Asthma is a heterogeneous disease which is characterized by chronic airway inflammation. It is an affecting 1-18% of the population in different countries. It can be treated mainly with inhaled medications in several forms, including the pressurized Metered-Dose Inhaler (MDI). MDI use can, unfortunately, be difficult for patients to use and even with repeated demonstration and some patients will still find co-ordination of the whole technique challenging, failing to master it despite repeated demonstration.
To evaluate the effect of the intervention on MDI use technique among adult asthmatic patients who attend a respiratory clinic in Jimma University Medical Center (JUMC), Southwest Ethiopia.
The interventional study was conducted from March-August 22/2018. All adult asthmatic patients who met inclusion criteria were included in the study. Patient baseline assessment was conducted (patient demography, inhalation technique, adherence, and asthma control status). The baseline inhalation technique was obtained using a standard check-list of recommended steps National Institute of Health (NIH) guidelines. After the intervention, inhalation technique was re-evaluated. Independent predictors of outcome identified and strength of association between dependent and independent variables determined by using binary logistic regression analysis and statistical significance was considered at p < 0.05. McNemar test was used to compare the pre-, post-result of the inhalation technique.
One hundred forty patients were included in the analysis. The most frequent critical step mistake in both pre- and post-intervention was the short duration of the inhalation 87.1%. At the first visit, 121 (86.4%, 95% CI: 81-92) patients were inefficient and it was dropped to 103 (73.57%, 95% CI: 66-81) after the intervention. The mean critical error was 2.69 in pre-intervention and dropped to 2.09 after an intervention. Before the intervention, 18 (12.9%) patients were controlled and increased to 26 (18.4%) after intervention.
Most of the study participants were inefficient before the intervention. After the intervention, the number of patients who were efficient is increased as compared to pre-intervention and found to be highly significant in the inhalation technique. The Hospital tries to adopt the video MDI teaching program and the patient should ask health care professional show to take medication and they should bring their device to receive a demonstration during the visit. Health professionals should re-evaluate the patient during their Hospital visit and encourage them to bring their device to give a demonstration.
Asthma, Intervention, Metered dose inhaler, JUMC
JUMC: Jumma University Medical Center; MDI: Metered Dose Inhaler; NIH: National Institution of Health; OPD: Outpatient Department; TAI: Test of Asthma Inhalation
Asthma is a heterogeneous disease which is characterized by chronic airway inflammation. It is a common chronic respiratory disease affecting 1-18% of the population in different countries [1]. Even though there is no nationwide study in Ethiopia, prevalence of bronchial asthma among adult patients in Debre berhan was 29.6% [2]. Most Nepalese families were found to use unprocessed biomass fuel (such as grass, wood, charcoal, renants of animals) for cooking and heating and hence respiratory symptoms have been associated with the use of smoky fuels in Nepal and in other countries [3].
Prevention of disease progression, improvement of symptoms, exercise tolerance and decrease in exacerbations and mortality are the goals of management for asthma [4]. The medications normally used in asthma are the bronchodilators and anti-inflammatory agents. Systemic administrations of the sea gents produce considerable side-effects. Hence, to overcome this problem as well as have a quicker onset of action and for better efficacy, inhaled medications are preferred [5].
Good inhaler technique is vital for a drug to be effective and bearing in mind the wide range of drugs used for the treatment of respiratory conditions cost of misuse can be significant. If patients are not using their inhalers correctly the need for increased dosages, systemic steroids and irregular visits to the doctor may increase. Only 79% of patients tested could use the MDI efficiently even after instruction. Patient education should play an important part in the provision of the inhaler device. The technique should be assessed by direct observation after expert instruction [6].
MDI is one of the most commonly used devices in the management of asthma. This can, unfortunately, be difficult for patients to use and even with repeated demonstration and assessment some patients will still find co-ordination of the whole technique challenging, failing to master it despite repeated training [7].
Previous studies have reported a high rate of inadequate inhalation technique varying from 77.5% to 89.2%. In addition, a gradual temporal decline in the correct technique of inhaler use has also been observed. This information is essential to plan a structured educational protocol while initiating patients on MDI therapy [8].
The consequences of poor inhaler technique are also financial, with one review estimating that about a quarter of all expenditure on inhalers is wasted owing to poor inhaler technique. The total cost burden associated with poor inhalation technique more than doubled when productivity losses were taken into account [9]. Miss utilization of MDI has a great role for control of asthma as the study shown which was conducted in different countries outside Ethiopia and in Adis Ababa. So this study, therefore, aims to evaluate the use of inhaler technique and its determinants with a view to providing possible solutions and appropriate interventions on how to improve the inhaler technique.
