Background: Ethiopia is one of the countries in sub-Saharan Africa that was most affected by the HIV epidemic. In response to HIV/AIDS, Ethiopia implemented the antiretroviral therapy program in an effort to preserve lives. However, the occurrence of first line ART failure has had an impact on the outstanding success documented in lowering morbidity and mortality. This study was designed to identify the incidence and predictors of first-line ART failure in selected public health facilities at Gullele sub city Addis Ababa, Ethiopia.
Methods: Facility based retrospective cohort study design was employed on archived data from 2017 to 2022. A data collection checklist was created using the intake card and the ART follow-up card. The collected data were entered through Epidata version 3.1 and analysed using SPSS version 25 software. Descriptive statistics, such as median and interquartile ranges (IQR) was used to compute continuous variables and counts with percentage for categorical variables. The survival experiences of the patients were assessed using the Kaplan-Meier survivor function. The log-rank test was used to compare the survival experiences among the different groups of subjects. Bi-variate and multiple Cox regression were used to determine the magnitude of treatment failure and identify factors significantly associated with the outcome variable analysis. Independent predictors associations were considered with p < 0.05. The incidence was measured with person-months of observation.
Results: 174 (54.9%) of the 317 participants, whose median age was 39 (IQR 32-45) years, were female. 60 (18.9%) people failed their first-line ART regimen during the 10,579 person-months of follow-up, at an incidence of 5.67 failures per 1000 person-months of observation, with a median time to failure of 17 months. The median survival duration was 37 months. Clients on ART for two years or less had high rates of treatment failure. Inadequate adherence (AHR=14.21 (95%CI: 6.341-31.87) and age less than or equal to 35 ((AHR) = 1.88, 95%CI (1.03-3.41)) were associated with an increased hazard rate for first-line ART failure.
Conclusion: This study shows treatment failure was high and occurs early during the treatment. Special counselling and follow up mechanism, during early treatment initiation and those patients were found the potential predictors of treatment failure, is important to identify early treatment failure.
ART, ART failure, Antiretroviral therapy, HIV, Survival analysis
ABC: Abacavir; AHR: Adjusted Hazard Ratio; AIDS: Acquired Immune Deficiency Syndrome; ART: Anti-Retroviral Treatment; ARV: Antiretroviral; ATV: Atazanavir; ATV/r: Atazanavir combined with ritonavir; AZT: Zidovudine; CHR: Crude Hazard Ratio; DM: Diabetes Mellitas; DRV: Darunavir; DTG: Dolutegravir; EFV: Efavirenz; FDC: Fixed Dose Combination; FMOH: Federal Ministry of Health; HAART: Highly Active Anti-Retroviral Therapy; HIV: Human Immune Deficiency Virus; HIVDR: HIV Drug Resistance; HTN: Hypertension; HVL: High Viral Load; LPV/r: Lopinavir combined with ritonavir; 3TC: Lamivudine; MRN: Medical Registered Number; NVP: Nevirapine; RAL: Raltegravir; RTV or /r: Ritonavir; TB: Tuberculosis; TDF: Tenofovir Disoproxil Fumarate; TF: Treatment Failure; TLD: Combination of Tenofovir, lamivudine and dolutegravir; UNAIDS: United Nations Program on HIV/AIDS; UNICEF: United Nations International Children’s Emergency Fund; VIF: Variance Inflation Factor; VL: Viral Load; WHO: World Health Origination
The AIDS pandemic has plagued the world for more than 35 years [1]. Since the invention of highly active antiretroviral medication, morbidity and mortality related to human immunodeficiency virus/acquired immunodeficiency syndrome have drastically decreased [2]. The expansion of treatment coverage for known patients at the earliest stages of illness has now become the focus of a global effort. Clinically, the benefits of HAART are manifested in lower morbidity and mortality. HIV illness management with HAART In a patient who has recently received a diagnosis, treatment should start right away. Upon seven days of an HIV diagnosis being confirmed, the World Health Organization has recommended that treatment be initiated quickly. Only patients who are ready and willing should receive HAART [3]. Worldwide, UNAIDS aimed to have 90% of those using HAART virally suppressed by 2030, preventing HIV treatment failure, to reduce morbidity and mortality. Initiating HAART in HIV patients has as its main objectives reducing HIV viral replication and regaining immunological function. Via routine viral load testing and/or CD4 cell counts, the clinical decision is made on whether such objectives have been met [4]. ART failure can be defined as progression of disease after initiation of ART. It occurs in the form of Virologic failure, immunologic failure, or clinical failure [5]. Treatment failure may have bad consequences for the individual patient and seriously threatens the initial success of combination therapy in the community, raising concerns about the selection and transmission of multi-resistant viruses [6]. Sub-Saharan Africa continues to be the area most impacted by HIV/AIDS today. There are currently over 38.4 million and 25.6 million HIV-positive people living in the world and sub-Saharan Africa, respectively. 75% of these people receive ART [6].
