Antisynthetase syndrome (AS) is a rare autoimmune condition characterized by fever, Raynaud's phenomenon, hyperkeratosis, inflammatory polyarthritis, and interstitial lung disease (ILD). The development of ILD in patients with antisynthetase syndrome (AS-ILD) portends a poor prognosis to an already rare and difficult to diagnose autoimmune disorder.
We present the case of a 67-year-old Caucasian male who initially presented for evaluation of an abnormal chest radiograph, taken a few weeks after he had been treated for pneumonia. A high-resolution chest-CT was concerning for a pattern of Non-Specific Interstitial Pneumonitis, or NSIP, and although without any musculoskeletal complaints at the time, his anti-nuclear antigen titer was quite high. He then developed symptoms and titers consistent with antisynthetase syndrome, and steroids were needed. Despite the addition of an immunosuppressive drug, steroids could not be discontinued due to the severity of his symptoms, and further immunosuppression was considered imprudent due to a history of melanoma. Intravenous immunoglobulin (IVIg) therapy was initiated, with good results, and continued as maintenance therapy. Since commencing IVIg therapy, his ILD has also not progressed.
The literature pertaining to treatment of AS-ILD is quite limited, and there are no large trials that have examined the use of IVIg for maintenance therapy. There is a growing body of literature that suggests it may be useful, as it has been described by various authors who used it for induction of remission. This is a unique case where we continued to use IVIg while reducing his immunosuppressive medications and have had success in control both the musculoskeletal and pulmonary pathological processes for over a year.
Antisynthetase syndrome (AS) is a rare autoimmune condition characterized by fever, Raynaud's phenomenon, hyperkeratosis, inflammatory polyarthritis, and interstitial lung disease (ILD). The development of ILD in patients with antisynthetase syndrome (AS-ILD) portends a poor prognosis to an already rare and difficult to diagnose autoimmune disorder.
The use of intravenous immunoglobulins in treating antisynthetase syndrome is limited to case reports, showcasing patients in whom it was used either acutely in the hospital [1], or when the clinician's hand was forced due to side-effects or infection. There is a growing body of evidence proving its utility in improving myositis, dermatological and neurological complications associated with DM/PM, but it is yet unproven for treatment of the deadliest complication-ILD [2,3]. Furthermore, there are only a few case reports of using IVIg in the early stage of disease [4].
This report adds to a limited body of literature on the use of IVIg as an initial steroid sparing agent in the outpatient setting for AS-ILD and myositis.
A 67-year-old Caucasian male was seen for an abnormal CT scan, concerning for interstitial lung disease (ILD) in April 2019. He had been treated twice for bacterial pneumonia recently, but had persistent infiltrates on chest x-ray while undergoing preoperative workup.
At the time of initial evaluation, he had normal vital signs (BP 150/94, HR 64, Oxygen saturation 98% on room-air) and was afebrile.
He did not complain of cough, rash, dry eyes, muscle or joint aches at the time, but a screening panel for connective-tissue disease (CTD) was strongly positive for ANA, (1: 5120), and the myositis panel was positive for anti-Ku antibodies. His CT scan raised suspicion for fibrosing nonspecific interstitial pneumonia (NSIP) and surgical lung biopsy was recommended. He declined, on account of feeling asymptomatic. However, he soon developed dry eyes, complained of polyarthralgia, as well as weakness in his lower extremities. With rising creatine kinase (CK) levels, he agreed to a biopsy of his left biceps femoris muscle.
Despite an undiagnostic biopsy, his constellation of symptoms, CT-scan findings, and antibody titers, it was established that he has antisynthetase syndrome.
Soon thereafter, he developed a dry cough and became dyspneic, and high-dose prednisone was started. There was immediate improvement, and mycophenolate was added as a second agent but could not be used more than 500 mg a day due to GI side effects. Prednisone dose could not be lowered to less than 20 mg as the myalgias and arthralgia as would become unbearable.
After a lengthy delay due to problems with obtaining insurance approval, IVIg was started in April 2021 at a dose of 2 gm/kg of actual body weight, and he had the greatest degree of symptomatic improvement three days later. The effect initially lasted for 3 weeks, but has been maintained with each subsequent round of monthly dosing for 4 weeks. Since addition of IVIg, his prednisone dose has been tapered down to 10mg, and his mycophenolate dose continues at 500 mg (Figure 1 and Figure 2).
