One of the most important causes of acute hepatitis is vascular pathologies of the liver. There are several well-recognized forms of vascular injury to the liver, including Budd-Chiari syndrome, ischemic hepatitis, hepatic infarction and passive congestion due to hemodynamic instability. We present a case of acute liver injury accompanied by hemodynamic and respiratory pathologies.
A 53-year-old lady was admitted to the emergency department with complaints of abdominal pain, nausea, vomiting for a week. Gastrointestinal examination was normal. Laboratory tests revealed mild thrombocytopenia, prolonged international normalized ratio (INR) and transaminases were ten-fold higher. In abdominal ultrasonography, no signs of chronic liver failure and vascular pathologies. Abdominal computed tomography (CT) revealed no pathology. Transthoracic echocardiography disclosed severe mitral regurgitation and dilatation of both atria and right ventricle. Pro-BNP level was increased. Thorax CT demonstrated filling defect compatible with pulmonary thromboembolism (PTE). The patient was accepted PTE, and enoxaparin treatment was initiated. Under the anticoagulant and diuretic treatments, the patient's orthopnea disappeared, control blood values declined.
Acute liver injury can be the initial presentation in a patient with severe valvular disease and acute PTE.
Cardiac decompensation, Echocardiography, Heart failure, Hepatitis, Severe mitral regurgitation, Pulmonary thromboembolism
ALP: Alkaline Phosphatase; ALT: Alanine Aminotransferase; AST: Aspartate Aminotransferase; CT: Computed Tomography; CTPA: CT Pulmonary Angiography; ECG: Electrocardiography; GGT: Gamma Glutamyl Transferase; INR: International Normalized Ratio; LDH: Lactate Dehydrogenase; Pro-BNP: Prohormone B-Type Natriuretic Peptide; PTE: Pulmonary Thromboembolism
Hepatitis refers to an inflammatory condition of the liver. It's commonly caused by a viral infection, but there are other possible causes of hepatitis. These include autoimmune hepatitis and hepatitis that occurs as a secondary result of medications, drugs, toxins, and alcohol [1]. Henrion, et al. reported that acute hepatitis may also develop in hemodynamic instability such as congestive heart failure, acute heart failure, chronic respiratory failure and septic/toxic shock [2]. Severe acute liver injury defines a syndrome characterised by markers of liver damage (elevated serum transaminases) and impaired liver function (jaundice and INR > 1.5) which usually precedes clinical encephalopathy [3]. Here, we present a case of acute liver injury accompanied by hemodynamic and respiratory pathologies.
A 53-year-old morbidly obese lady was admitted to the emergency department with complaints of abdominal pain, nausea, vomiting, weakness, loss of appetite for a week. Her medical history included hypothyroidism and mitral regurgitation. She didn't have a history of smoking or exposure to any kind of chemical and hepatotoxic food. She had a history of drinking two beers a week. She had a temperature of 37 ℃, a pulse rate of 115 beats/minute, a respiratory rate of 24 breaths/min, in room air fingertip saturation of 96% and a blood pressure of 115/60 mmHg. In the respiratory system examination, inspiratory crackles were heard in the bilateral lower zones. A 2/6 systolic murmur was heard over the mitral area. Pretibial 2+ edema was present. There was no feature in the gastrointestinal examination. There was atrial fibrillation with high ventricular rate in her ECG. Cardiothoracic index was found to be increased in posteroanterior chest X-ray. Hemogram examination showed mild microcytic anemia (hemoglobin: 11 g/dL) and mild thrombocytopenia (platelet count: 109400/μL). In the coagulation panel, international normalized ratio (INR) was prolonged (INR: 2.14), and in the biochemical parameters transaminases were ten-fold higher (AST: 695 U/L, ALT: 983 U/L). Serum cholestasis markers are elevated (ALP: 174 U/L, GGT: 326 U/L, LDH: 717 U/L). Serum bilirubin levels slightly high. The patient with acute hepatitis didn't consume specific medication