Catamenial pneumothorax is the most common form of thoracic endometriosis syndrome. It is a form of spontaneous recurrent pneumothorax, occurring mostly in women of reproductive age, typically within 72h from the onset of menstruation. Although aetiology is unknown, several hypothesis have been raised trying to explain the pathogenesis behind it. We present two cases of women in reproductive age, with episodes of recurrent right pneumothorax. In surgery were visualized diaphragmatic defects compatible with the diagnosis of catamenial pneumothorax. After surgical correction and hormonal treatment,they are asymptomatic and without new episodes of pneumothorax.
Thoracic endometriosis (TE) is a clinical condition manifested clinically by catamenial pneumothorax, hemoptysis, catamenial hemothorax and pulmonary nodules [1-3].
The most common clinical presentation of TE is catamenial pneumothorax [1,2,4-7]. However, it is also known that absence of TE can occur, associated with diaphragmatic defects [8]. Catamenial pneumothorax was initially described in 1958 by Maurer, et al. [9]. It is a rare form of secondary spontaneous pneumothorax, under diagnosed. It occurs mostly in adult women, with a peak of incidence between 30-35 years. It is characterized by recurrent pneumothoraces, in perimenstrual period, usually occurring within 72 hours before or after onset of menstruation [1,8,10], mostly in the right hemithorax [1,4,6,8,10]. It corresponds to 3-6% of cases of recurrent spontaneous pneumothorax and a third of all cases of spontaneous pneumothorax in women at reprodutive age [1,2,4].
As recurrences are common, the best recommended treatment is a combination of surgery and hormone therapy [1].
Catamenial pneumothorax aetiology is still unknown, although several theories try to explain it.
We report in this article 2 cases of young women with recurrent spontaneous pneumothorax, surgically diagnosed with catamenial pneumothorax.
A 37-year-old patient with a history of bronchial asthma and allergic rhinitis, non-smoker. She went to the emergency department due to progressively worsening dyspnoea, cough and productive cough and fever. An X-ray showed a large right pneumothorax. A chest tube was placed in the 5 th intercostal space, in the midaxillary line. After documenting the resolution on chest CT, the chest tube was removed. CT showed no blebs or bullae. However, there was recurrence of the pneumothorax during hospitalization. For this reason, she was transferred to Thoracic Surgery, and underwent wedge resection of the right upper lobe and mechanical pleurodesis by video-assisted thoracic surgery (VATS). Subsequently, due to a new recurrence of pneumothorax, she needed a new surgery, and were visualized diaphragmatic fenestrations suggestive of catamenial secondary spontaneous pneumothorax. She underwent right pleurectomy and diaphragmatic talcage. After the surgical intervention, she initiated hormone suppression with monthly goserelin for 6 months, without recurrence.
A 41-year-old patient with only known history of rhinitis. Previous admitted one month earlier for spontaneous right pneumothorax. She came back with pain located in the right shoulder and irradiation to the scapula, worst with deep inspiration, with one day of evolution. She denied associated trauma. No clinical signs of infection. She wasn´t menstruated. Chest radiography showed right pneumothorax without deviation of mediastinal structures. After placement of the chest tube, an apical pneumothorax chamber was maintained. As it was a second episode, the thoracic surgery was contacted. She underwent atypical right superior lobe resection with pleurectomy and talcage, by VATS. Multiple diaphragmatic fenestrations were seen, some pericentimetric with hepatic exposure. No intrathoracic endometriosis, bleds, or bullae were visualized. She was discharged with an indication to continue treatment with goserelin.
