Background: In malaria-endemic regions like Ghana, success in combatting the disease hinges on information accessibility and individual decision-making. The emergence of commercial herbal remedies for malaria treatment, along with the channels through which people acquire this knowledge, holds significant weight. Individuals play an active role in choosing between herbal and conventional antimalarial drugs, such as artemisinin combination therapy. These decisions are heavily influenced by information sources and personal perspectives.
Method: A cross-sectional survey was conducted across three densely populated Ghanaian cities to assess the sources of herbal medicine information, preferences and opinions of individuals on malaria health seeking options, in the era of commercial herbal antimalarials. Opinions about malaria treatment options were analysed thematically while the choice of treatment option and venue and the influence of gender on these choices were analysed through frequencies and statistical comparison of means respectively.
Results: Results revealed that television was the primary source of herbal medicine information, closely followed by radio, emphasizing the pivotal role of multimedia platforms. Ghanaians showed a marked preference for seeking malaria treatment at hospitals and drugstores, in line with Ghana Health Services guidelines. ACTs were the favoured drug option, followed by herbal preparations. Gender dynamics were also shown to influence treatment venue and drug choice selection. This study also revealed potential risks associated with the alternate, unprescribed use of herbal antimalarials for things like malaria prophylaxis and emergency contraceptives.
Conclusion: These findings of this research reveal the pivotal role of multimedia in spreading information on herbal medicine as well as some misconceptions and misuses herbal and allopathic medicines. There is the need for targeted interventions and educational initiatives, addressing these nuanced perspectives, considering gender, to effectively combat malaria.
Malaria, Herbal medicine, Allopathic medicine, Opinions
HP: Herbal Preparation; ACT: Artemisinin Combination Therapy
Ghana, an endemic region for malaria, transitioned from chloroquine to Artesunate-Amodiaquine combination in malaria treatment in 2004 [1]. Success of this shift hinges on public adoption. However, some still resorted to chloroquine [2] and herbal remedies [3], signifying a preference for alternative treatments. In Ghana, herbal anti-malarials, evaluated and approved by the Food and Drugs Authority, complement allopathic drugs like artemisinin combination therapy (ACT) [3].
The venue for treatment of malaria plays a crucial role even in choice of antimalarial drug. The Ghana Health Services (GHS) guidelines permit antimalarial purchase after a positive Rapid Diagnostic test, allowing treatment in pharmacies, licensed drug stores, and herbal shops [4]. Fenny, et al. [5] demonstrated that 48% of uninsured Ghanaians preferred informal care for malaria, often bypassing hospitals due to accessible over-the-counter drugs. Despite endemic awareness of malaria symptoms and its association with mosquitoes, individuals opt for proximity to home in choosing treatment locations [6].
When it comes to the drug for treatment, studies reveal a fluctuation in antimalarial preference between traditional/herbal and allopathic/western medicine. For instance, in Ivory Coast, both approaches were employed, sometimes in combination [7]. In Nigeria, Okwa, et al. [8] found varying preferences for artemisinin-combination therapy (ACT) drugs, with Amatem and p-alaxin being favoured. Additionally, about 80% of respondents utilized local herbs. In Ghana, Yeboah, et al. [4] reported a preference for herbal medicines over Western medications. Notably, in this study, herbal medicines refer to commercially prepared antimalarials sold in Ghana, distinct from locally sourced and prepared herbs [3].
Individuals in Ghana have the autonomy to choose between herbal and allopathic medicines, both accessible without a prescription [9]. Eventhough the official antimalarial drug policy recommends the use of atermisin-based combination therapy [1], there is flexibility in the choice of treatment and venue [4] especially with the wide range of herbal medicines approved for treatment malaria treatment by the Ghana Food and Drugs Authority (FDA) [3]. This choice impacts their healthcare-seeking behavior, potentially influencing the effectiveness of national malaria policies. Understanding Ghanaian preferences for treatment venues and opinions on antimalarials, especially herbal options, is paramount for effective policy implementation.
