We present successful management of an unusual foreign body (FB) case in the larynx for 20 days. A 45-year old man presented with complaints of hoarseness of voice and coughing up a few pieces of silver-colored flakes. He had unresolved dyspnoea and wheeze for three weeks and was managed as an asthmatic with partial resolution of symptoms. The patient was alcohol and drug dependent and was under treatment for epilepsy.
Fibre-optic laryngeal examination revealed a suspicious object in the Rima glottis. A blister pack measuring 2.6 cm × 2.2 cm was removed under GA. FB larynx is routinely associated with a definitive short history and the need for immediate resuscitation. However, the long period of persistence of FB in the larynx is possible depending upon the position of the FB. A history of aspiration may not be available in patient’s dependent on alcohol, drugs, and with epilepsy.
Foreign body larynx, SOB: Shortness of breath, Stridor, Choking, Dysphonia
Inhalation of a foreign body (FB) is a serious event. Many unfortunate individuals have lost their lives, have fallen victims to the presence of a FB in the airway [1], and such cases may go unpublished. It is exceptional for the FB to remain lodged in the larynx for weeks and remain undiagnosed. Failure to diagnose and remove it could result in a fatal accident anytime in a few minutes.
The patients usually present with a short history and symptoms of acute shortness of breath, drooling, choking sensation, or dysphonia. It can lead to a complete cessation of breathing & sudden death [2] unless retrieved in time. The foreign body can also present with non-life-threatening symptoms like chronic cough, haemoptysis, dyspnoea & wheezing [3]. There are many reports in the medical literature with a delayed diagnosis of the foreign body in the lower respiratory tract [4,5]. However, scarce medical literature is available with a delayed diagnosis of a foreign body in the larynx.
Numerous foreign bodies have been reported to block the larynx and the lower airway. The FB can vary from coins, metallic pins, food-bolus, dentures, small bones, live bees, etc. [6,7]. We present an unusual case where a large blister pack was retrieved from the larynx that had remained lodged for 20 days without causing complete airway obstruction.
A 45-year-old Caucasian man was referred to the ENT on-call team with features of sudden hoarseness of voice and coughing out a few pieces of silver-colored flakes. He was under the care of physicians for the past 20 days and was being treated for presumed asthma. His only complaints when admitted were shortness of breath and wheezing. He had received steroids, bronchodilators, and two courses of antibiotics. He had reported partial resolution of symptoms with these medications. His clinical records noted his dependence on alcohol and addiction to psychotropic drugs; He was also on anti-epileptic medicines.
Since the patient had fresh complaints of hoarseness of voice and cough with production of strange material, a Fiber-optic laryngeal examination under topical anesthesia was carried out. It confirmed the presence of a large translucent foreign body in the larynx (Figure 1).