This study was done in JUMC, Jimma, Ethiopia. JUMC is located in Jimma town which is 346 km far from Addis Ababa and it is found southwest Ethiopia. It is one of the largest teaching University hospitals in Ethiopia. JUMC is offering diagnosis and treatment for approximately 10,791 patients per month. There are about 9 outpatient clinics located within the hospital which serves over 9592 visits/month [10]. Among these Outpatient department (OPD) visits, about 45 patients are asthmatic (according to GINA, 2017 guide lines and physician decision) per month [11]. This study was conducted specifically at OPD service which is a respiratory clinic from March, to August, 22/2018 G.C.
Hospital-based Interventional study was used to assess the effect of the intervention on metered dose inhaler use technique among asthmatic patients attending the respiratory clinic in JUMC. All adults age 18 and above, patients with confirmed diagnoses of asthma and who are willing to participate and having followed up at outpatient respiratory clinics were taken as the source population. Patients having exacerbations during the data collection period, being handicapped and age > 75-years-old were excluded from the study. Finally, all adult patients who satisfy the inclusion criteria were a candidate as a subject for the study.
All adult patients who met inclusion criteria and presented to the hospital in the data collection period were recruited in the following way.
Figure 1 the selection criteria of sample population.
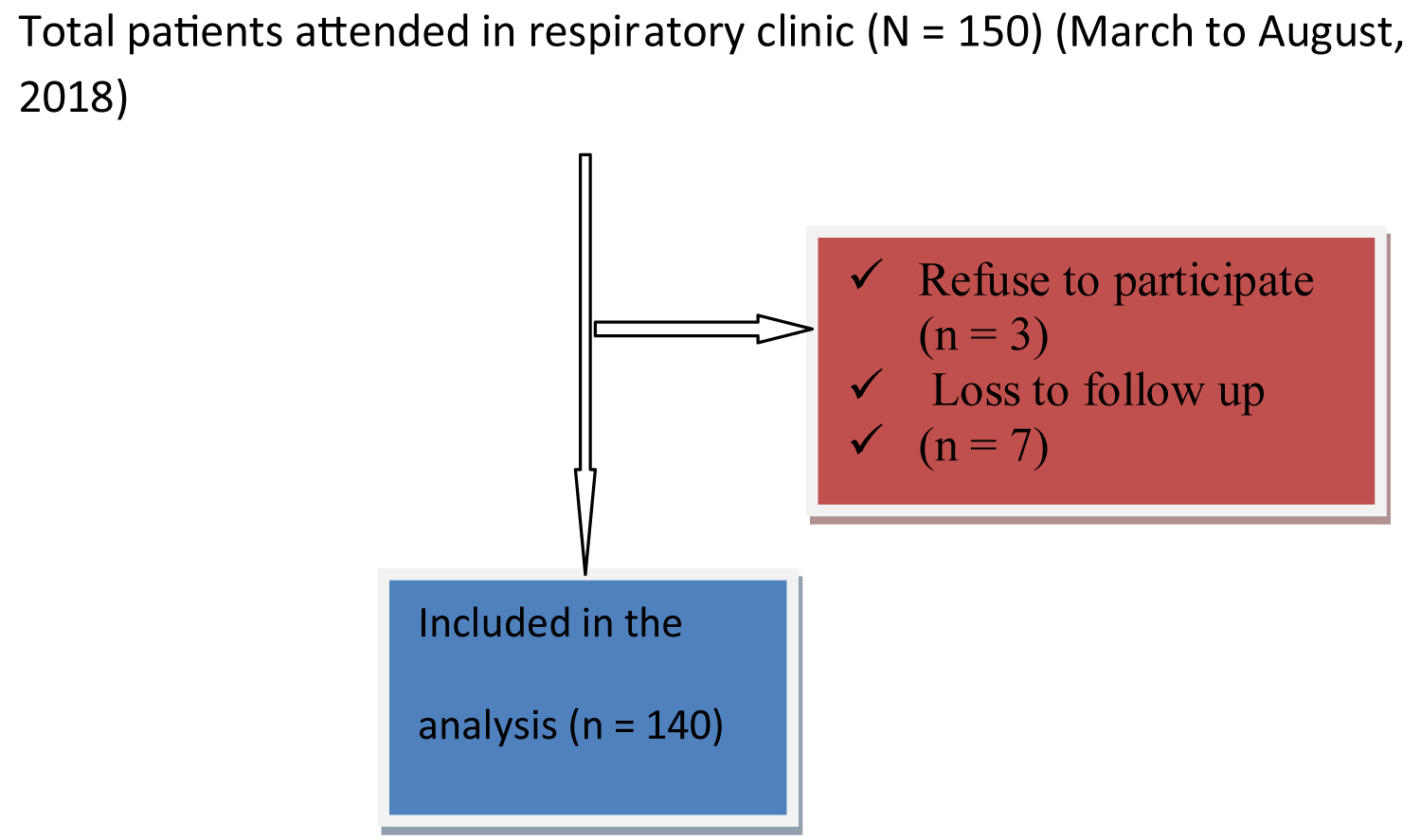 Figure 1: Summary of sampling procedure.