A cross-sectional survey was chosen to assess malaria health seeking patterns of Ghanaian adults [10-12] to assess the following research questions
1. Where do Ghanaians receive information on herbal antimalarial drugs?
2. Where do Ghanaians go for treatment when they suspect Malaria?
3. Which drugs do Ghanaians prefer for treating suspected malaria?
4. What are Ghanaians’ opinions about allopathic antimalarial medicines?
5. What are Ghanaians’ opinions about herbal antimalarial medicines?
The target population for this study included all adults in Ghana, while the accessible population consisted of adults from three regional capitals: Cape Coast (Central Region), Takoradi (Western Region), and Accra (Greater Accra Region). These regions were chosen because of large population densities and their capital cities, being metropolises were places of interaction between Ghanaians from different backgrounds. In Cape Coast, surveying was done at the New Site (Science), Abura, Pedu, Kotokoraaba, and Apewusika suburban areas. In Takoradi, the areas used for the survey included the Pipe Ano, Market circle areas. In Accra, surveying was done around Korle Bu, Mamprobi and Chorkor areas (Figure 1).
 Figure 1: Map of Ghana showing cities survey was conducted in. (Source: Remote Sensing and Cartographic Unit, University of Cape Coast, 2013).
View Figure 1
Figure 1: Map of Ghana showing cities survey was conducted in. (Source: Remote Sensing and Cartographic Unit, University of Cape Coast, 2013).
View Figure 1
Conducted between 2013 and 2014, the sample size was determined based on the 2010 Ghanaian population census and at the time the Central, Western and Greater Accra regions had populations of 1,108,800, 1,149,408 and 2,025,637 respectively, accounting for a total of 4,283,845 individuals [13]. The sample size was calculated on the accessible population using Cochran’s formula (1963), [14]
Where n 0 is the sample size , Z is the confidence level at 95% (standard value 1.96), e is the margin of error at 5% (standard value 0.05), and p in this case is 0.5. This resulted in a sample size of three hundred and eighty-four (384) individuals.
The survey was open and gender-neutral, excluding participants under 18-years-old. A systematic sampling approach was employed, involving every third person or individuals in every second open store at the street level. At the neighbourhood level, every other house was selected. The study's nature and purpose was explained to individuals selected to respond to the questionnaire. Those who agreed to participate were provided with a questionnaire for completion. For literate respondents, a consent form was provided for their signature. Some literate individuals were given the questionnaire to fill at their own pace and collected at a later date.
For illiterate respondents, an audio recording of their agreement was noted. The questionnaire was then read out loud and their responses were translated to English and written down by researcher. Open ended responses were either written down by respondents themselves or with their permission, by the researcher.
The instrument for the study was a questionnaire developed to assess the health seeking habits of Ghanaians but was part of a larger study with results published in [3]. As such, the full instrument included other items outside of the scope of this paper’s research objectives. The questionnaire tackled among other things, the demographics of the participants (age, gender), the preferred malaria treatment venue, preferred antimalarial drug, sources of herbal antimalarial information, opinion on allopathic medicines and opinions on herbal medicines. Preference for treatments/venues and sources of information were assessed by providing options for individuals to tick or indicate. Any extra options were indicated by Opinions on either allopathic medicines or herbal medicines were assessed through open ended questions.
To assess the association between gender and treatment drug or treatment venue the Monte-Carlo exact test was used. This test was chosen ahead of the standard chi-square test because the assumptions were violated as more than 20% of the table cells had expected cell frequencies less than 5 [15].
The z-test was then used to compare the proportions of males against females who chose a particular “antimalarial treatment” or “treatment venue”. The z-test allows for comparisons of proportions from independent samples. It was done to ascertain whether a particular gender chose a specific option significantly more than the other. This adds value to the Monte-Carlo exact chi-square test which would simply determine whether or not there is a significant difference in their choices but won’t identify whether frequencies of a specific choice are significantly different between females and males. Consequently, a confidence interval of 95% was employed.