Ethiopia is one of the sub-Saharan African nations most afflicted by the HIV epidemic. The most recent Spectrum modelling estimated that in 2022, there were 612,925 HIV-positive peoples [7]. As a response to the HIV/AIDS, Ethiopia has introduced the Antiretroviral Treatment program to save lives [8]. Meanwhile still Ethiopia is challenged by ART failure. In patients receiving highly active antiretroviral therapy, treatment failure is a growing concern. Even while these regimens reduce morbidity and death, a sizeable minority of patients fail to show a sustained response to treatment [9]. If treatment failure is not detected early it can lead to minimize life expectancy and quality; to increase risk of drug resistance and Toxicity [10,11]. A rise in the number of HIV patients, which necessitates the need for more qualified medical staff; a rise in the level of poverty; a rise in the cost of health treatment; a rise in the cost of paying for burial services; a rise in the amount of responsibility placed on children or orphans living in decreasing school enrollment due to financial hardship, declining fertility and birth rate, a decline in the skilled labor force, and economic and social growth (Age 15 to 49 is most affected) [6]. For the timely detection of treatment failures, the identification of patients needing more intensive adherence support, minimize the development of drug resistance and unnecessary switching to expensive and constrained ART regimen options [12]. Failure rates to first-line ART may vary region wise and need not be uniform all over the country due to various identified reasons [13]. Patients unnecessarily remained in failed regimen experienced higher morbidity and mortality, and failed regimen might threaten successful ART program [14]. First-line ART treatment has a high failure rate, according to numerous studies. [12,15], Studies in East Africa have shown a high prevalence of immunologic failure ranging from 8% to 38% among clients on first-line HAART, and furthermore, the magnitude increases as the time of follow-up increases [12]. In Ethiopia conducted shows the prevalence of ART treatment failure is ranges from 4.9% to 22.7% [16-18]. Treatment failure was found to be 19.8% with incidence rate of 8.46 failures per 1000 person-months [19]. In Ethiopia, different report shows low achievement on treatment failure monitoring [17]. In settings with limited resources, managing first-line ART failure is a major concern for HIV programs [20]. The national ART program must be guided by information on population-level estimations of TF (virologic, immunologic, and clinical outcome) in order to achieve good treatment outcomes. Determining the incidence of TF and identifying the associated risk factor of TF is of paramount importance to achieve a high treatment success rate and improve the quality of life of people living with HIV [21]. However, there is little data on the prevalence of TF and its causes among HIV-infected individuals on ART in Ethiopia [1]. In this study, treatment failure among adult patients receiving first-line highly active antiretroviral therapy in Gullele Sub City, Addis Ababa, was evaluated along with its incidence and determinants.
The study conducted in Gullele sub city which is one of the eleventh sub cities in Addis Ababa, the capital city of Ethiopia. Thirteen health facilities, including 11 health centers and 2 hospitals, provide ART services. According to Gullele sub city health office 2022 people living with HIV report 11,224 people are on ART. The procedure of enrollment in chronic HIV care was that patients who tested positive for HIV at different service outlets were enrolled in HIV care and registered on HIV positive tracking. The preferred first-line regimens and the medical eligibility requirements for the start of ART were in accordance with the national recommendation.
