Calcium pyrophosphate deposition (CPPD) disease is caused by calcium pyrophosphate (CPP) crystal deposition in the fibrocartilage. It usually presents as monoarticular deposition but can deposit in multiple joints presenting as chronic polyarticular disease mimicking rheumatoid arthritis (RA), known as pseudo-rheumatoid arthritis, making it very challenging for the correct diagnosis. We are presenting a case of a 64-year-old female presented with chronic polyarticular disease refractory to disease-modifying antirheumatic drugs (DMARDs) therapy that developed multiple extensor tendon ruptures. She underwent surgery, and pathology confirmed CPPD. Association of pseudo-rheumatoid arthritis with tendon ruptures is described previously but is rare. Therefore, more research is necessary to understand the pathophysiology and clinical presentation.
Calcium pyrophosphate deposition, Calcium pyrophosphate, Pseudo-rheumatoid arthritis, Tendon ruptures
CPPD: Calcium Pyrophosphate Deposition; CPP: Calcium Pyrophosphate; CCAL1: Chondrocalcinosis 1; CCAL2: Chondrocalcinosis 2; PPi: Inorganic Pyrophosphate
Calcium pyrophosphate deposition (CPPD) disease is caused by calcium pyrophosphate (CPP) crystals in the fibrocartilage. The risk factors associated with CPPD are age, primary osteoarthritis (OA), consequences of mechanical trauma, familial predisposition such as mutation in the genetic locus chondrocalcinosis 1 (CCAL1) and chrondrocalcinosis 2 (CCAL2), hyperparathyroidism, long-standing hypermagnesemia, hypophosphatasia, and hemochromatosis [1-3]. Patients usually are asymptomatic but may present with acute onset of monoarticular arthritis with higher incidence among older adults. However, five percent of patients with CPPD can manifest with a chronic polyarticular, symmetric joint distribution mimicking seronegative rheumatoid arthritis (RA) called pseudo-rheumatoid arthritis [4]. Patient with this condition has chronic low-grade inflammatory arthritis in writs, metacarpal phalangeal joints (MCP), and spare proximal interphalangeal (PIP) and metatarsal phalangeal joints (MTP) [5]. Patients present with synovial thickening and elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) but negative rheumatoid factor (RF). The pathophysiology is not well-known but consists of deposition of inorganic pyrophosphate (PPi) formation from extracellular adenosine triphosphate (ATP) that combines with calcium deposition in articular cartilage vesicles [1]. Different factors that play important role for the homeostasis of PPi may contribute with more formation and deposition of the crystals [4]. The mutation in the transmembrane pyrophosphate transporter called ANKH (the human homologue to the mouse progressive ankylosis protein) increases the transport of pyrophosphate from chondrocytes into cartilage [3]. The overactivity of ectonucleotide pyrophosphatase/phosphodiesterase 1 (ENPP1) and ENPP3 generates more intracellular and extracellular PPi via hydrolysis of ATP [6,7]. Another mechanism is the lack of alkaline phosphatase (ALK) or the abnormal function [8]. The ALK has the function to disintegrate the PPi and uses the magnesium (Mg++) as cofactor. However, the high level of iron, calcium, and cooper inhibit the function of ALP [9]. Besides, the increase of previous minerals mentioned, the low level of Mg++ enhances the nucleation of CPP crystals in cartilage.
The diagnosis is based on a synovial-fluid finding of positively birefringent, rhomboid-shaped crystals in compensated polarized light microscopy and calcification of the cartilage or capsule on imaging [10]. The most common sites for deposition are knees, hands, wrist, and pelvis (larger synovial joints). Less frequently, CPPD can deposit in the synovial lining, ligaments, tendons, and periarticular soft tissues [11]. It is necessary to rule out metabolic conditions such as hyperparathyroidism, hemochromatosis, hypophosphatasia, hypomagnesemia, and hypothyroidism, particularly in young patients with polyarticular manifestation [12]. We are presenting a case report of a female patient with pseudo-rheumatoid arthritis with multiple hand extensor tendon ruptures who required numerous surgical treatments.