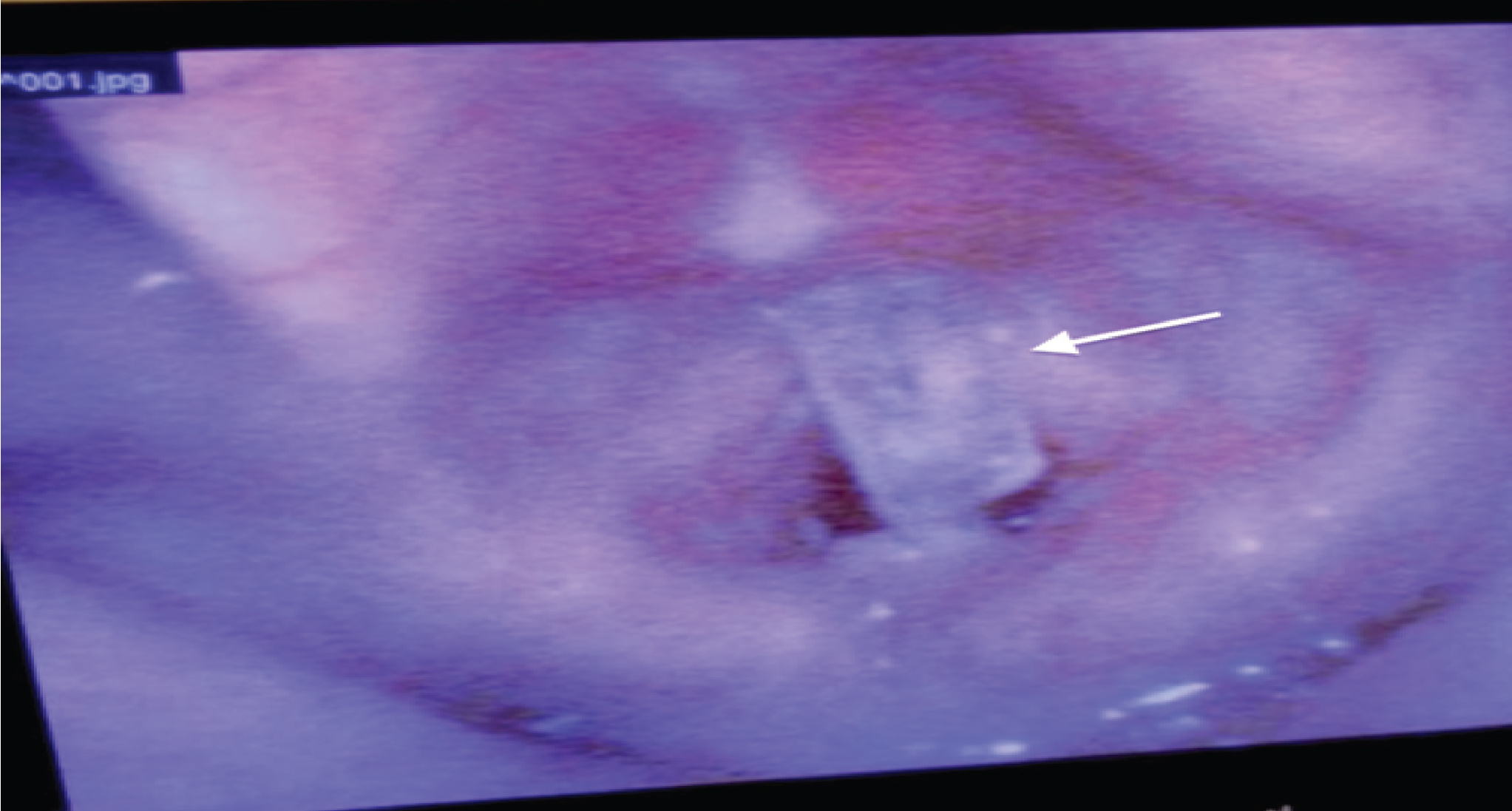 Figure 1: Foreign body as seen in the larynx before removal. The character of the foreign body is unknown. View Figure 1
Figure 1: Foreign body as seen in the larynx before removal. The character of the foreign body is unknown. View Figure 1
Further management plans were discussed with the anesthesia team, and informed consent was obtained from the patient. An escalation plan to deal with any eventuality of airway resuscitation was discussed and documented. This included readiness for performing cricothyroidotomy, tracheostomy, and rigid bronchoscopy.
Using McGrath video laryngoscope and Magill’s forceps, an empty blister pack measuring 2.6 cm × 2.2 cm (Figure 2, Figure 3 and Figure 4) filled with the mucopurulent discharge was removed from the endolarynx. The procedure was uneventful, and the patient was discharged home the next day with complete resolution of symptoms. Follow-up fiber-optic examination at three months revealed a normal larynx (Figure 5).