and food. Serum viral serologies were negative. Serum transaminase levels were found to be normal in the blood tests performed during the cardiology examination two months ago. In abdominal ultrasonography, no signs of chronic liver failure and vascular pathologies. Liver sizes slightly increased and edematous appearance in perihepatic area. Hepatic veins were normal diameters. Inferior vena cava dilated (IVC > 2 cm) and when the respiratory collapse was less than 50%. Abdominal computed tomography (CT) showed no significant pathology. Autoimmune serologic tests (antinuclear antibody, liver kidney microsomal autoantibody type-1, anti-mitochondrial antibody, anti-smooth muscle antibody) were normal. Intravenous furosemide infusion was initiated due to congestive heart failure, and intravenous atrioventricular nodal blocking agents were applied to treat high ventricular rate. Transthoracic and transoesophageal echocardiogram disclosed normal left ventricular systolic function, severe mitral regurgitation, dilatation of both atria and right ventricle, severe pulmonary hypertension (estimated systolic pulmonary artery pressure was 59 mmHg). And also Pro-BNP level was increased (Pro-BNP: 4281 pg/mL). The patient's current hepatitis table was evaluated in favor of congestive hepatopathy secondary to cardiac decompensation. For the aetiology of cardiac decompensation, thorax CT pulmonary angiography (CTPA) was performed. In the CTPA study, filling defect compatible with pulmonary thromboembolism was observed in lower lobe segment branch of right pulmonary artery. There was also pleural effusion in right hemithorax and typical pulmonary infarction (Figure 1). The patient was diagnosed with having acute submasive pulmonary thromboembolism, and enoxaparin treatment was initiated. Under the anticoagulant, diuretic and symptomatic treatments, the patient's orthopnea disappeared, control transaminases regressed (AST:85 U/L, ALT:223 U/L), INR returned to normal. Thrombocytopenia improved (Table 1).
Table 1: In blood chart. View Table 1
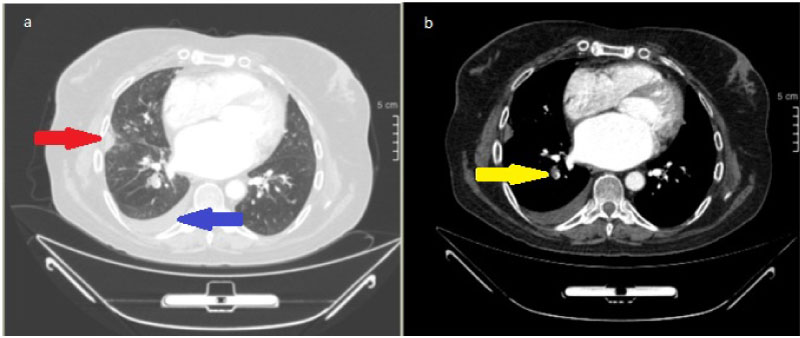 Figure 1: Thorax CT/CT angiography; pleural efusion in right hemithorax [blu earrow], typical pulmonary infarction [red arrow] (a), filling defect compatible with pulmonary thromboembolism was observed in lower lobe segment branch of right pulmonary artery [yellow arrow] (b). View Figure 1
Figure 1: Thorax CT/CT angiography; pleural efusion in right hemithorax [blu earrow], typical pulmonary infarction [red arrow] (a), filling defect compatible with pulmonary thromboembolism was observed in lower lobe segment branch of right pulmonary artery [yellow arrow] (b). View Figure 1
This case illustrates how the combination of pulmonary embolism and severe valvular heart disease can present as acute liver injury. The circulatory system is a complex interaction between multiple organs. Circulatory dysfunction ocurs when one or more organs begin to fail and disrupt adequate delivery of blood to the body [4]. A pathology that occurs in the circulatory system directly affects other organs such as the liver. The majority of cases of ischemic hepatitis occur in the setting of congestive heart failure, illustrating the dual hit of both arterial hypoperfusion and chronic passive venous congestion that set the liver up for central hypoxia [5]. Organ dysfunction also develops because of inadequate blood collection. As a result, following a period of hepatic under-perfusion, liver transaminases can become markedly elevated. ALT levels are correlated highly with right atrial pressure, free hepatic venous pressure, and wedged hepatic venous pressure [4]. Therefore ALT increase is more dominant. An ALT/LDH ratio of less than 1.5 is more typical of hypoxic hepatitis than viral hepatitis or drug induced liver injury [6]. In more severe cases such as acute liver failure, thrombocytopenia and INR prolongation may be seen. In our case, ALT level was dominantly elevated. The ALT/LDH ratio was 1.37. Thrombocytopenia was present and INR was prolonged. Viral serological markers were