A 64-year-old female with unremarkable past medical history presented in our office with multiple swelling involving both dorsal hands over the last 2 months. The patient noticed having 5-10 minutes of morning stiffness, tenderness, and swelling in both hands, with decreased range of motion with minimal improvement with ibuprofen 800 mg daily. The patient denied acute injury, recent weight loss, Raynaud's phenomena, eye pain, oral ulcers, gastrointestinal complaints, or rash. On physical exam, a bony hypertrophic enlargement was noticed in the right 2nd finger distal interphalangeal (IP) joint and mild swelling in right 3rd, 4th, 5th metacarpophalangeal (MCP) joints with limited extension consistent with synovitis. Laboratory shown as noticed in Table 1. Subsequently, the next two days patient experienced the inability to extend her right 4th and 5th MCP joints and left 5th MCP joints consistent with tendon rupture (Figure 1). Due to the polyarticular distribution and multiple tendon ruptures, the patient was started on methotrexate 5 mg once weekly for possible seronegative rheumatoid arthritis (RA). Arthrocentesis was not possible due to the size of the joint and ongoing tendon ruptures. The patient was referred to orthopedics. Magnetic resonance imaging (MRI) of both hands showed hyperintense structures in the carpometacarpal (CMC) joint and 4th MCP joints (Figure 2). The patient underwent right-hand tenosynovectomy and tendon debridement of partial tears of the long finger extensors. The pathology report showed synovial hyperplasia, chronic lymphocyte-predominant perivascular inflammation, and positively birefringent crystals on polarization suggestive of calcium pyrophosphate dihydrate crystals (CPPD). The patient underwent additional surgery to repair the rest of the tendon (Figure 3). The patient started on colchicine 0.5 mg twice a day with subsequent symptom improvement. Laboratory for hemochromatosis and Wilson's disease were negative.
 Figure 1: (A) Left hand with 5th finger tendon rupture (red arrow); (B) Right hand with 3rd, 4th, and 5th fingers tendon ruptures (orange arrows).
View Figure 1
Figure 1: (A) Left hand with 5th finger tendon rupture (red arrow); (B) Right hand with 3rd, 4th, and 5th fingers tendon ruptures (orange arrows).
View Figure 1
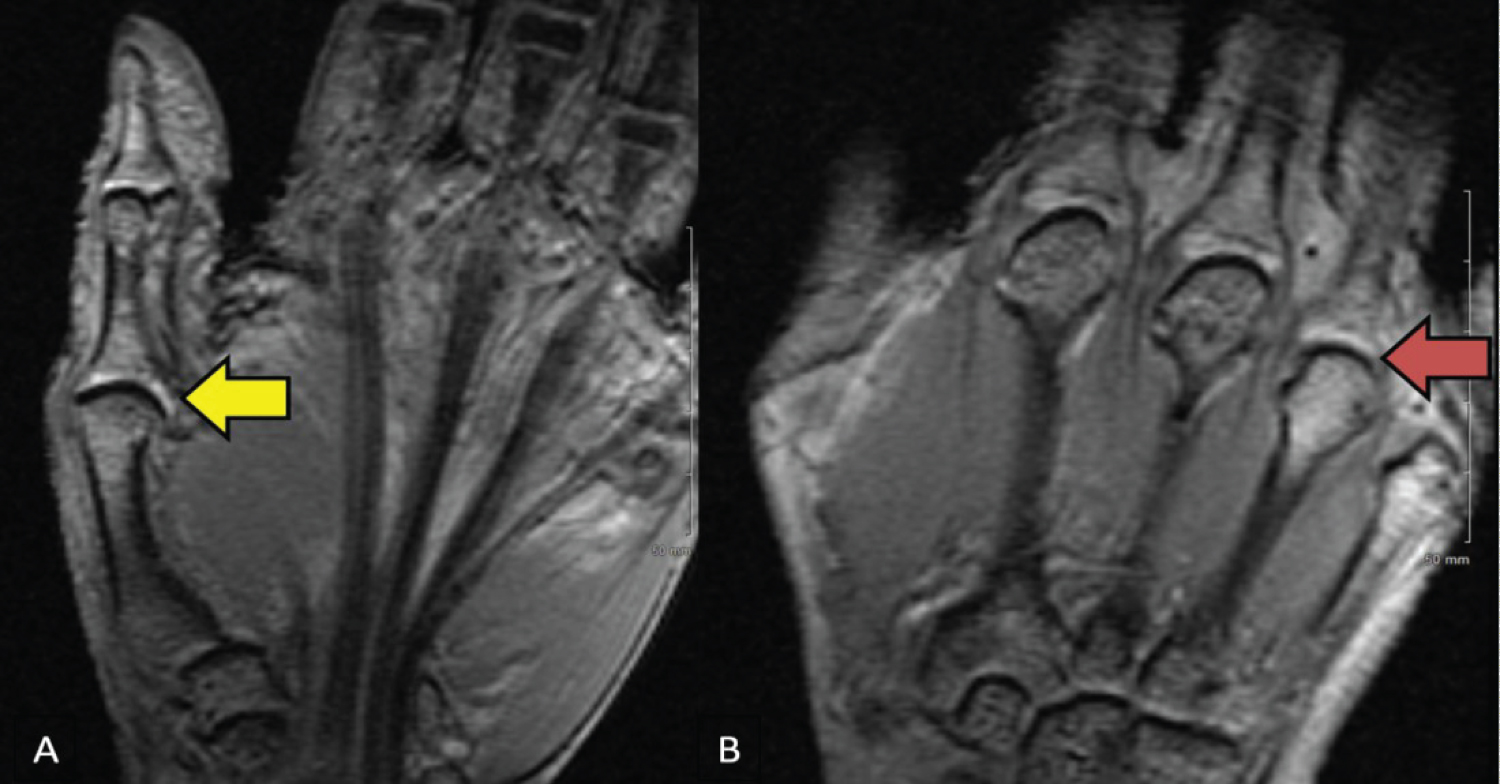 Figure 2: MRI of the left hand: (A) Yellow arrow pointed a T2 hyperintense structure along the medial aspect of the first CMC articulation, which measure approximately 11 × 3 × 3 mm. This may represent a small ganglion. Mild edema is demonstrated along the volar aspect of the base of the first metacarpal, likely related to adjacent degenerative etiology; (B) Red arrow pointed T2 hyperintense structure along the medial aspect of the fourth MCP articulation, which measure approximately 8 × 3 × 3 mm.
View Figure 2