Thematic analysis was also employed to assess opinions about herbal antimalarials and allopathic drugs. Thematic analysis is a method detecting, examining, structuring, elucidating, and communicating recurrent themes observed within a specific dataset [16]. As such, unlike content analysis, another similar method of qualitative analysis, which often converts qualitative data into counts, thematic analysis only reveals the themes and patterns in qualitative data [16].
Overall, due to a low response rate and a difficulty in tracing some of the participants to return the questionnaires, 344 questionnaires were filled by respondents (Table 1). Of that number, 182 were male and 162 were female. However not everyone answered all the questions in the questionnaire. As such, for every item, the total number of respondents is indicated.
Table 1: Gender demographics of study respondents. View Table 1
The means through which participants were introduced to these herbal medicine was also investigated. The most popular source of herbal prepartion/medicine (HP) information was the Television followed by the radio, friends, vehicular advertising, drugstores, billboards and door to door advertising (Table 2).
Table 2: Sources of herbal information. View Table 2
With reference to perceived malaria, the treatment option for malaria greatly depends, in this part of the world, on the venue from which treatment is sought. The most patronized malaria treatment venue was the hospital followed by the drugstore. The frequency at which participants chose a particular venue is presented in Table 3.
Table 3: Respondents' preference for malaria treatment venue. View Table 3
Respondents’ preference for a treatment venue as influenced by their gender was also assessed. A greater number of male respondents, 173, were obtained for this question than females who numbered at one hundred and fifty four (154) (Table 4). Across both genders however the most popular treatment venue was the hospital, followed by the drugstore.
Table 4: Cross tabulation of gender and malaria treatment venues. View Table 4
A Monte-Carlo’s exact test of Pearson ’s chi-square was conducted to assess whether there was an association between gender and treatment venue. It revealed a significant p-value of 0.002 (at 99% CI, two-tailed, of 10,000 samples) which meant that the means of the two samples, males and females differ about their means for choice of a malaria.
In order to assess whether the choice of one of the two most popular treatment venues, hospital and drugstore, by the two genders was significantly different, a z-test was performed. It revealed that females chose hospital significantly more (z = - 3.083, p = 0.002, two-tailed) than males, who chose the drugstore significantly more (z = 3.642, p = 0.002, two tailed) than females.
Respondents were also asked questions pertaining to their patronage and perceptions about the various antimalarial options available to them. Table 5 shows the respondents’ antimalarial drug preference for every respondent that answered the relevant question. The frequency at which participants chose a particular antimalarial drug was then also expressed as a percentage of the total frequency.
Table 5: Drugs for malaria treatment. View Table 5
Respondents’ choices for antimalarial drugs were also assessed across Gender to ascertain whether choice for a particular drug varied as according to gender. A greater number of male respondents, 162, were obtained for this question than females who numbered at one hundred and forty-five (145). Across both genders however the most popular antimalarial drugs were the ACTs (Table 6).
Table 6: Cross tabulation of gender and antimalarial drug choices. View Table 6
A Monte-Carlo’s exact test of Pearson ’s chi-square was conducted to assess whether there was an association between gender and antimalarial drug. The test revealed a significant p-value of 0.000 (at 99% CI, two-tailed, of 10,000 samples) which means that there is a significant difference in between choice of males and females for an antimalarial drug.
In order to assess whether the choice of one of the two most popular treatment drugs, ACTs and HPs, by the two genders was significantly different, a z-test was performed. It revealed that females chose ACTs significantly more (z = -4.551, p = 0.002, two-tailed) than males. Males also preferred HPs significantly more than females (z = 1.9986, p = 0.0455, two tailed).
This response was open-ended and as such the results were analysed by thematic analysis. Overall, 152 respondents provided responses to the questions on the opinions on herbal and allopathic antimalarials. Several themes were obtained in this analysis. Overall, the opinions of herbal medicines were either “positive” or “negative”.
Positive opinions about herbal antimalarials were centered on their effectiveness, side-effects, prophylactic use and alternate use.