negative. Laboratory findings were compatible with acute liver failure. Serum transaminase levels were found to be normal in the blood tests performed during the cardiology examination two months ago. In abdominal ultrasonography, no signs of chronic liver failure and vascular pathologies. These findings have taken us away from chronic liver failure and non-alcoholic steatohepatitis. Hepatic veins were normal diameters and no ischemic pathology. These conditions prevented us from thinking of a hepatic vascular pathology such as Budd-Chiari syndrome, hepatic sinusoidal obstruction syndrome etc. With signs of congestive heart failure (orthopea, in abdominal ultrasound; liver sizes slightly increased and edematous appearance in perihepatic area, inferior vena cava dilated (IVC > 2 cm), when the respiratory collapse was less than 50%) and increased pro-BNP level in mind, transthoracic and transoesophageal echocardiography revealed severe eccentric mitral regurgitation (Figure 2) due to rheumatic mitral valve disease, severe pulmonary arterial hypertension. Despite adequate diuresis in response to diuretics and AV nodal blocking agents, the patient's orthopnoea persisted. Congestive hepatopathy refers to hepatic manifestations attributable to passive hepatic congestion, as occurs in patients right-sided heat failure. Passive congestion often coexistis with reduced cardiac output, making their relative contributions to hepatic injury interwined [7]. We hypothesise that the pulmonary thromboembolism was the last hit that resulted in acute liver failure.
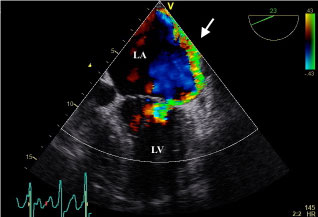 Figure 2: Transoesophageal echocardiogram in apical 4 chamber view depicting severe eccentric mitral regurgitation (white arrow). LA: left atrium; LV: left ventricle. View Figure 2
Figure 2: Transoesophageal echocardiogram in apical 4 chamber view depicting severe eccentric mitral regurgitation (white arrow). LA: left atrium; LV: left ventricle. View Figure 2
The hypotension is the most important clinical finding of cardiovascular collapse caused by massive pulmonary embolism. Early mortality was significantly higher in patients with right ventricular dysfunction than echocardiography despite hypotension [8]. Aslan, et al. was suggested that there may be a relationship between elevation of transaminase and the severity of pulmonary thromboembolism [9]. Van den broecke, et al. was emphasized that pulmonary thromboembolism is a rare cause of hypoxic hepatitis (1.4%), but it is one of the most common causes of death in early mortality (37.5%) [10]. Therefore pulmonary thromboembolism is a rare but mortal complication of acute hepatitis. Our patient did not develop hypotension and shock, but there were signs of right ventricular dysfunction in echocardiography and cardiac enzymes. Patient was deemed as submassive pulmonary thromboembolism and we immediately started anticoagulant therapy. Follow-up after anticoagulant therapy showed improvement in symptoms, decreased transaminases, improved thrombocytopenia and normalization of INR. The normalization of the blood chart in 7-10 days also support congestive hepatopathy.
In conclusion findings of congestive heart failure and hepatitis can mask the pulmonary thromboembolism. Pulmonary thromboembolism should be included in the differential diagnosis especially in patients with acute liver injury, especially if cardiac pathologies and respiratory symptoms accompany.
• I would like to thank our patient who allowed us to present this case and all my colleagues who helped us during the case presentation.
• On behalf of all the contributors I will act and guarantor and will correspond with the journal from this point onward.
• Material described is not under publication or consideration for publication elsewhere.
• No financial or other support was received during the creation of the article.
• There are no conflicts of interest in connection with this paper.
• All of the authors declare that they have all participated in the design, execution, and analysis of the paper, and that they have approved the final version.