View Figure 1
Figure 1: Summary of sampling procedure.
View Figure 1
Relevant information like patient characteristics, inhalation technique, current medications, co-morbidities, duration of illness, inhaler use and adherence (assessed by asthma inhaler test) were recorded using a structured questionnaire (adapted from different published literature [12-16]. The questionnaire was translated into local language and retranslated to English. Relevant data were obtained by interviewing the patient inhalation demonstration/observation and chart review when necessary. At baseline, data were collected regarding patient demographics, frequency of follow up, inhalation technique, previous MDI instructions, and asthma control status (frequency of asthma symptoms, severity of symptoms, presence of overnight symptoms and restriction of activity, GINA, 2017) [1]. An empty and their own MDI was adapted to enable a patient's inhalation technique to be recorded and patients were asked to use their aerosol just as if they would be at home. Patient baseline inhalation techniques were identified, using a standard check-list of recommended steps by the National Institute of Health (NIH) guidelines [17] with 1 point given for each step performed correctly (maximum score = 8). The inhalation technique was dichotomized as efficient and inefficient. Patients who performed three critical steps correctly regardless of the other steps were considered as efficient and otherwise inefficient [18].
Following baseline assessment, patients were given inhalation technique information leaflets and inhalation technique demonstrations. The demonstration was given by trainer after 1-day training about the inhalation technique. The patient's inhalation technique was re evaluated in the 2nd visit. Supplementary information and clarifications on some patient's medical information were obtained through discussion with respective nurses and physician. Identified baseline technical inhalation errors were recorded.
Data were entered into a computer using EpiData 3.1 software and analyzed with SPSS version 21. Before analysis, the presence of colinearity between independent factor (having less than 2 variance inflation factor) and model fitness (with Hosmer Lemeshow p-value 0.156) were checked. Chi-square statistics were used to check the adequacy of cells for binary logistic regression. Independent predictors of outcome and strength of association between dependent and independent variables were identified by using binary logistic regression analysis and P-value < 0.25 entered to multiple regressions. P-value < 0.05 was considered as significant. McNemar test was used to evaluate whether there is a difference between pre and post-intervention inhalation technique. Descriptive statistics were used to characterize the inappropriate utilization of MDI and independent variables. The results of the study were organized in the form of frequencies and percentages. The data was summarized and described using tables and figures.
A total of 140 patients were included in the study. Of which 78 (55.7%) were females. The overall response rate was 98%. The mean age was 47.8 (age range 19-74) years with the maximum number of patients being in the age group of 41-59 years. About (32.9%) patients were farmers. The majority of patients 110 (78.57%) found to have isolated asthma (have no confirmed comorbidity). Fifty-seven (40.7%) patients had moderate persistent asthma, 35% had severe persistent and the rest 24.3% had mild persistent. Classification of asthma severity is according to GINA, 2017 guidelines. Only 3 (2.1%) of the study subjects were current smokers while 121 (86.43%) were non-smokers. Among study participant, 71 (50.7%) patients were illiterate and only 8 (5.7%) were attended post-secondary school. Seventy-seven (55%) and 72 (51.4%) patients drank alcohol and chew khat respectively. The majority of patients 88 (62.9%) were exposed to biomass fuels during cooking food and other activities shown in (Table 1). Among these, females were 55 (39.29%). The median duration of illness and MDI experience was 4 years (ranges from 4 months-42 years) & 3 years respectively. Fifty-eight (41.42%) patients knew the importance of gargling after inhalation of steroids. Sixty-nine (49.3%) had experienced an asthma exacerbation in the past 12 months. About 29.3% of patients were admitted to hospital and only 9.76% admitted more than 2-3 times per year.