Effectiveness: On its effectiveness, respondents were noted for saying things like
“Herbal medicines tend to be more effective compared to orthodox medicines."
Or things like,
“Because(herbal medicine) it cures you easily and well"
Some respondents believe herbal medicine is not only effective against malaria but even more so than allopathic medicines. However, caution is advised. Wilmot, et al. [3] caution that out of five commonly used herbal preparations in Ghana, only one demonstrated efficacy, albeit less effective than the standard ACT. Research has confirmed the effectiveness of certain herbs against malaria, like Xylopia aethiopica and Haematostaphis barteri [17,18], but caution is still advised. Komlaga, et al. [19] noted varying levels of efficacy and even cytotoxicity in plants evaluated for malaria treatment. This underscores the need for proper public health education and monitoring in Ghana, as perceptions of herbal medicine's efficacy over allopathic medicines may not always be accurate.
Side effects: On the side effects, respondents expressed that herbal medicines had little to no side effects in comments like,
“it (herbal medicine) cures malaria quick without any side effects.”
Or comments like,
“it (herbal medicine) has no side effects.”
This means for some Ghanaians, their main concern was the side-effects of the antimalarial drug there were choosing. And for herbal medicine, some believed it had no side effects. This sentiment has also been reported by Aziato and Antwi [20] who noted that Ghanaians prefer herbal treatments for malaria because they perceive it has fewer side-effects despite reports identified side-effects [4,21]. This perception may persist because of an affinity people have towards anything that is branded natural [22]. In Ghana, the food and drugs board assesses the toxicity of these herbal preparations [3], but perhaps stricter laws must be put in place to check advertisement of false uncertified herbal medicines [23] with hidden side-effects.
Prophylactic use: On prophylactic use, one respondent remarked,
“I don't wait to have malaria; I take one cup (pointing to a jug of a herbal concoction) every day in the morning"
This means some respondents were taking herbal medicine regularly in an attempt to prevent malaria infection. This has been noted in earlier studies like Idowu, et al. [24] and Okello and Kang [25] in Uganda. Similarly, a comment by a respondent in Appiah’s, et al. [26] study showed that the respondent was taking the herbal mixture daily for malaria prevention. This signifies a potential of herbal antimalarials, particularly those that have been evaluated for safety to be evaluated for use in malaria prophylaxis.
Alternate use: On the alternate use of herbal antimalarials, one respondent indicated,
“The one that says not safe for pregnant women. I use that one for when it (menstrual cycle) passes”
This opinion indicates that individuals were taking herbal medicine for other reasons than what they are indicated for. In this case, the herbal medicines that had warnings for pregnant women were being taken as emergency contraceptives. Beyond any risk that may be posed to the health of the pregnant women themselves, some of these drugs with such labelling may actually present teratogenic effects to the foetus [27]. This presents a potential public health risk if correct education is not provided regarding the proper, certified use of these herbal medicines.
Negative opinions about herbal antimalarials were also centred on their effectiveness, side-effects, dosage, certification, and taste.
Effectiveness
With regards to the effectiveness some of the comments were about how long the medicines take to be effective
“I don't prefer herbal medicine because it takes a long time."
Or comments like,
“[Herbal Medicine] Takes time to work. Sometimes it takes 2 or 3 bottles to clear malaria”.
This opinion shows that some Ghanaians were concerned with the duration it takes for some of these herbal medicines to clear the symptoms of malaria. This demonstrates also that some respondents are possible abusing large quantities of herbal medicines to cure the disease.
Other respondents on the hand, simply believed herbal antimalarials were not efficacious. Some respondents said
"herbal medicine …..does not completely cure the disease"
While others said,
"with herbal medicine the malaria symptoms come back"
These respondents' statements highlight diverse concerns under the efficacy of herbal medicines. While some were concerned about the complete eradication of malaria, others were also alluded to the potential for symptom recurrence with the administration of herbal antimalarials. This has also been noted by Wilmot, et al. [3] who noted that some of the commercial herbal medicines do not actually clear malaria parasites. This sentiment indicates that some Ghanaians are educated about the uncertainty regarding herbal medicine efficacy.