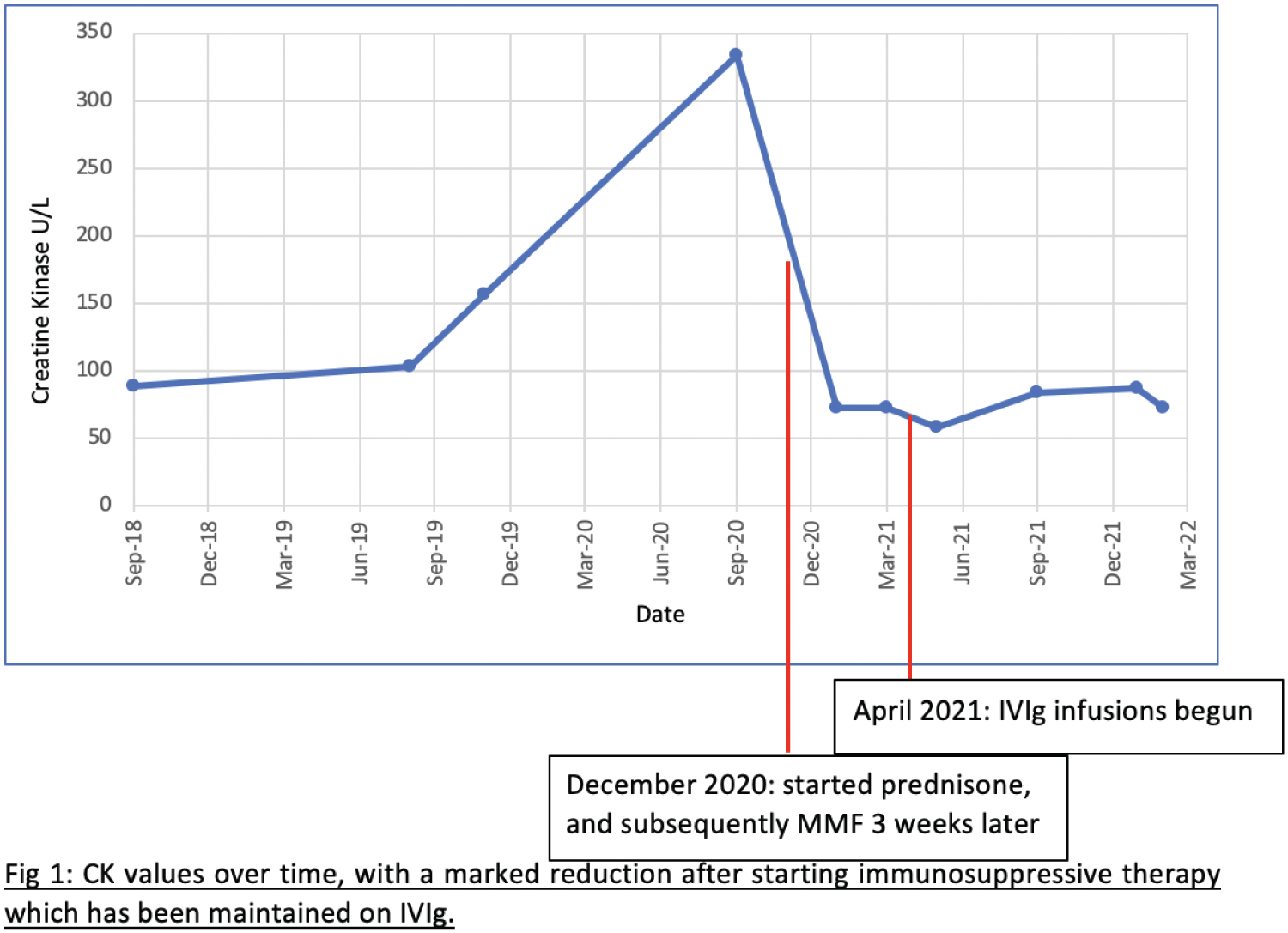 Figure 1: This is a graph depicting the creatine kinase (CK) levels over a period of nearly 4 years, pre-dating our first encounter
with the patient. The points of intervention with prednisone, mycophenolate mofetil (MMF), and IVIg have been marked. View Figure 1
Figure 1: This is a graph depicting the creatine kinase (CK) levels over a period of nearly 4 years, pre-dating our first encounter
with the patient. The points of intervention with prednisone, mycophenolate mofetil (MMF), and IVIg have been marked. View Figure 1