A facility based retrospective follow-up study design using secondary data was used. The study was conducted at randomly selected ART providing health facilities in Gullele sub city, Addis Ababa Ethiopia, from June 1 to 30, 2023. Out of the total 1643 people living with HIV (PLHIV) who were put on treatment at the time of the study, 1501 of them were adults above and equal to 15 years of age. Adult patients who were taking ART during the study period and who are >= 15-years-old and who had been on first-line ART for greater than or equal to 6 months. The records of all HIV-positive adults who were taking ART for more than 6 months from the facility they started the treatment between November 2017 to October 2022 were included in the study.
The dependent variable was clinical, immunological failure and/or virological failure among HIV-positive adults on the first-line ART 6 months after ART initiation.
Clinical failure: New or recurrent WHO stage 4 condition OR new or recurrent WHO stage 3 with pulmonary TB and/or severe bacterial infections after 6 months of optimal adherence to appropriate ART regimen [22].
Virologic failure: Viral load above 1000 copies/ml based on two consecutive viral load measurements 3 months apart with enhanced adherence support [23].
Immunological failure: Fall ofCD4 count to baseline (or below) OR 50% fall from on- treatment peak value OR Persistent CD4 levels below 100 cells/mm 3 [22].
Viral suppression: Plasma viral load below 1000 copies/ml based on one viral load Measurement [23].
Adherence: No of dose of HAART taken/No of prescribed doses of HAART * 100% Good adherence, > 95%, fair adherence, 85-95% and poor adherence, < 85% doses take [24].
The independent variables were Socio-demographic factors such as age, gender, occupational status, marital status, educational status and educational level. Clinical factors -months since diagnosis, Baseline CD4 count, TB-confection, WHO stage, functional status, Presence of OI, baseline BMI and history of side effect during follow. Medical follow up factors - Adherence, follow up appointment, Disclosure status, ART regimen and Duration of treatment.
The sample size was calculated based on proportional Cox hazard model considering the magnitude of treatment failure was 21.5% [25]. Among the different factors, Base line CD4 count between 0 and 349 yields the maximum sample size, with an AHR of 2.673. The proportion of patients with baseline CD4 count 0-349 cells/mm 3 (exposed group) was 31.2% and proportion of patients with base line CD4 count 350 cell/mm 3 to 999 cell/mm 3 (non-exposed group) was 7%; and 95% CI, power of 80%, AHR of 2.673, ratio of one to one, and 10% non-response rate considering for compensation of incomplete records. The final sample size calculated was 317. Based on this sample size, selected health facilities providing ART service were included, and the sample size was proportionally allocated to each facility based on the patient load the health facilities had. The sampling frame was that the list of all patient records in the specified period was obtained from the patient registers and electronic databases in selected the health facilities. The sample size was proportionally allocated and was used systematic random sampling method to obtain the samples.
Pretested and structured data extraction tool was used to collect the data. Pretesting of the data extraction tool was conducted on 5% of the sample size in a health center outside the study area. A data extraction form was developed from the ART follow-up form of the federal ministry of health (FMOH) [23]. The data were collected by 4 data collectors who had a minimum diploma in information and communication technology (ICT). After obtaining permission from the medical directors, data collectors were review and extracted data from patient medical records, electronic database and registries used a check list by their medical registration/card numbers. Before data collection, the data collectors and supervisor were get a one day orientation by principal investigators to be known ART data management and familiar with all the information in the data extraction instrument. There were two supervisors involved with responsibility to check completed questionnaires for consistency and completeness daily and before entry by the principal investigator. The required data was collected by considering carefully all the variables stated in the tool with due attention to avoid any redundancy of the study participants. Finally, data was analysed using SPSS after employing appropriate statistical treatment following proper entry and cleaning.
The extracted data were entered through Epidata version 3.1 and exported to Spss version 25 for cleaning and analysis. Descriptive statistics, such as median and interquartile ranges (IQR) was used to compute continuous variables and counts with percentage for categorical variables. The survival experiences of the patients were assessed using the Kaplan-Meier survivor function. The survival experiences of the various subject groups were compared using the log-rank test. Bi-variable Cox proportional hazard regression was fitted to select potential candidate predictors to the full model with cut-off point P ≤ 0.25. The Cox PH model was done to identify the independent effect of predictors on the occurrences of treatment failure. The multi-collinearity for variables in the final fitted model were checked using variance inflation factor (VIF) with cut-off point mean VIF > 10. Association between predictors and hazard of treatment failure was summarized using adjusted hazard ratio (AHR), and statistical significances will be tested at P < 0.05. The incidence was measured with person-months of observation. Ethical clearance was obtained from the Institutional Research Ethics Review Committee of Rift Valley University health science department and from institutional review committee of selected hospitals (St. Paul's Hospital Millennium Medical College and St. Peter specialized hospital). Then, permission was also obtained from the administrative bodies of each hospital to access the ART client’s database and charts. In order to ensure confidentiality, the identity of the person was not recorded, and only relevant parties, such as the primary investigator, were allowed access to the data.