Table 1: Socio-demographic and clinical characteristics of participants, respiratory clinic, JUMC, Ethiopia, 2018. View Table 1
Thirty (21.42%) patients wanted to receive information about how to take their medication from health professionals during their hospital visit. Sixty patients received education about their medication previously from different health professionals. Of these, 32 (53.3%) of them received from physicians and the rest were educated by other health professionals (Figure 2). Twenty eight (46.7%) patients received a demonstration and the rest 53.3% received verbal instruction. Among total patients who received demonstration, 25 (41.67%) patients were re-evaluated: 12 (48%) once, 8 (32%) twice, 4 (16%) three times and only 1 (4%) patients re-evaluated every visit.
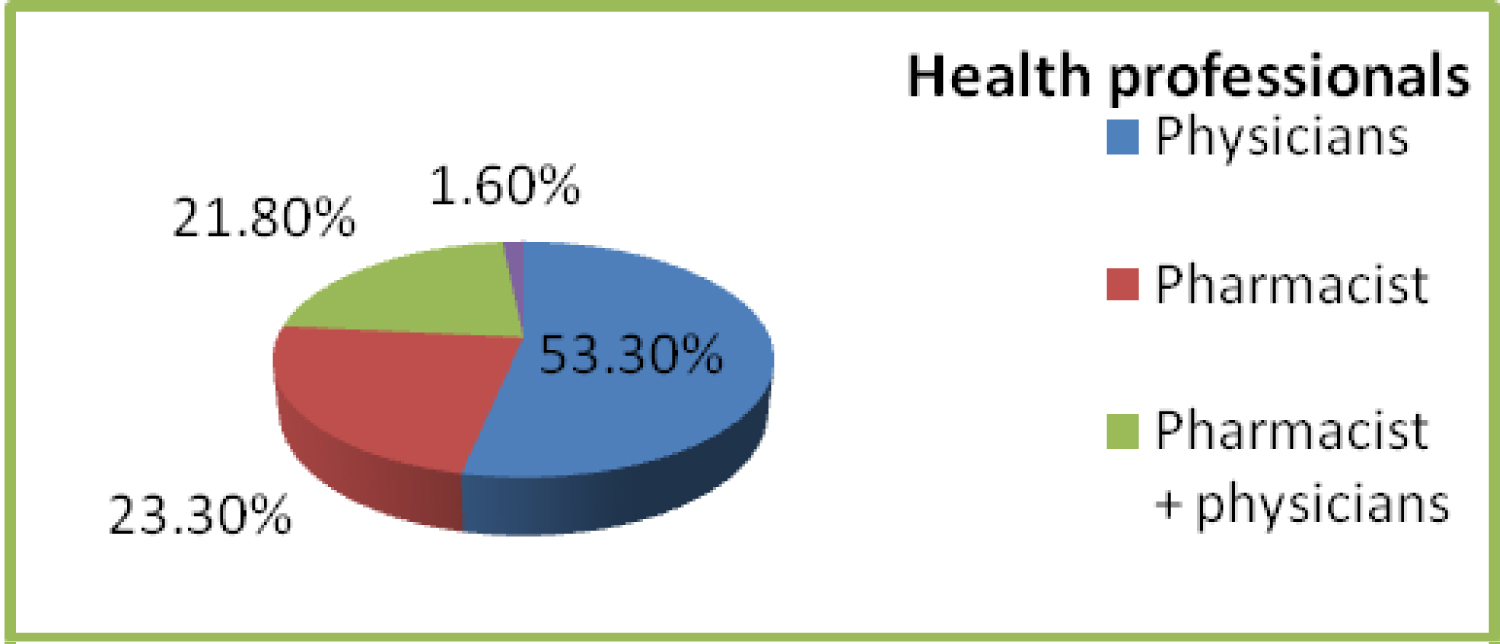 Figure 2: Sources of patient education about their inhalation technique, respiratory clinic, JUMC, Ethiopia, 2018.
View Figure 2
Figure 2: Sources of patient education about their inhalation technique, respiratory clinic, JUMC, Ethiopia, 2018.