We present two cases women with episodes of recurrent spontaneous right pneumothorax, identificated as catamenial. Catamenial pneumothorax is usually unilateral, occurring mostly in the right hemithorax, although it can occur on the left or be bilateral [4-6]. The aetiology of catamenial pneumothorax is still unknown, but there are several theories that try to explain the mechanisms that lead to it. Rossi and Goplerud in 1974, in their hormonal theory, claimed that high levels of Prostaglandin F2 during ovulation lead to vasospasm, with consequent ischemia, and bronchospasm, responsible for alveolar rupture [1,4-6,11]. Blebs and/or bullae can be more susceptible to rupture during menstrual-related hormonal changes [6]. However, it was also found that continuous use of non-steroidal anti-inflammatory drugs did not prevent relapses and that this theory would not justify the prevalence of the right side [10]. Another theory based on an anatomical explanation defends that dissolution of the cervical mucus plug during the menstrual period allows communication between the peritoneal cavity and the external environment. Air migrates through the fallopian tubes into the abdominal cavity, and from there through fenestrations or congenital diaphragmatic defects into the pleural space. Since those defects are more frequent on the right, this theory justifies the right hemithorax prevalence found in the literature and the low rate of pneumothorax recurrence after surgical correction of the defects [1,4-6,11]. There are reported cases of postpartum and postcoital catamenial pneumothoraces that also help to support this hypothesis [1,4].
The migration theory advocates the migration of endometrial tissue from the uterus through the peritoneal flow into the subdiaphragmatic space. The cyclic necrosis of these diaphragmatic implants produces defects that allow the passage of endometrial cells into the thoracic cavity. Due to the preferential flow of peritoneal fluids through the right paracolic gutter, most endometrial tissue migrates to the right hemidiaphragm [6,8]. Resulting from the cyclic necrosis of implants in the visceral pleura, alveolar rupture may occur [1,4,11].
The metastatic theory defends that occur transdiaphragmatic migration of endometrial tissue through the peritoneal cavity into the pleural space via transdiaphragmatic, hematogenous lymphatic or congenital diaphragmatic fenestrations [1,4], with subsequent necrosis of those endometrial foci in the proximity of visceral pleural causing air leak [6]. Some studies show a high prevalence of diaphragmatic defects (50-62.5%) [10].