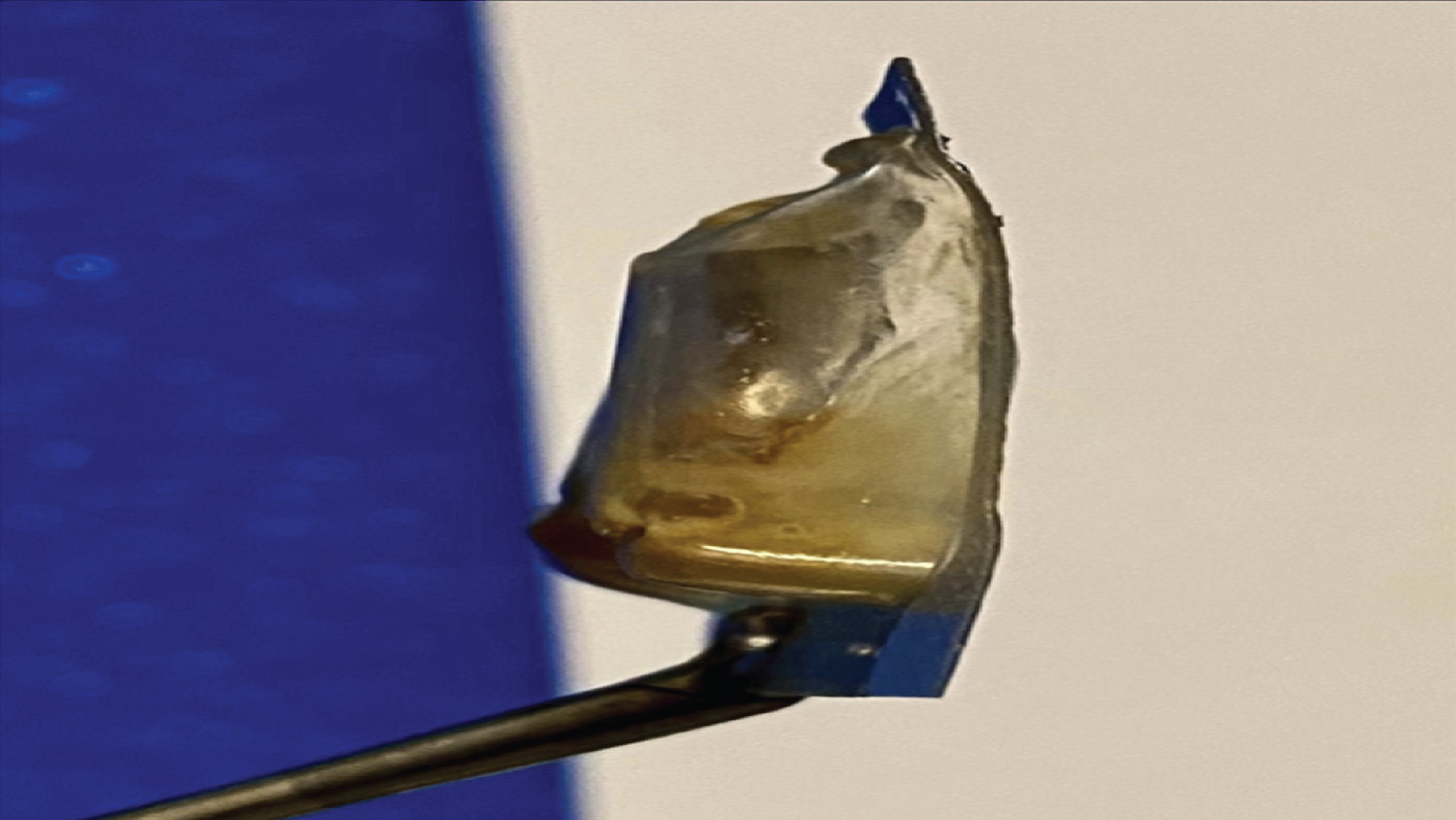 Figure 2: The foreign body is seen in the larynx with only top-end visible. View Figure 2
Figure 2: The foreign body is seen in the larynx with only top-end visible. View Figure 2
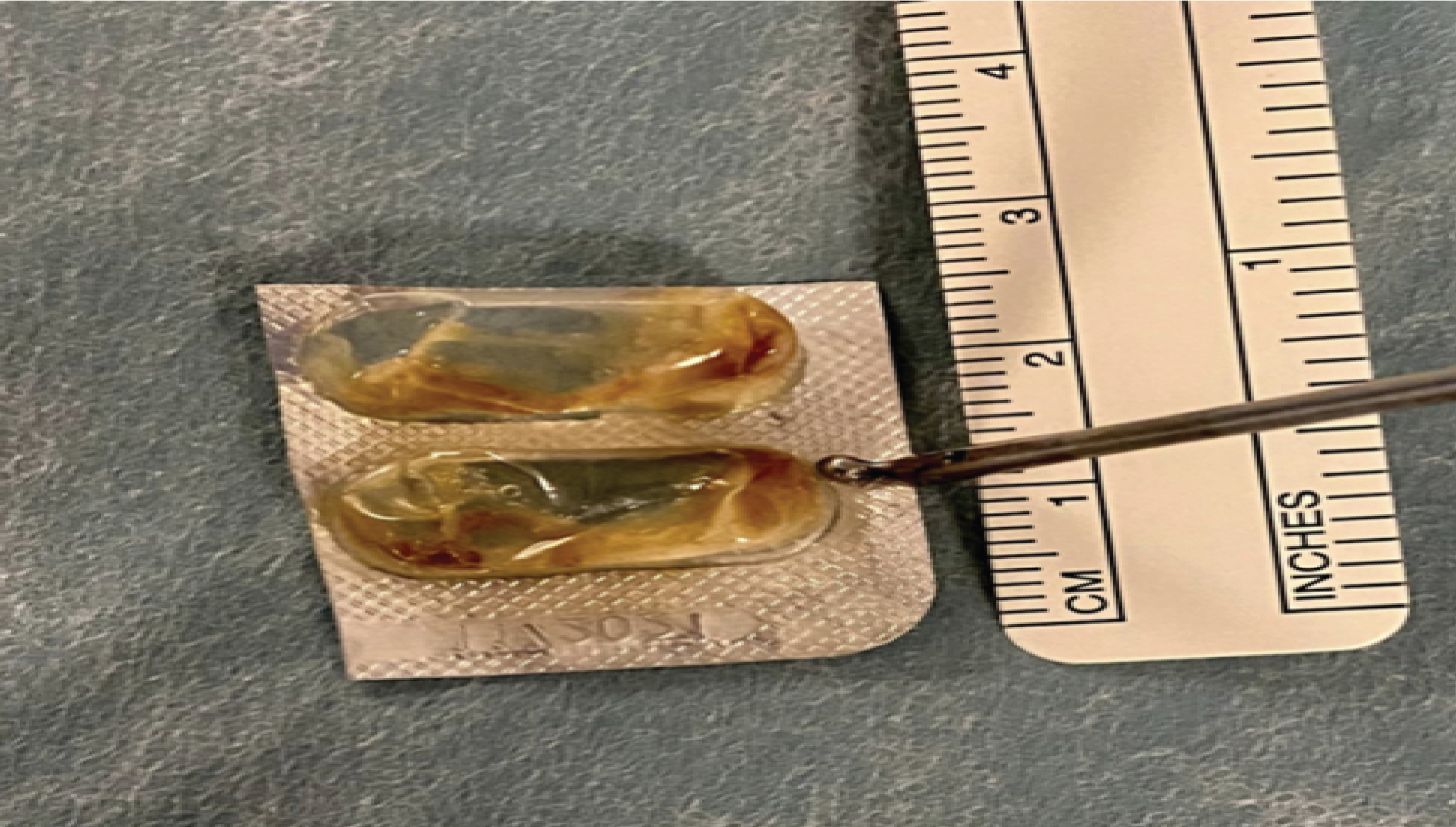 Figure 3: The blister pack (Foreign body) after removal, measuring cranio-caudally (2.6 cm). View Figure 3
Figure 3: The blister pack (Foreign body) after removal, measuring cranio-caudally (2.6 cm). View Figure 3
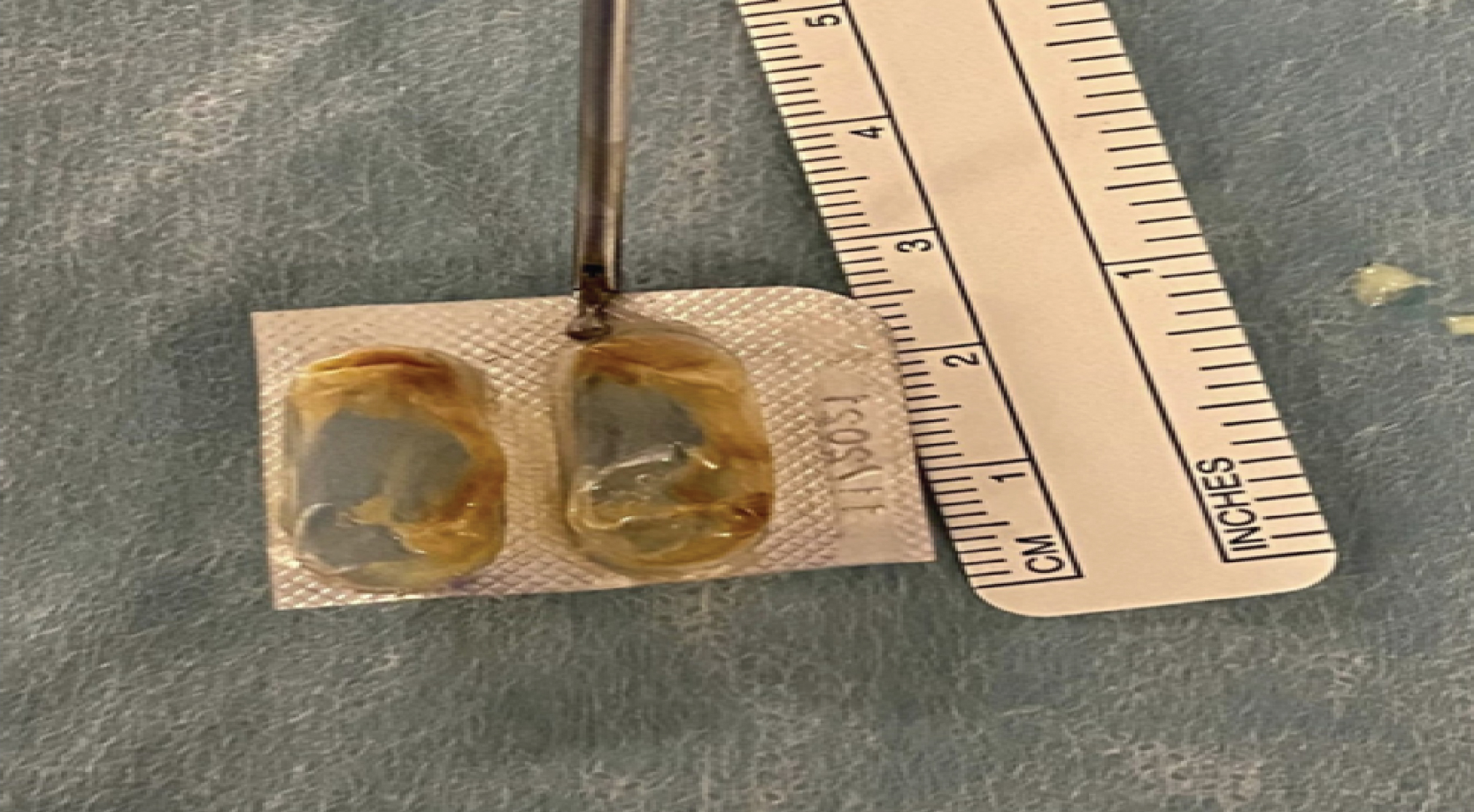 Figure 4: The blister pack (Foreign body) after removal & measuring Antero Posteriorly (2.2 cm). View Figure 4
Figure 4: The blister pack (Foreign body) after removal & measuring Antero Posteriorly (2.2 cm). View Figure 4
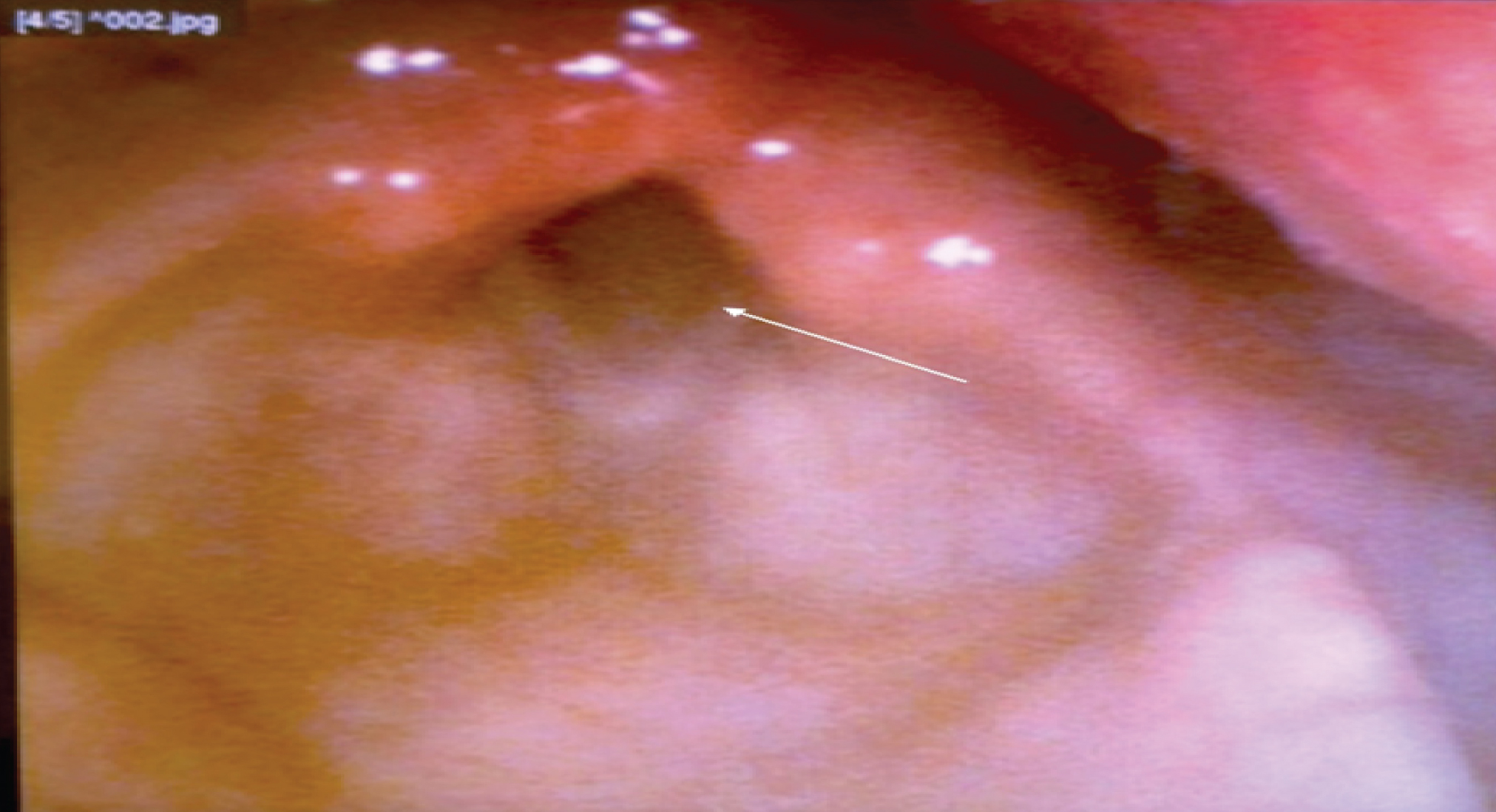 Figure 5: A normally functioning larynx three months after the removal of the foreign body. View Figure 5
Figure 5: A normally functioning larynx three months after the removal of the foreign body. View Figure 5