View Figure 2
During baseline assessment, 139 (99.29%) patients had errors in one or more steps of the inhalation technique. In this visit the highest number of errors was found to be done in the step inhale slowly deeply and press canister simultaneously where 120 (85.7%) of the patients failed to do it correctly. The second most frequent error was taken the inhaler out of mouth and hold the breath for 5-10 sec., 98 (70.0%) and Lean head slightly back is the third most frequent error, 80 (57.1%). The most correctly performed steps shook the inhale rigorously (5-10 times) and place mouthpiece between teeth and lips, 124 (88.6%) and 111 (79.3%) respectively. Among 140 patients, 121 (86.42%, 95% CI: 81-92) committed at least one critical error in pre-intervention whereas it was dropped to 103 (73.6%, 95% CI: 66-81) after the intervention. The mean number of critical errors per patient was 2.69 in the first visit and which was reduced to 2.09 after the intervention.
At the 2nd visit, 130 (92.85%) patients had errors in one or more steps of inhaler technique. The highest number of errors was found to be done in step inhale slowly, simultaneously press canister and breathing in slowly and deeply which is 97 (69.28%). The second most frequent error was lean head slightly back, 69 (49.3) and take inhaler out of the mouth and hold the breath for 5-10 sec was the third most missed step which accounts 54 (38.6%). In this visit the most correctly followed step shook the inhaler vigorously (5-10 times), only 3 (2.14%) patients missed this step. Two critical steps, steps 7 and 8 were the most frequently missed steps in both first and second visits (Table 2). Before the intervention, 73 (52.14%) patients missed more than one critical step, whereas, in the second visit, this number dropped to 36 (25.7%).
Table 2: pre-post performance of inhalation technique, respiratory clinic, JUMC, Ethiopia, 2018. View Table 2
As shown in the above (Figure 3), in pre-intervention 31.9% of patients did more than four steps among a total of eight steps and which was increased to 87.1% after the intervention. Only 7.86% of patients did six steps in pre-intervention, whereas in post-intervention, this was increased to 30%. After the intervention, there was no patient who did only one or two steps (every patient performed at least three steps). About half of the patients (47.2%) did less than four steps in pre-intervention, whereas after intervention only 2 (1.4%) patients did less than four steps. The number of steps done by the patient was increased after intervention as compared to pre-intervention.
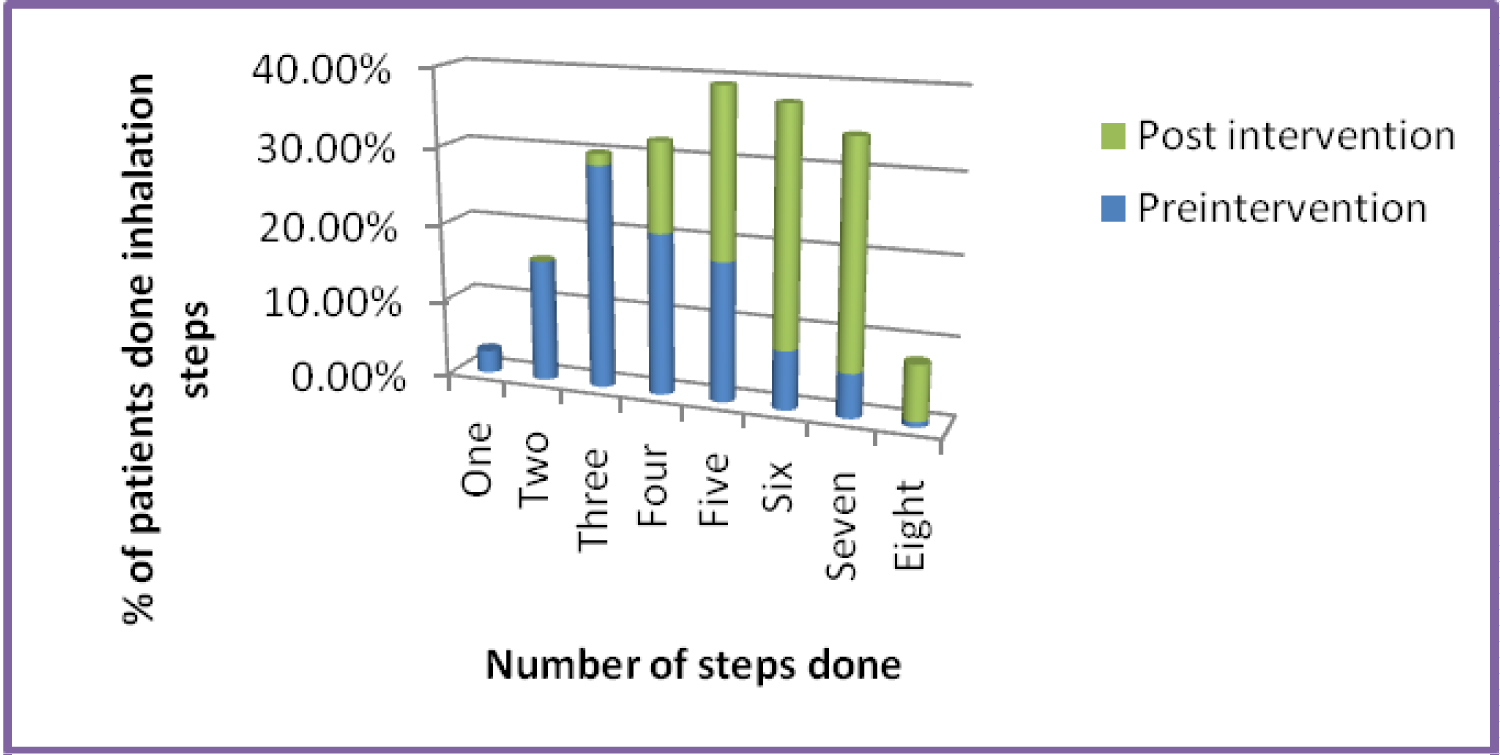 Figure 3: Number of steps done by the patient pre- and post-intervention, respiratory clinic, JUMC, Ethiopia, 2018.
