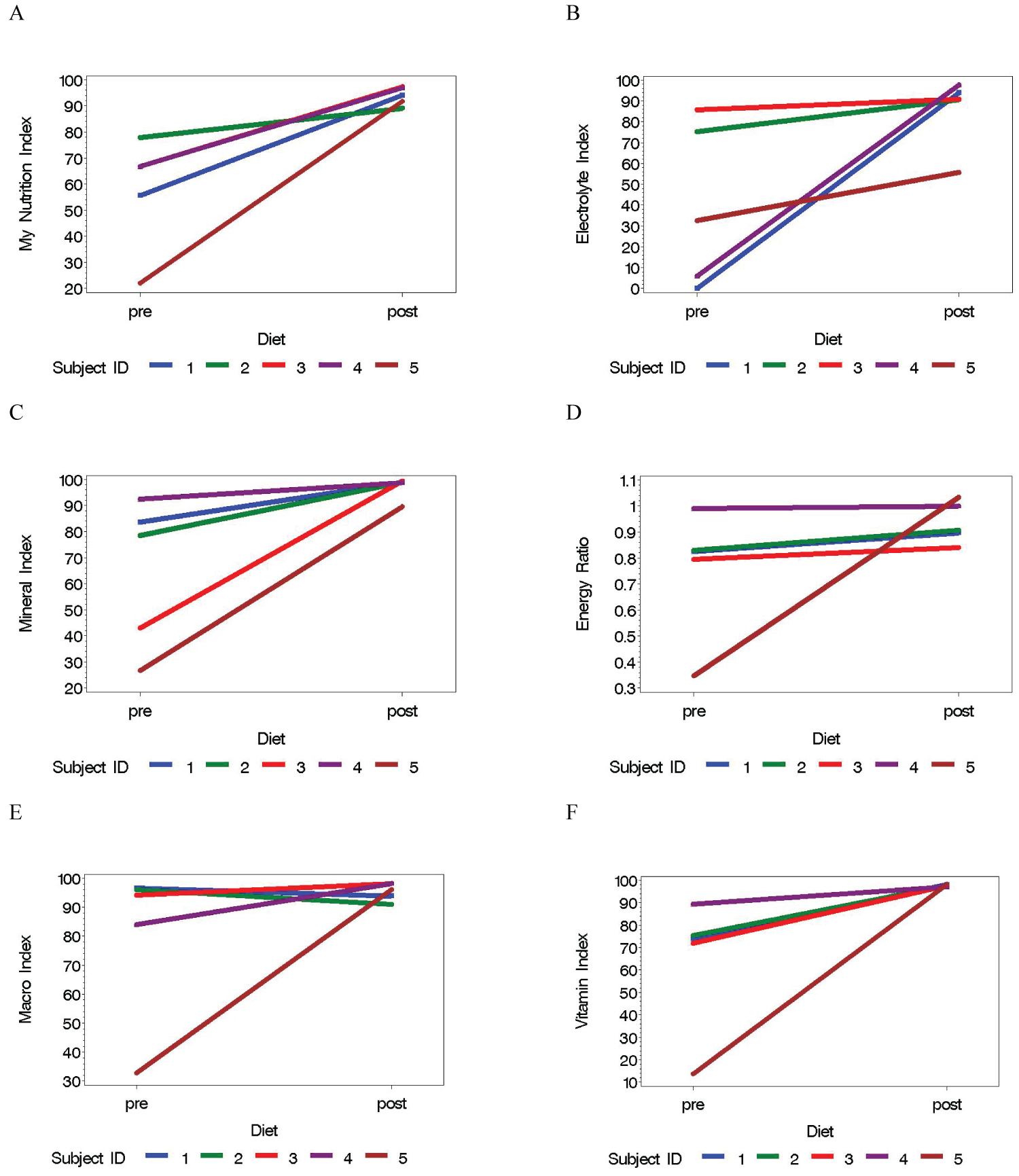 Figure 1: Dietary indices from pre- and post-assessment diets for the five subjects: A) My Nutrition Index; B) Electrolyte Index; C) Mineral Index; D) Energy Ratio; E) Macro Index; and F) Vitamin Index.
View Figure 1
Figure 1: Dietary indices from pre- and post-assessment diets for the five subjects: A) My Nutrition Index; B) Electrolyte Index; C) Mineral Index; D) Energy Ratio; E) Macro Index; and F) Vitamin Index.
View Figure 1
The average pre-consultation MNI was 58 and ranged between 22 and 78 (Figure 1A), compared to the post-consultation MNI averaged at 94 (range: 89 to 97). The macro nutrients were all in adequate ranges in the post-consultation diets (Figure 1E) with all five diets boasting at least 84% of targeted calories (Figure 1D). Three of five (60%) patients had pre-consultation diets with inadequate electrolytes, which were improved to guideline values in four of the five (80%) patients. The vitamin and mineral indices (Figures 1C and Figure 1F) were all improved to guideline levels for each component for all patients with the exception of one patient who had slightly reduced minerals.
We have demonstrated that the MNI and subscales correctly measure the improved nutrient value of the recommended diets for IBD patients, as evaluated by a registered dietitian. This is important given the heterogeneous nature of Crohn's Disease as well as the complexity of patient disease and personal characteristics influencing decision-making.
Limitations include a small sample in a tertiary academic medical center so patients may be more complex than those seen in the IBD community at large. For this study we did not evaluate how adherent the patients were to using the recommended diet. Further, the dietitian balances changing a diet for nutrition and for adherence-with the plan that overtime, the recommendations could be further improved with minimally processed food, less red meat, less saturated fats and more fresh fruits and vegetables in tolerated forms.
The MNI tool, while not a substitute for dietitian advice, can inform both patients and their nutrition providers with numeric feedback around the nutritional value of their diet and appreciate small, customized, incremental changes to reach their goals. Further the tool could be used as a way to characterize patient nutritional value in the setting of clinical research.
LK is a consultant to Pfizer and Abbvie, has a research grant from Abbvie and is a co-founder and equity shareholder for Trellus Health, Inc.CG is partially supported by the Mindich Child Health and Development Institute at the Icahn School of Medicine at Mount Sinai.
The authors have no conflict of interests to disclose.
CG and LK conceived of the study, LM collected the data, CG calculated the indices. CG and LK wrote the first draft with contributions from LM. All authors reviewed and commented on subsequent drafts of the manuscript.