Side-effects: On the side effects of herbal medicines, some intimated that they didn’t like herbal medicines because the side-effects are unknown. As a respondent indicated,
“I do not like them [herbal medicines] because they don't indicate the side effects of the drug”
This reveals a prevalent concern among respondents regarding the uncertainty surrounding the potential side effects of herbal medicines. The lack of clear information about possible adverse effects is cited as a factor influencing their preference for herbal antimalarial drugs.
Others communicated clear side-effects of herbal medicines saying,
“it is a laxative”
Or they indicated,
“I hear they are toxic (liver damage)"
This finding highlights the concerns with the side-effects of herbal medicines, with some respondents pointing out specific known, damaging side-effects, such as the potential laxative effect or concerns about possible toxicity leading to liver damage. Liver damage with herbal supplements and medicines has also been demonstrated by Rossi and Navarro [28] and Navarro, et al. [29]. Other specific side effects have been noted such as blocked/ringing ears, blurred vision, itching, nausea and general body weakness by Yeboah, et al. (2022).
Dosage: On the dosage of herbal medicines they indicated that the dosages were not known. Some said,
"Dilutions/Dosage [of Herbal medicines] not clear"
While others said
"Not precise as to [information on] dosage and storage"
These opinions reveal a common concern among respondents regarding the lack of clarity surrounding dosage instructions for herbal medicines. Some expressed uncertainty about dilutions and dosage, while others noted a lack of precision in information provided regarding dosage and storage. Appiah, et al. [26] also noted then when it comes to dosage with herbal antimalarials, the dosage is unspecific and seems to be decided by the pursing taking the remedy and not necessarily a standardized, tested dosage. This practice reflects a public health loophole and a potential source of some of disease from damage to internal organs or other side-effects of overdose of a particular herbal remedy.
Certification: On the certification, some respondents asserted that the herbal medicines were not certified or approved. As this respondent indicated,
“some[herbal medicines] are not tested. "
While others said,
“some (herbal medicines) are not good"
Under this theme, respondents indicated a concern about certain products not undergoing testing, while others expressed misgivings about the overall quality of certain herbal remedies. These are concerns that have something to do with how these drugs are tested and certified for use either by the companies that produce it or by regulatory bodies that certify it for use. This may be so because of some of the already mentioned risks that come with herbal medicines and that are advertised and sold. Some are actually certified [3] while some are not [23].
Taste: When it comes to taste, the main complaint was that herbal medicines were bitter tasting as indicated by this respondent.
"I don't prefer [herbal medicines] because of the bitterness"
The bitter taste of these herbal medicines, while efficacious variants are a positive arsenal against malaria, seems to be a barrier in any future effort to coordinate efforts to test and prescribe any herbal remedy in Ghana. Figure 2 summarises the opinions on herbal antimalarials.