View Figure 3
Figure 3: Number of steps done by the patient pre- and post-intervention, respiratory clinic, JUMC, Ethiopia, 2018.
View Figure 3
Before the intervention, 19 (13.6%) patients incorrectly performed all three critical steps, but after the intervention, none of the patients missed all critical steps. Before the intervention, the total number of patients who were able to be efficient was only 19 (13.57%) but 37 (26.42%) in post-intervention (Figure 4). After the intervention the overall efficiency of the inhalation technique was improved by 12.58%, which is significant (p = 0.007, McNemar test) (Table 2).
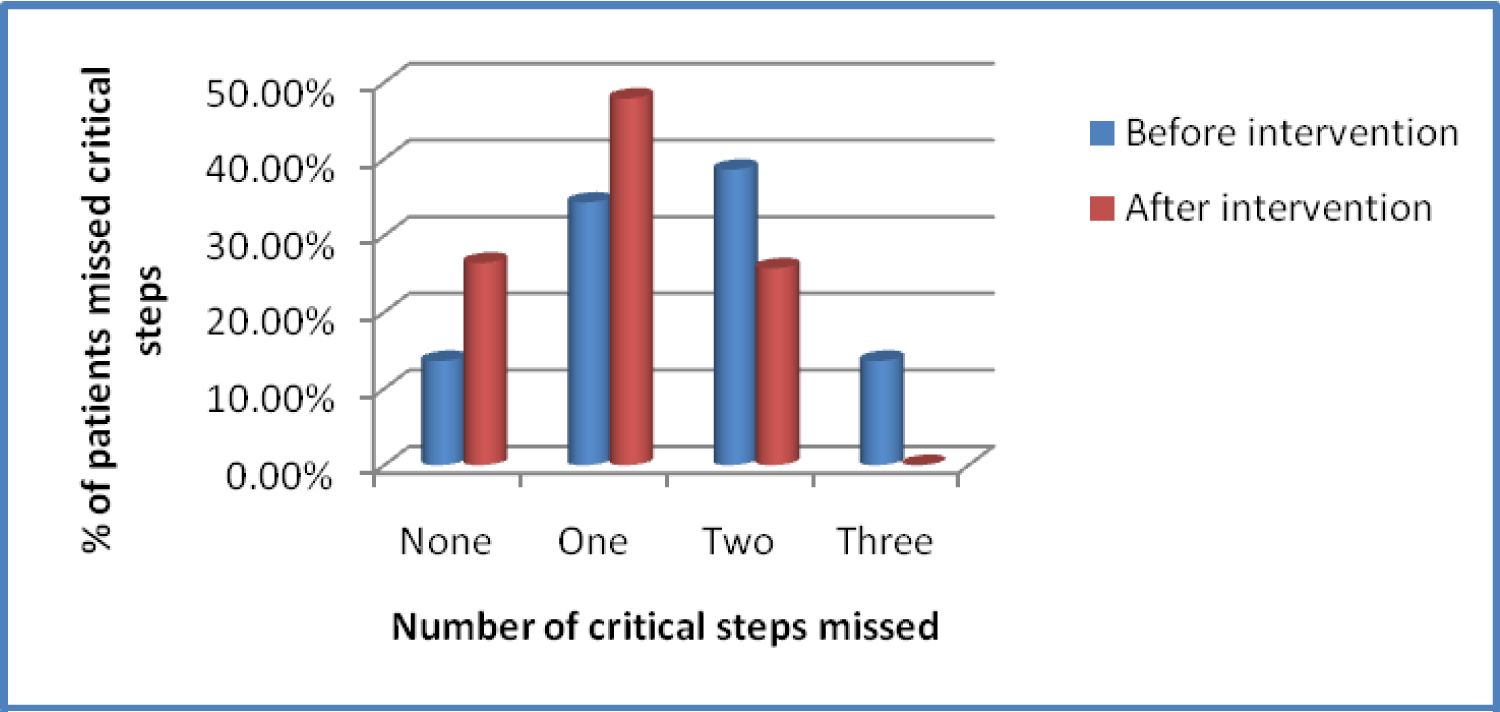 Figure 4: Number of critical steps missed in pre and post-intervention, respiratory clinic, JUMC, Ethiopia, 2018.