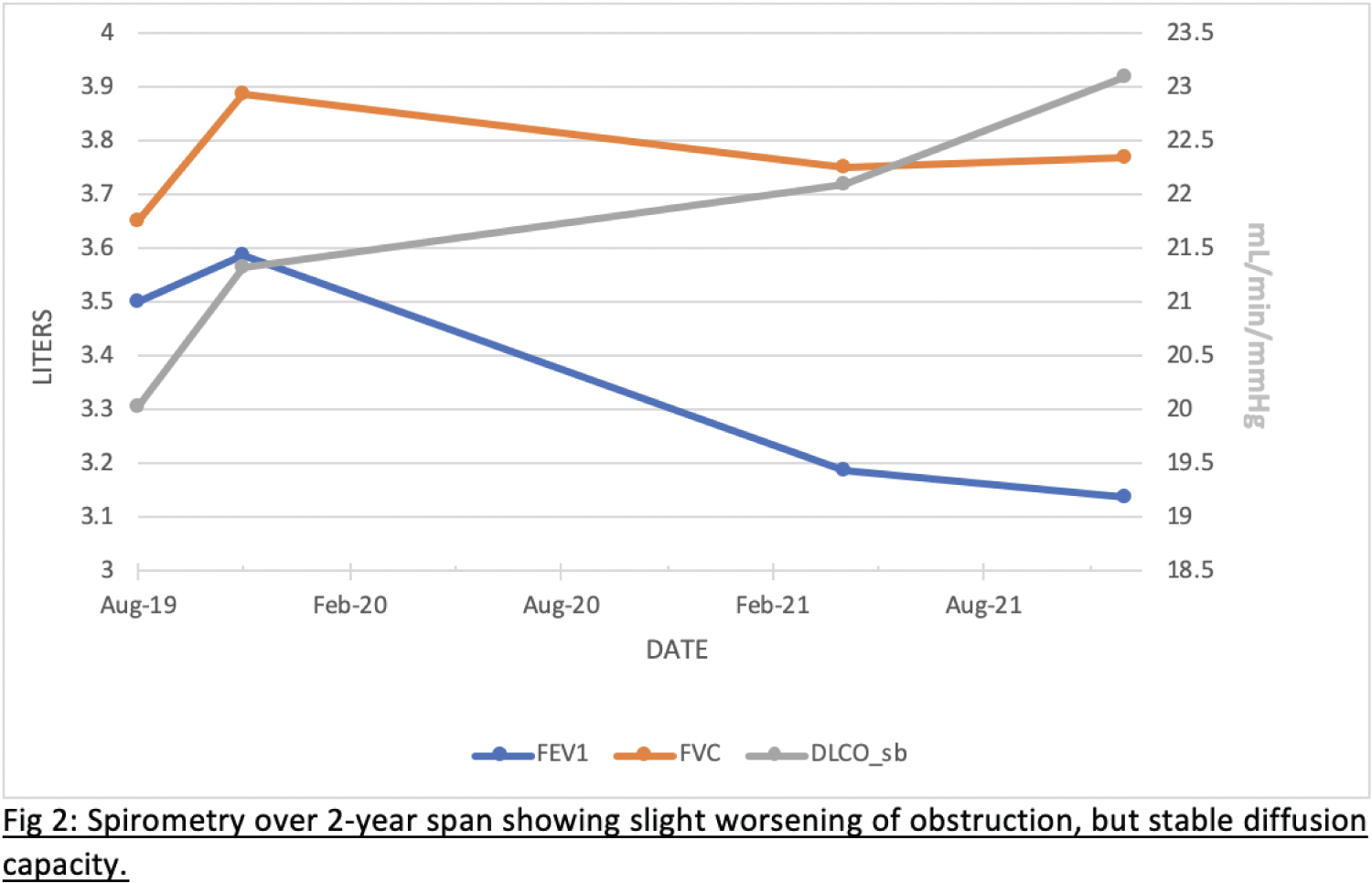 Figure 2: This graph connects 4 discrete data points obtained from pulmonary function testing (PFT) performed in the
office. View Figure 2
Figure 2: This graph connects 4 discrete data points obtained from pulmonary function testing (PFT) performed in the
office. View Figure 2
Axial images from a repeat CT in March 2022 are shown below, and show no progression in airspace disease. He has no current complaints of dyspnea or cough, and is able to do his daily activities and work without respiratory issues. There have been no hospital admissions or infections over this period. He has not had any known reported side-effects due to the IVIg transfusions (Figure 3).