A total of 317 eligible participants with median age of 39 (IQR 32-45) were enrolled into the study. Above half of the participants (54.9%, n = 174) were female, all most third fourth (67.8%) were unemployed, nearly half of (46.7%) were married and 39.7% reported as their educational level is primary education (Table 1).
Table 1: Socio-demographic factors of the study participants. View Table 1
About one third, 95 (30%) of the study participants were categorized to WHO clinical stage 3 and the median CD4 cell count was 208cells (IQR 114-283), and the median BMI was 21(18.7-22.6). more than three-fourths, 305 (96.2%) of participants started ART initiation less than 12 months after know their status, during follow up most of participants experienced opportunistic infection 196 (61.8%), and nearly one-third 79 (24.9%) were with TB-co-infection. Most, 224 (70.7%) of the working functional status while one third, 76 (24%) of participants functional status were ambulatory when they start ART (Table 2).
Table 2: Distribution of clinical and immunological characteristics of study participants. View Table 2
One hundred eighty one (57.1%) of study participants were found on TDF-3TC-DTG regimen during ART initiation, nearly half of participants were on AZT-3TC-EFV and the majority, 215 (67.8%) of them had good ART adhere during their last follow-up period. Nearly Half (52.4%) of the study participants disclosed their status. Among the study participants, 157 (49.5%) were found on three to five months follow-up status. The median ART clinic follow up period of participants was 37 months (IQR 17-48) months with minimum 6 months and maximum 65 months of follow-up. The majority, 281 (88.6%) of study participants were on ART follow-up at the time of the study, 17 (5.4%) were reported as lost, 2 (0.6%) dead, 4 (1.3%) drop, and 13 (4.1%) were transferred out (Table 3).
Table 3: Medical follow up history of participants. View Table 3
Treatment failure among adults living with HIV on first line antiretroviral therapy by socio-demographic, Clinical, immunological and Medical follow up history of participants : The overall treatment failure among adults on first line ART was 18.9%. From this 7.6% immunological failure, 5.7% clinical failure, 3.2% virological failure and 2.5% mixed treatment failure experienced. 23% of them switched to second line regimen. the treatment failure was higher among female, BMI <= 18.5, unemployed, married, primary education, WHO Clinical stage 3 ,working functional status, age (25-34), presence of opportunistic infections, No TB co-infection, start of ARV since know status < 2 years, follow up status (3-5 months) and with less than 200 CD4 count and those who were on ART for less than 2 years. Treatment failure was higher among those with poor adherence and not disclosed, however patients on regimen TDF-3TC-DTG and TDF-3TC-EFV have nearly equal magnitude of treatment failure (Table 4).
Table 4: Treatment failure among adults living with HIV on first line antiretroviral therapy by socio-demographic, clinical, immunological and medical follow up characteristics. View Table 4
Incidence of treatment failure
Incidence of treatment failure : All study participants (317) who were followed for different periods in 5 years, a minimum of 6 months and a maximum of 65 months. The median survival time was 37 months with 10579 person-months follow up time. Sixty, 18.9% participants experienced treatment failure. The overall incidence rate 5.67 failures per 1000 person-months of observations. Of this, 0.9, 1.7 and 2.26 incidence rate per 1000 person-months of the adults have experienced a Virologic, clinical and Immunologic failure respectively. Generally, majority of clients on first line antiretroviral.
Treatment failed at median time of 17 months. The high rates of treatment failure was high among adult’s clients on first line ART for less than two years compared to those who were on ART for more than two years (log rank test, p < 0.0001) (Figure 1).