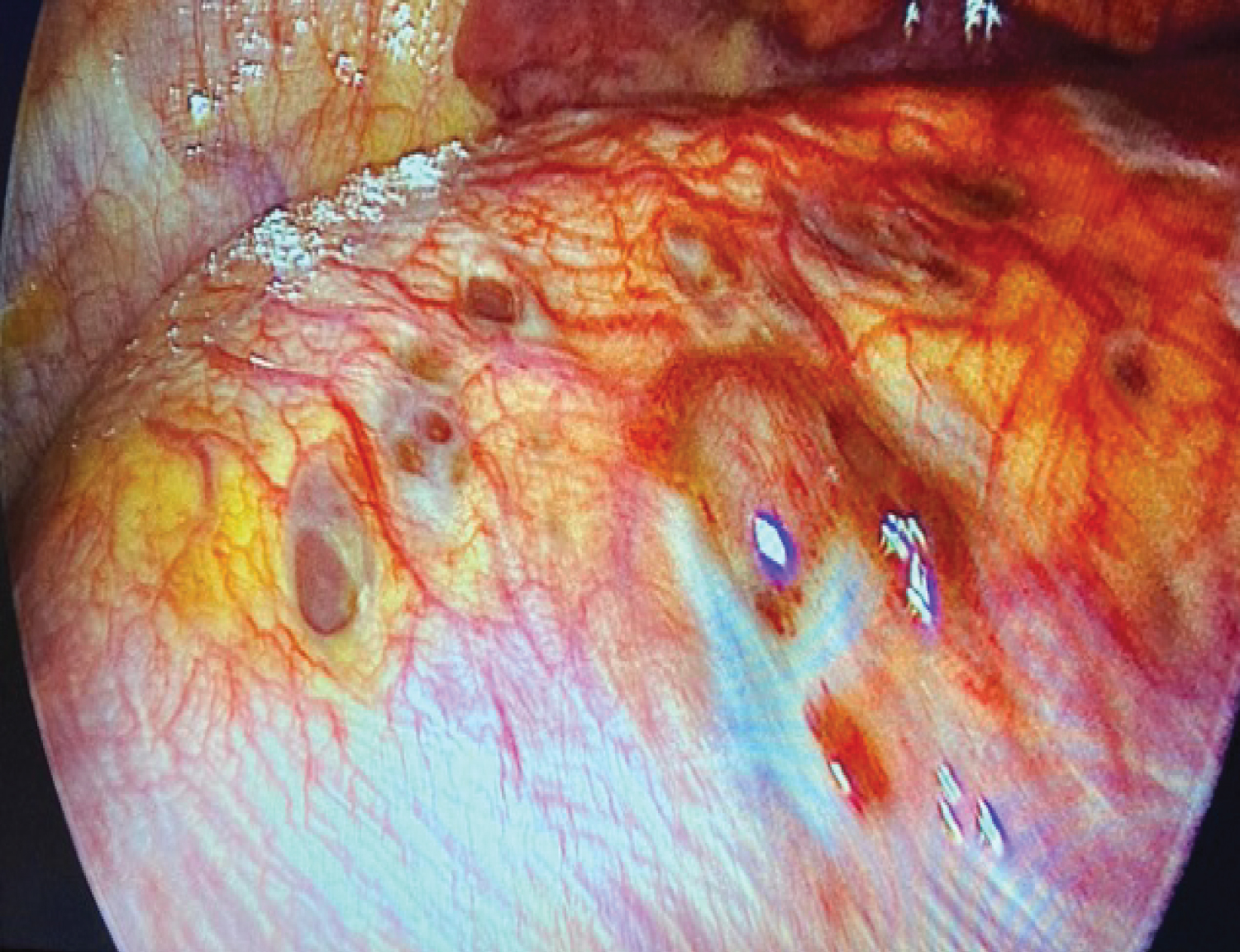 Figure 1: Intraoperative findings of the 2nd patient. Multiples diaphragmatic fenestrations. Liver can be seen underneath the perforations.
View Figure 1
Figure 1: Intraoperative findings of the 2nd patient. Multiples diaphragmatic fenestrations. Liver can be seen underneath the perforations.
View Figure 1
In endometriosis occurs an increase in the levels of CA-125. Although not specific, it can guide the suspicion towards an earlier diagnosis. CA-125 is a tumour marker used in the monitoring of ovarian cancer, although it can be elevated in several benign conditions [1,4,6].
These two women were submitted to VATS, that are described in the literature as the preferred approach [5]. In both cases, endometriosis was not seen, there was only evidence of diaphragmatic fenestrations that suggested the diagnosis.
The absence of findings frequently during videothoracoscopy makes catamenial pneumothorax an underdiagnosed entity [1].
Treatment involves surgery (pulmonary resection, pleurectomy, chemical or mechanical pleurodesis and diaphragmatic reconstruction) and hormonal therapy [1,4,7].
A high recurrence rate has been documented with the use of hormone therapy or surgery alone. Post-surgical recurrence is reported to be, depending on the study, 8 to 40%. and may happen several years after the first episode [2,3,6].
Hormonal therapy with gonadotropin-releasing hormone is important to prevent recurrence, inducing hypogonadotropic hypogonadism and amenorrhea after surgery, for at least 6 to 12 months [4,6,7,12,13].
Catamenial pneumothorax is an entity described as rare, although it is responsible for a large number of spontaneous pneumothorax. For this reason, we should suspect of it in women of reproductive age, with suggestive history and recurrent pneumothorax, even in absence of symptoms related to pelvic endometriosis.
Conservative treatment is insufficient. VATS allow better visualization of the pleural space and diaphragm. Considering the high frequency of diaphragmatic abnormalities, early surgical exploration should be pursued in these patients. Hormone therapy after surgery is responsible for reducing the recurrence rate.
One year after surgery and continuous hormonal therapy our patients remain asymptomatic and without recurrence of pneumothorax.