View Figure 4
Figure 4: Number of critical steps missed in pre and post-intervention, respiratory clinic, JUMC, Ethiopia, 2018.
View Figure 4
McNemar test was computed to see the effect of the intervention on each step of the inhalation technique and overall efficiency. In post-intervention five of eight steps were significantly improved as compared to pre-intervention. In 3 Steps (1, 4, and 5), there was no significant improvements. The overall efficiency is significantly improved at post-intervention as compared to pre-intervention (p = 0.007) (Table 2).
Multivariate logistic regression was done to identify significant independent predictors with controlling confounding factors. Sex, educational status, knowledge, and exposure for previous education were significant predictors whereas age, adherence, duration of MDI experience and attitude were not significant predictors.
Literate people were able to perform more correctly than illiterate patients. Illiterate patients who missed more than one critical step account for about 17.23%. Among all efficient patients, 26.6% illiterate, 32.14 patients having primary education, 35.1% people having secondary education, 10.8% of people having post-secondary education. Illiterates were less likely efficient as compared to patients having post-secondary education (p = 0.02).
Knowledge is significantly associated with the inhalation technique. Patients having good knowledge about their medication inhalation technique and self-management were more likely efficient than patients with poor knowledge (p = 0.049). Male patients were able to perform all critical steps more correctly than female patients, where 26 (70.27%) of male patients, and 11 (29.73%) female patients were able to perform all critical steps in the inhalation technique. Sex is significantly associated with inhalation technique (p = 0.02) (Table 3).
Table 3: Bivariate and multivariate analysis for predictors of inhalation technique among asthmatic patients, respiratory clinic, JUMC, Ethiopia, 2018. View Table 3
This is the first study in Ethiopia in which inhalation technique of patients with asthma has been tested in practical demonstration and with an instructional leaflet. This study also showed us the effect of training on the efficiency of the technique. The method is safe for the patients because a placebo canister was used for MDI devices so as to prevent hygiene-related problems.
In this study, it was found that 88.57% of the patients did not use their inhaler devices properly; even though they claimed that they knew how to inhale their medication. Before the intervention, majority of the patients believe that they knew how to use their medication however, substantial number of patients missed critical steps in practical demonstration. This result is similar with the previous studies reported in Europe, India, and Saudi [8,19-21]. However, our result is not similar to the study done in India [22]. This discrepancy could be in our study, a lower proportion of patients performed correctly two critical steps (steps 6 and 8) as compared to the previous studies.
The most frequent mistake was found to be done in the step inhale slowly, deeply and press canister simultaneously in both pre- and post-intervention. A similar finding has shown in Bulgari [23]. These small proportions of patients followed step 7 is, because this step needs high demands of skills to inhale slowly and understanding, which is better achieved when the patient actually observes the steps being demonstrated rather than simply reading them/verbal instruction. It also suggests that greater emphasis should be given on these specific steps during demonstration especially for those steps which are critical for asthma control.
In this study before intervention, patients made a higher number of mistakes as compared to post-intervention which is supported by the report in Bulgaria [23]. Only one patient was followed all steps in pre-intervention and increased to ten after the intervention. The result in pre-intervention technique was similar to the result in India by GP Jolly A [22]. But in post-intervention, our finding is lower than the previous result. This discrepancy might be because 50% of the study population is illiterate in our study as compared to the previous study which makes it difficult for the patient to remember and adhere to what they received. And most of the patients missed non critical steps which do not need high demands of skills to carry out. More than half of the patients were missed more than one critical step which might contribute for poor control of asthma. This supported by study done in Malta in which educational level was significant predictors on inhalation technique [24].