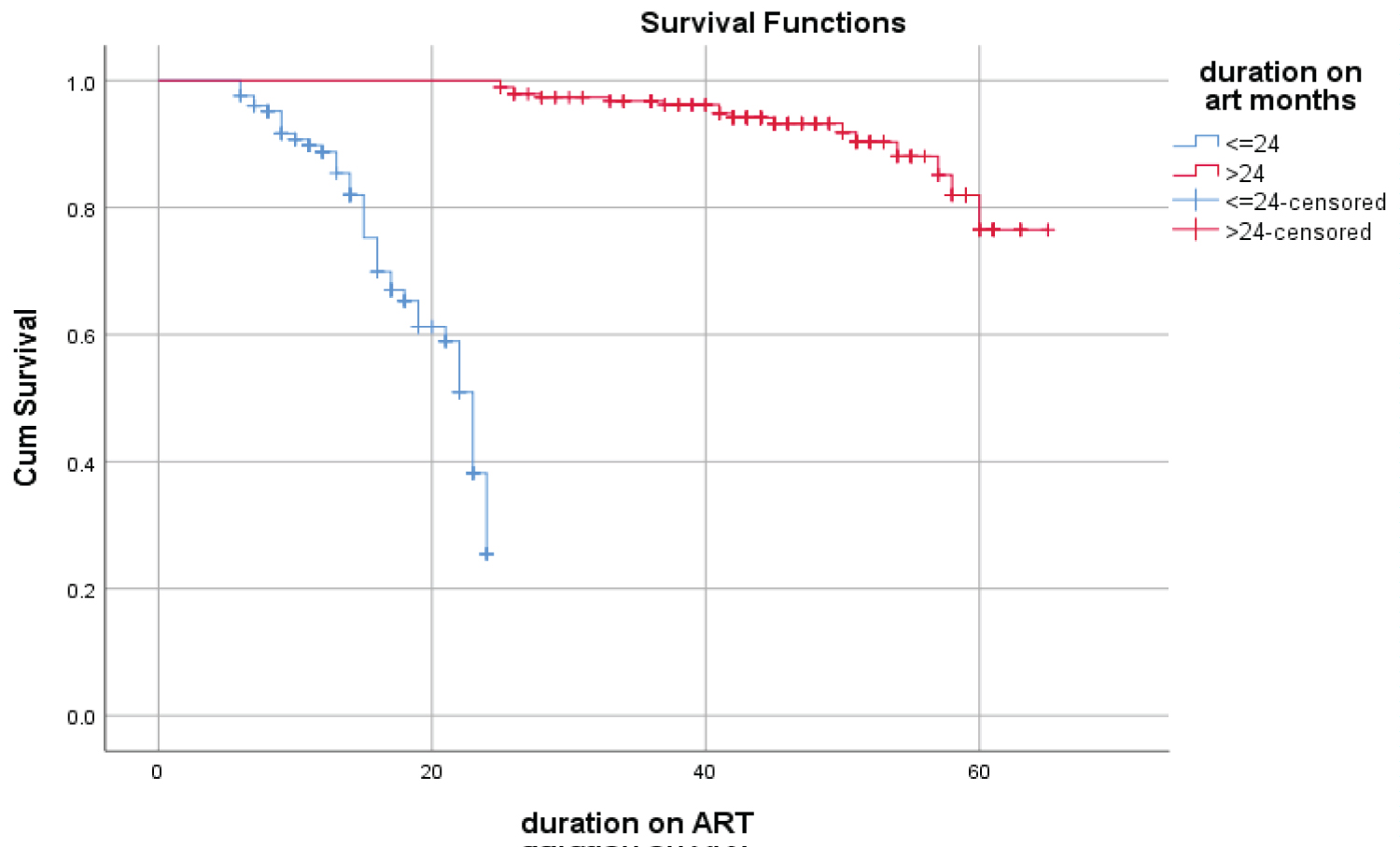 Figure 1: Median time to failure among adults living with HIV/AIDS on first line antiretroviral therapy by numbers of years on ART.
View Figure 1
Figure 1: Median time to failure among adults living with HIV/AIDS on first line antiretroviral therapy by numbers of years on ART.