Adults with a median age of 64 years are the most frequent group of patients presenting with a foreign body in the larynx; however, our patient was a 45-year-old male [6]. The foreign body in the upper airway usually presents with shortness of breath, stridor, sudden hoarseness of voice, drooling, wheezing, and choking sensation within a short time following an act of aspiration [2]. The patient had presented with symptoms of dyspnoea and wheeze but had no signs of stridor, choking, or hoarseness of voice. He was admitted twice in the previous few weeks and managed as an inpatient with a presumed diagnosis of asthma. Our patient was oblivious of inhaling or swallowing a foreign body. The atypical symptoms and absence of a definitive history of aspiration muddled the suspicion of a FB till fresh symptoms of hoarseness of voice and coughing out a few pieces of silver foil emerged.
A lack of a high degree of suspicion was probably responsible for a delay in diagnosing the presence of a FB. A plain X-Ray of the chest did not help either as FB was lodged in the larynx and, the roentgenogram did not include the upper neck. The delay in diagnosis could have been avoided by paying more attention to the medical history of new-onset asthma and partial resolution of symptoms with medical management. A request for an endoscopic airway assessment in such presentations can help with an early diagnosis.
The patient reported partial improvement of symptoms with antibiotics, bronchodilators, steroids, and oxygen support. A similar case report in the literature describes a patient with a foreign body in the larynx, managed as a case of asthma. His symptoms resolved partially until the foreign body was discovered and removed [8].
Our patient had impacted FB in the narrowest region of the larynx [1], i.e., Rima glottis, for 20 days, which is significantly longer than the previously reported publication of three days in a 78-year-old man with