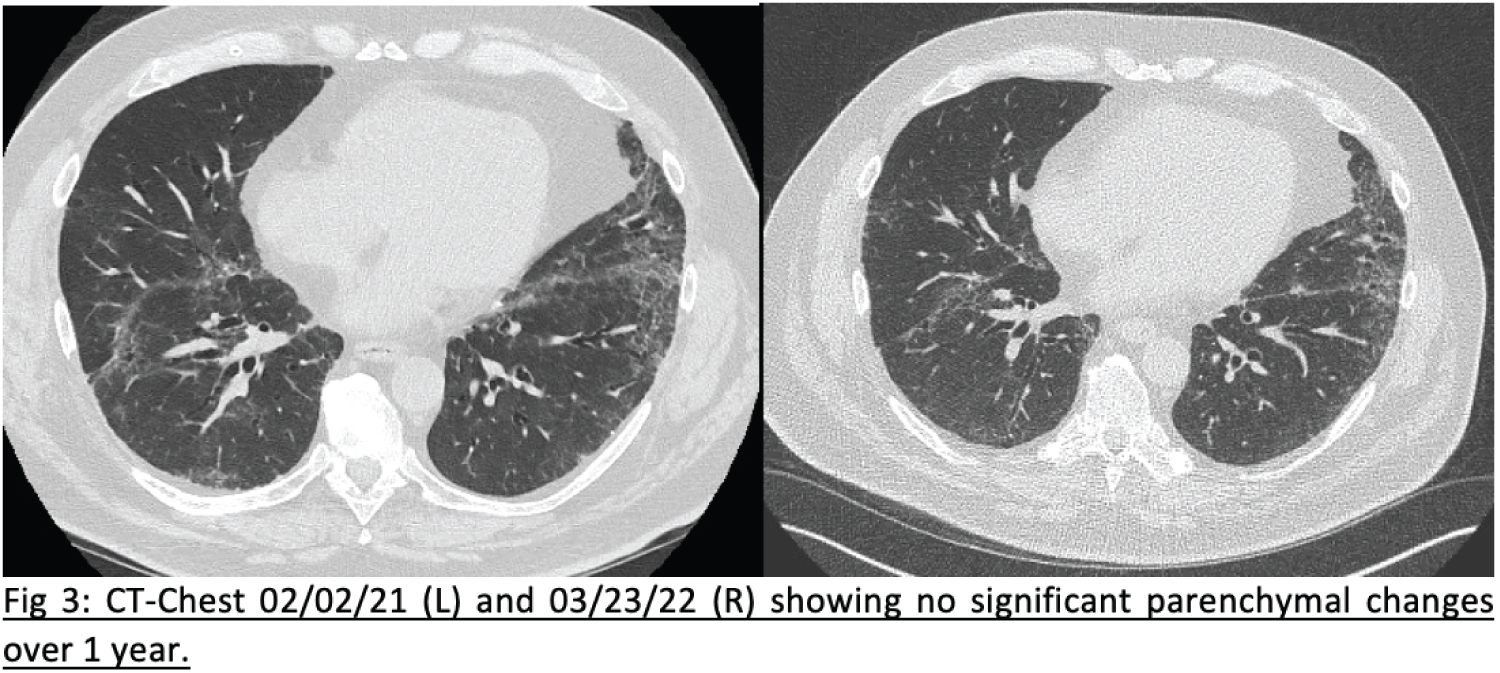 Figure 3: These are 2 cropped images of cuts at a similar location, from two 0.75 mm cut high-resolution CT-chest scans,
separated by 13 months. View Figure 3
Figure 3: These are 2 cropped images of cuts at a similar location, from two 0.75 mm cut high-resolution CT-chest scans,
separated by 13 months. View Figure 3
At present, the neuromuscular complications of antisynthetase syndrome are better understood, making the diagnosis and treatment simpler when those are the prevailing symptoms. Yet, interstitial lung disease can sometimes be the presenting symptom, appearing months prior to any other complaints, as seen in this case.