View Figure 1
C4.7 bivariate Predictors of first line ART treatment failure among adults living with HIV/AIDS: Bivariate analysis of predictors of first line ART treatment failure among adults living with HIV/AIDS is presented in Table 5. The incidence of developing treatment failure was two times higher among patients of age less and equal to 35 as compared to those age greater than 35 years with hazard ratio [(HR) = 2.60, 95%CI (1.57-4.32)]. Two (HR=2.40, 95%CI = 1.31-4.41) times higher among clients on ART for never married compared to those who were on ART for married. participants who had Low baseline BMI (<= 18.5) has about two times higher risk (HR, 1.99, 95%CI: 1.12-3.23) of failure as compared to those who have BMI (> 18.5). When compared to those who started at WHO stages 1 or 2, those who started ART at stages 3 or 4 had 2.33 (HR = 2.33; 95% CI = 1.39-3.92) times greater risks of treatment failure. Patients who have any opportunistic infection, other than tuberculosis, are at higher risk of treatment failure than those who do not (HR: 1.89; 95% CI (1.07-3.32). participants who had TB had a two-fold greater chance of failure (HR, 2.55, 95% CI: 1.53-4.25) than those who did not have the co-infection. The incidence of developing treatment failure was about seventeen times higher among patients those had inadequate adherence as compared to those had good adherence [HR = 17.83, 95%CI (8.45-37.60)]. Moreover, participants who had follow up less than 6 months experienced high as compared to those had six months follow up with crude hazard ratio [(HR) = 3.62, 95%CI (1.83-7.16)]. However, this estimate had a borderline significance at 5% level clinical characteristics associated with failure.
Table 5: Bivariate independent predictors of ART treatment failure among the client first line ART. View Table 5
Multivariate cox regression independent predictors of ART treatment failure among the clients on first line ART : During bivariate cox-proportional hazard analysis age, marital status, BMI, WHO stage, presence of opportunistic infection, TB-co-infection, adherence and follow-up status had a p-value of ≤ 0.25; hence, they were candidates for the multivariable model. However, sex, occupation, educational status, functional status, regimen at iniation,disclosure,cd4 count at enrollment and months since diagnosis were demonstrated p-values of > 0.25; therefore, they were excluded from the multivariable analysis. After controlling all potential confounders in multivariable Cox proportional regression, age <= 35 and inadequate adherence were independent predictors of first-line ART failure. The risk was two times higher among patients of age less than and equal to 35 as compared to those greater than 35 years with adjusted hazard ratio [(AHR) = 1.88, 95%CI (1.03-3.41)] and The Hazard of developing treatment failure was 14.21 (AHR = 14.21, 95%CI = 6.34-31.87) times higher among client’s inadequate adherence compared to those who had good adherence (Table 6).
Table 6: Multivariate cox regression modelling of independent predictors of ART treatment failure among the clients on first line ART. View Table 6
In countries with low resources, like Ethiopia, managing first line ART failure is a major concern for HIV/AIDS programs. The revised UNAIDS targets for HIV diagnosis, ART initiation and viral suppression denoted as 95/95/95 respectively were endorsed by many countries including Ethiopia and these targets were aligned with the of HIV diagnosis and treatment program goals. As a result, this research sought to identify the prevalence of first-line ART treatment failure and related factors. The overall incidence treatment failure among patient initiated ART during this study was 5.67 per 1000 person months at risk which is closer to previous study done in low- and middle-income countries including Tanzania and Ethiopia demonstrated 5.24 and 4.91 rate of antiretroviral failure per 100 person years among clients on ART (25.5). Higher incidence of ART failure was reported from Ethiopia (9.38 per 1000 person years) [26]. Other studies from Ethiopia (0.78 per 1000 person months) and Sub-Saharan Africa (1.33 per 1000 person months) documented lower incidence of ART failure [5,27]. Reasons for varied results could be explained by differences in ART initiation criteria, ART regimen used, and definition of ART failure and period of follow-up. According to this study, the incidence of immunological, clinical, and virological failure is 2.26, 1.7, and 0.9 per 1000 person months of follow-up, respectively. Despite these drawbacks, immunologic and clinical failures were discussed to have low sensitivity and specificity. As a result, HIV viral load testing has gained importance in recent years, suggesting the relevance of diagnosing failure using viral load determination technique to obtain better yield of patients' status. In order to confirm real treatment failure, make the best changeover, and prevent misclassification, viral load testing must also