Before the intervention, all patients had errors in one or more steps of the inhalation technique (except one patient). This could be because more than half of the patients did not receive any formal education by any health care professionals regarding the proper use of inhaler devices and the proportion of patient awareness about their medication and the use of asthma devices were low. Majority of patients followed 6 or fewer steps which are high as compared to the study shown in Malta, it was about 63.5% [24]. This difference could be the frequency of follow up in our study participant is longer as compared to the previous study in which the minimum length of follow up is one month. This long duration of follow up could contribute to loss of memory that they received by the health care professionals.
Patients were significantly improved inhaler techniques in much of the steps in post-intervention as compared to the first visit. This result is similar to what was found in Serbia [25]. The overall inhalation techniques of the patients were significantly improved after the intervention. This is similar to the study done in Nepal, Bulgaria, UK, Egypt, and Germany [18,23,26-28]. In this study, the mean score of the patients before and after intervention was lower than the previous study in Nepal [26].
This disagreement could be more than half of the patients did not get previous education in our study whereas almost all of the patients received from different health professionals and repeated re-evaluation including asthma trainers in Nepal.
In our study gender is significantly associated with inhalation technique in which male is about three times more efficient than female patients. This study is in line with the previous study done in Nepal [26] but not similar compared with the result reported in India and Nigeria [22,29]. There was no significant difference between males and females for following the essential steps. This difference could be the proportion of illiterate of the female patient in our study is high as compared to male patients (67.9% vs. 29%) and share of previous education/demonstration is also low in case of females (36.4% vs. 53.2%) respectively.
Our study showed that educational status is an important factor for inhalation techniques. Illiterate patients were less likely followed essential steps as compared to patients having post-secondary education. This study is in line with the previous study conducted in India 21.2% illiterate and 78.8% literate were followed these steps correctly [22].
Patient education about inhalation techniques and/particularly practical evaluation is the main tool to target this problem. Different methods can be used to explain to patients and ensure improvement in technique, ultimately enabling patients to master the proper method. Regular re-assessment is important and recommended as patients may lose the adequate technique over time especially illiterate patients.
Patients having good knowledge are more than three times more likely to use inhalers than patients with poor knowledge and this is because patient having good knowledge can be easily shaped by the health care professionals (patients having good knowledge can understand and implimente what is forwarded from health professionals).
Patients, who received prior education on inhalation technique, use asthma device efficiently more than three times as compared to who did not receive. It is supported by the study done in India and Netherlands [22,30].
The major modifiable factors for inadequate device use were lack of knowledge regarding asthma and patient education on use of inhaler administration. Only 20% of patients received the previous demonstration about how to take their medication by the health care professionals and associated asthma control. So the researcher is better to evaluate the competency of health professionals on inhalation techniques.
Our study is relay on a physician diagnosis of asthma. Small sample size and short study period (only one-time re-evaluation).
This study revealed that though the majority of patients claimed to know how to use inhalation devices correctly, only a few patients followed all the essential steps of the inhalation technique of MDI before the intervention. This study showed that there is a significant improvement in the inhalation technique after demonstration and counselling. But more than half the patients were inefficient even after intervention. So, repeated re-evaluation during their visit is mandatory to optimize the inhalation technique. The previous demonstration, sex, knowledge and educational status were significantly associated with inhalation techniques. As there are still a lot of illiterate people in our patients, the need for proper counselling during their visit even more important. Therefore, proper and regular training about error-free inhalation technique needs to be conducted to optimize the patient benefit.
A letter of ethical clearance was obtained from the ethical review committee of the institute of health, Jimma University (JHRPGD/202/2018). A letter for cooperation from the department of internal medicine OPD services was obtained. Verbal consent from respective physicians, nurses, and patients was secured to extract data from patients' medical charts and to conduct a practical demonstration. Privacy and confidentiality were ensured during patient interview and review of patient charts.
Not applicable.
All data analyzed during this study was available for publication.
The authors declare that they have no competing interests.
This covered by Jimma University Medical Center.
Not applicable.
I would like to thank Mezan Tepi University for sponsoring me to attend my M.Sc program and Jimma University for motivating and sponsoring me to do this research. I am also very grateful to the nursing staff for their cooperation in giving sufficient patient information. I would like to give special thank you to my study participants for their cooperation to participate in this study.