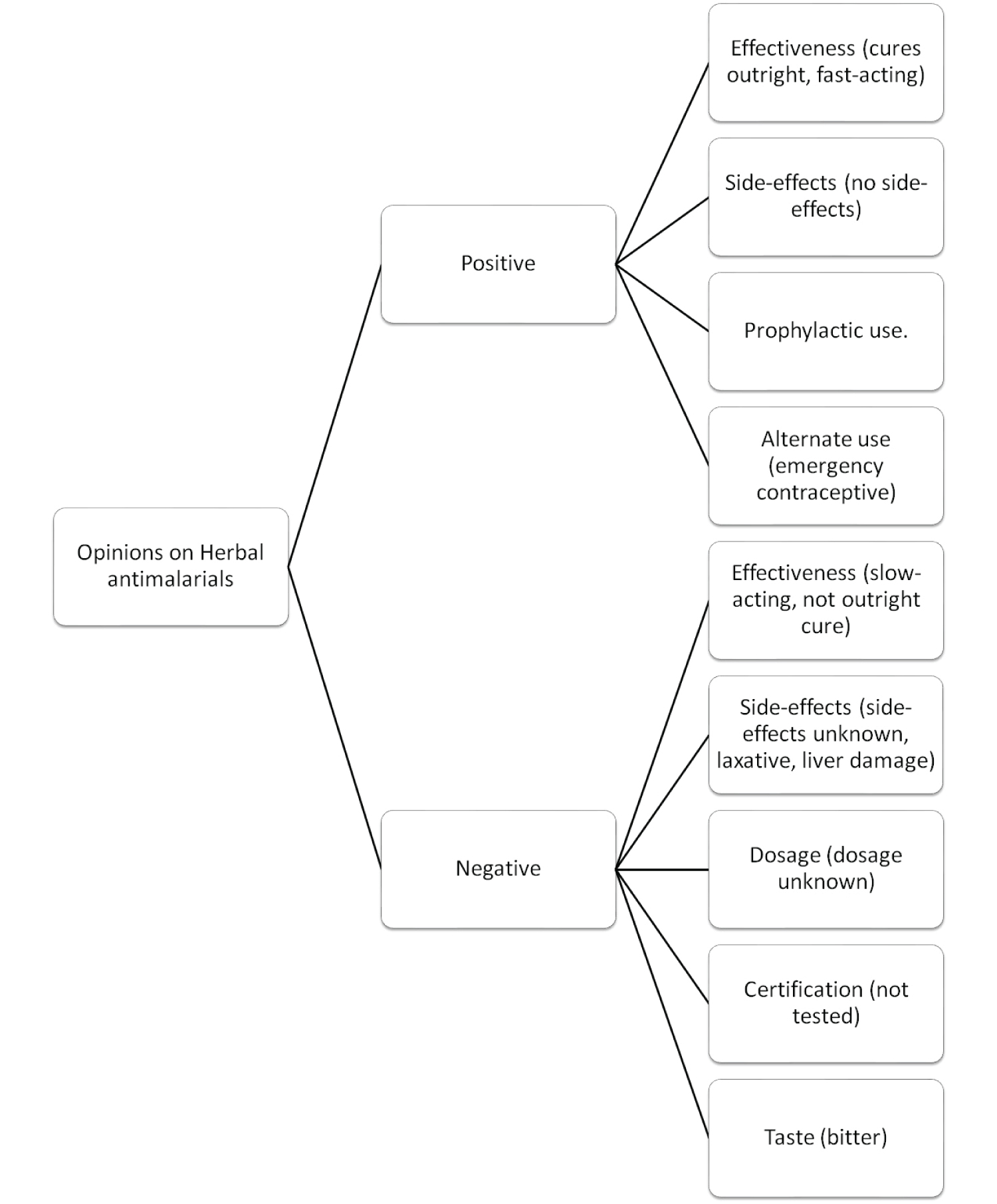 Figure 2: Opinions on Herbal antimalarials.
View Figure 2
Figure 2: Opinions on Herbal antimalarials.
View Figure 2
This response was open-ended and as such the results were analyzed qualitatively by thematic analysis. Several themes were obtained in this analysis. Overall, the opinions of allopathic medicines were either “positive” or “negative”.
Positive opinions about allopathic antimalarials: The positive opinions about allopathic antimalarials centred on the certification, effectiveness, dosage and side-effects of allopathic antimalarials.
Certification:
On certification, respondents indicated that allopathic antimalarials are recommended by government. One respondent indicated,
“Because that [allopathic medicine] is what is recommended by the government.”
Or another who said,
“They do (safety) tests [on allopathic medicines]. Prescription based administration. "
Respondents were of the opinion that allopathic antimalarials are recommended by government and subject to rigorous safety testing and regulated administration protocols. This acknowledgment of government endorsement and stringent safety tests seems to suggest that some Ghanaians have a trust and confidence in the use of allopathic medicines for malaria treatment, underscoring their perceived reliability and efficacy.