neurological disabilities [9]. His alcohol dependence and epilepsy could have predisposed him to increased chances of aspiration [1]. The FB had partially blocked the laryngeal inlet (Figure 1), thus allowing for air exchange and survival of the patient. The FB can lead to laryngospasm [10] and a catastrophic cessation of breathing. The typical history of a choking event was seen in approximately 5% of all adult patients [11]. There was always an impending risk to his life throughout the presence of the foreign body in the larynx.
The laryngeal foreign bodies are better removed in a controlled environment of the operating room if the situation and time permits. Intubation past the foreign body may push the FB into the trachea or principal bronchi; hence no attempt was made to intubate the patient. We could retrieve the FB by direct laryngoscopy at the first instance. In case of an unfortunate event of failure to extract the FB, there were two possibilities, complete obstruction of the laryngeal airway and dislodgment into the distal airway. The plan was to perform an immediate cricothyroidotomy or a tracheostomy in case of complete airway obstruction [12]. A rigid bronchoscope (6) extraction was the procedure of choice to remove the FB if it dislodges into the lower airway. The removal of FB leads to a complete resolution of symptoms [8].
Foreign body aspiration should be a part of differential diagnosis in patients with new-onset asthma and partially resolving wheeze with medical management. An endoscopic airway assessment in such patients can help reach an early diagnosis. A definitive history of FB aspiration may not be available in patients with alcohol or drug dependence or neurological disorders. Successful removal of a foreign body in the larynx requires good teamwork in the operating room and readiness to deal with any eventuality of airway compromise.
Not applicable.
The authors declare that they have no conflict of interests.