While steroids are the first-choice therapy for treatment of CTD-ILD, the addition of a second-line agent is usually required to achieve remission [5]. There are no randomized-controlled trials that have studied these therapies in patients with AS-ILD specifically. Although high quality evidence is lacking in general, drugs such as azathioprine, cyclophosphamide, mycophenolate and cyclosporine have an established pedigree in management of PM/DM-ILD.
In refractory cases where high-dose corticosteroids and two immunosuppressants do not control the disease, there is some evidence to support use of rituximab. In a case-series of 7 patients with refractory AS-ILD, one year after starting rituximab, all patients had improvement on PFTs or HRCT, and the median prednisone dose could be reduced from 20 mg/day at baseline to 9 mg/day (0.015) [6]. However, rituximab is associated with increased risk of infection and may also be associated with risk of melanoma [7].
The major consideration in our patient for avoiding rituximab is his history of melanoma, which had been treated successfully a few years prior. He also had recent recurrent pneumonia, and diverticulitis requiring surgery. IVIg is not known to cause immunosuppression, and should not increase the risk for infection, nor cancer. As IVIg does not carry an official indication for treatment of AS-ILD, there was a long delay in obtaining insurance approval and starting the infusions. Aside from small studies and case reports, IVIg is currently used as a treatment of ‘last resort' for AS-ILD, when the immunosuppressive agents fail.
Suzuki, et al. reported a case series of 5 patients who were treated with IVIg for refractory PM/DM-ILD, after high-dose corticosteroids and cyclosporine and/or cyclophosphamide did not achieve remission. 3 out of those 5 did not survive beyond 64 days, but in the 2 survivors, there was a notable improvement in PF ratios after IVIg [8].
Huapaya, et al. analyzed data from seventeen AS-ILD patients retrospectively, of whom 17 were treated with IVIg. They found that the mean percent-predicted forced vital capacity (FVC%) (p = 0.048), and percent-predicted diffusing capacity of the lung for carbon monoxide (DLCO%) (p = 0.0223) increased over time, while the mean prednisone dose (p < 0.001) decreased over time. However, 14 of those patients had also been on steroids and 2 immunosuppressive agents prior to initiation of IVIg, while 2 had been pre-treated with either MMF or azathioprine. The 1 patient who was started on IVIg concurrently with immunosuppression had only mild ILD [9].
Peshbahar & Bendstrup reported a case of an anti-Jo1-antibody positive polymyositis with OP/NSIP patient who received IVIg immediately after pulse-dose steroids. They were then maintained on a combination of low-dose prednisone, azathioprine and IVIg until their death, 4 years later [4]. The notable difference between our case and theirs, is that IVIg was first given as salvage therapy when the patient was admitted with acute hypoxemic respiratory failure.
In the outpatient setting, the lack of data showing benefit in preventing progression of lung disease, and higher cost of IVIg compared to immunosuppressing drugs means that it is rarely used. This is especially true when considering its use for maintenance, as opposed to just for achieving remission. However, in certain cases, IVIg may be the safer, more efficacious choice, and could prevent further morbidity by preventing long-term consequences from immunosuppression. Based on our case and the existing literature, there is a need for high-quality research investigating the use of IVIG for both induction and maintenance of remission of AS-ILD in the outpatient setting. In addition to improvement in dyspnea, we anticipate the benefits may also include lower mortality, reduced incidence of infection and reduced hospital admissions.
None.
Both authors contributed equally to this report.