Figure 2: MRI of the left hand: (A) Yellow arrow pointed a T2 hyperintense structure along the medial aspect of the first CMC articulation, which measure approximately 11 × 3 × 3 mm. This may represent a small ganglion. Mild edema is demonstrated along the volar aspect of the base of the first metacarpal, likely related to adjacent degenerative etiology; (B) Red arrow pointed T2 hyperintense structure along the medial aspect of the fourth MCP articulation, which measure approximately 8 × 3 × 3 mm.
View Figure 2
 Figure 3: Left hand 5th finger tendon repair (blue arrow) and right with 3rd, 4th, and 5th fingers tendon repair (green arrows).
View Figure 3
Figure 3: Left hand 5th finger tendon repair (blue arrow) and right with 3rd, 4th, and 5th fingers tendon repair (green arrows).
View Figure 3
Table 1: Laboratory result. View Table 1
Tendinitis and tenosynovitis secondary to CPP crystals have been shown in triceps, hand flexors, extensors, and Achilles tendons [13]. There are very few reports about multiple extensor tendon ruptures secondary to CPPD [14-18]. The mechanism is unknown, but the deposition of CPPD can be localized in the tendon sheath, which is more frequent in the small joints of the hand and foot [15]. The calcium deposits in the sheath decrease the laxity of the tendon, provoking a rupture secondary to mechanical force rather than inflammatory factors. As a rheumatologist, a patient presents with bilateral hand hypertrophy with deformity, and tendon rupture increases the likelihood for RA. However, CPPD should be considered as a possible differential diagnosis in patients resistant to disease-modifying antirheumatic drugs (DMARDs). Therefore, arthrocentesis is critical to making the correct diagnosis and preventing further complications such as tendon rupture. Unfortunately, due to the limited size of the DIP and MCP joints, we were not able to perform arthrocentesis in our patient. We realized during our literature search limited case report and guidelines, and we believe more research about pathophysiology and better descriptions of pseudo-rheumatoid arthritis are necessary.
Pseudo-rheumatoid arthritis is not well-described pathology and is considered a great mimicker of RA. Hence, a rheumatologist and the general clinician should be aware of the clinical presentation and keep in mind as a differential diagnosis. A rapid diagnosis is crucial to prevent further complications such as tendon rupture. Therefore, a DMARD treatment-refractory or atypical tenosynovitis should be considered for arthrocentesis.
The data sharing is not applicable to this article as no new data were created or analyzed in this study.
No funding was involved in this publication.
No conflict of interest (COI) was declared.
Consent was obtained and saved at Northeast Georgia Medical Center.
YMC retrieved and corroborated the data. YMC, and BF, collaborated in the discussion. BF, and LJ collaborated in the internal review and proofreading. All authors contributed to manuscript revision, read, and approved the submitted version.