be performed in addition to clinical assessments of improvement [5]. The study found that the majority of the clients on first line ART failed at the median time of 17 months. High probability of ART treatment failure was reported among clients on ART for two years and less. This finding was consistence with the study done in South Africa, Haiti and which showed ART median time to failure of 12 and 16 months respectively [28,29], this might be due to treatment related factors which includes side effects, use of unfavorable taste brand, and missing opportunity for counselling due to shortage of staffs. But it has been below the study done in Cameroon and Northern Ethiopia and Senegal study which shows 23, 24 and 28 respectively [27,30,14]. A recent analysis of patients from seven countries in Africa and Asia indicates a modest rate of 11% at 12 months and 12% at 24 months of ART. The median survival time was 36 months study conducted in Tigray, despite the fact that the mean survival time (the predicted time to event) in the current study was 37 months [17]. The difference may be due to the health care practices and care that is provided. Even though the binary cox regression showed many variables to have significant predictors of ART failure, multivariate cox regression indicates that only age less than and equal to 35 and inadequate adherence were found significant predictors of ART failure. The hazard of developing treatment failure among patients age less than and equal to 35 years was [(AHR) = 1.88, 95%CI (1.03-3.41) higher compared to age older than 35 years. This study is consistent to the study conducted in Myanmar, Tigray, Gondar, Uganda, Mozambique, Australia and Latin America, [29,17,31-35] where younger patients had a higher risk of treatment failure. This might be due to their vulnerability to emotional instability with depression and the differences in the medical attention given to the patients with advanced age, which leads to poor adherence resulting in poor treatment outcomes [36]. Inadequate adherence was found to be predictor of treatment failure (AHR = 14.21 (95% CI: 6.34-31.87)), Higher among clients who had inadequate adherence compared to those who had good adherence. This finding was consistent with studies conducted in Ethiopia (AHR (95% CI: 1.86-19.80) = 5.68)), Kenya (AHR (95% CI: 2.20-3.49) = 2.77)) South Africa (AHR (95% CI: 2.13-2.91) = 2.49)) and Uganda (AHR (95% CI: 2.3-11.05) = 5.05)) [26,28,37-39]. Actually, the main concern for ART users is adherence. It is undeniable that those who miss three ART doses per month have lower rates of sustained HIV suppression, medication resistance, and treatment failure. Presences of opportunistic infections, who clinical staging, cd4, tb confection were not found to be predictors of ART failure, unlike reports from another studies Ethiopia and sub-Sahara Africa [21, 40, 28, 14, 38,39, 41,9,42,43].
The study limitation was missing information, loss to follow up and use of secondary data, which restrict the number of variables that would be studied such as side effect and differences in quality of care and service in each hospital.
The rate of treatment failure was high in this population and occurs early during the treatment. Age under 35 and adherence were found the independent predictors of treatment failure. One of the most important areas for improvement for healthcare professionals is the early detection of antiretroviral therapy failure. This is done by closely monitoring ART patients and identifying the predictors of failure.
Our Special thanks go to the study participants for their willingness to participate and data collectors .Also we want to thank Department of public health Rift Valley University for giving me this chance to conduct We want to express our grateful thanks to Saint Paul’s Hospital Millennium Medical College and St. Peter Specialized hospital administrative for the cooperation in permitting data access.
File S2 Contains table of characteristics of chewers.
MWS conceived, designed, and performed the study. TTN Critically Review the manuscript. All authors read and approved the final manuscript.
This research is financially supported by authors.
All the data (SPSS) sets generated and/or analysed in this study are available from the corresponding author on reasonable request.
Ethical clearance was obtained from the Institutional Research Ethics Review Committee of Rift Valley University health science department and from institutional review committee of selected hospitals (St. Paul's Hospital Millennium Medical College and St. Peter specialized hospital). Then, permission was also obtained from the administrative bodies of each hospital to access the ART client’s database and charts. Confidentiality was also maintained by not recording the identity that describes the individual and limiting the access of the data only for concerned bodies like principal investigator.
Not applicable.
The authors report no conflict interest in this work.