Effectiveness:
On effectiveness, some alluded that not only are allopathic antimalarials effective but that they are fast-acting. One respondent said,
“it cures malaria faster”
Another also claimed,
"I prefer malostat because it works faster for me and I don't get any complications"
Also on effectiveness, some were stating that allopathic medicines were simply efficacious. One respondent said,
“no relapse. Cures malaria completely”
From the data, respondents expressed confidence in the fast-acting nature of allopathic medicines, with specific mentions of drugs like Malostat. Malostat is a sulphadoxine pyrimethamine combination therapy drug [30]. Additionally, respondents indicated that they perceived allopathic medicines to provide complete and lasting relief from malaria, emphasizing their efficacy in treating the disease.
Dosage:
On dosage, individuals indicated that the dosage was made known to them. As this respondent indicated,
"they show the dosage …. of the [allopathic] drug. "
Similarly, respondents indicated the side-effects of allopathic medicines were made known to them beforehand. One respondent said,
"Side effects are made known to me by qualified physician."
With allopathic drugs respondents indicated that they were well-informed about the dosage and potential side effects of allopathic medicines. They noted that healthcare workers clearly explained dosage instructions, and qualified physicians specifically informed them about potential side effects. This suggests that to a degree, there is involvement of healthcare personnel and physicians in discussions of dosage of allopathic antimalarials than in discussions of herbal antimalarials. There are, in Ghana however, 55 Government hospitals with Herbal Medicine units overseen by trained Medical Herbalists whose job is to coordinate and educate Ghanaians on herbal medicine dosage and uses [31]. Perhaps these units are not well-utilized by some Ghanaians.
Negative opinions about allopathic antimalarials: There were also negative opinions about allopathic antimalarials based on their effectiveness, side-effects and constituents.
Effectiveness:
Regarding the effectiveness, respondents indicated that the allopathic antimalarials do not work outright and usually need an extra dosage of herbal medicine to clear the parasites. As shown they commented things like,
“It (allopaths) doesn't cure outright. After a full course dosage there are still lingering symptoms. So I take Herbal medicines after"
Or,
"I take Malafan but usually after a full dose course I would not have recovered. 1-2 weeks later I supplement it Masaada (a herbal antimalarial)"
Here, respondents reveal that they perceived allopathic antimalarials as not always providing immediate and complete relief. As such, some respondents supplement their treatment with herbal medicines after completing a full course of allopathic medication to address lingering symptoms, supplementing Malafan with Masaada. Malafan is a pyrimethamine and sulphadoxine combination drug [32] while Masaada is a herbal antimalarial [33]. This practice highlights the perceived complementary nature of herbal remedies, suggesting that a combination of both allopathic and herbal treatments may be preferred by some for more comprehensive malaria management.
Side-effects:
Side-effects were another point of negative opinion regarding allopathic antimalarials. Respondents communicated that allopathic medicines made them feel weak with comments like,
it (allopaths) weakens my body
or as this respondent said,
"it (allopaths)makes me feel dizzy and more sick"
Respondents reported weakness, dizziness, and increased sickness after using allopathic medicines. This reflects a belief that such medications may bring about additional symptoms and illness. Similar findings of reported symptoms have been noted by Appiah, et al. [26] and Adjei, et al. [34]. These suggest a need for proper education on the dosage and indications/contraindications of taking some of these allopathic drugs.
Constituents:
Respondents also revealed they did not like allopathic antimalarials because of their constintuents. The notion was that these drugs contained “chemicals” which respondents did not want. They indicated this by saying,
"Because of the chemical (in the allopaths)"
And a comment like,
"I try as much as possible to prevent excess chemicals"
From the data above, respondents expressed concerns about "chemicals" in allopathic antimalarials, indicating a possible lack of understanding about their composition. This highlights a potential misconception, as all substances are ultimately chemicals. The term "chemical" may evoke negative imagery, contributing to public misperception [35]. This underscores the need for comprehensive public health education, especially regarding the natural origins of many herbal medicines, such as artemisinins, which are derived from plant extracts.
Figure 3 shows a code tree of the opinions of respondents had about allopathic antimalarials.
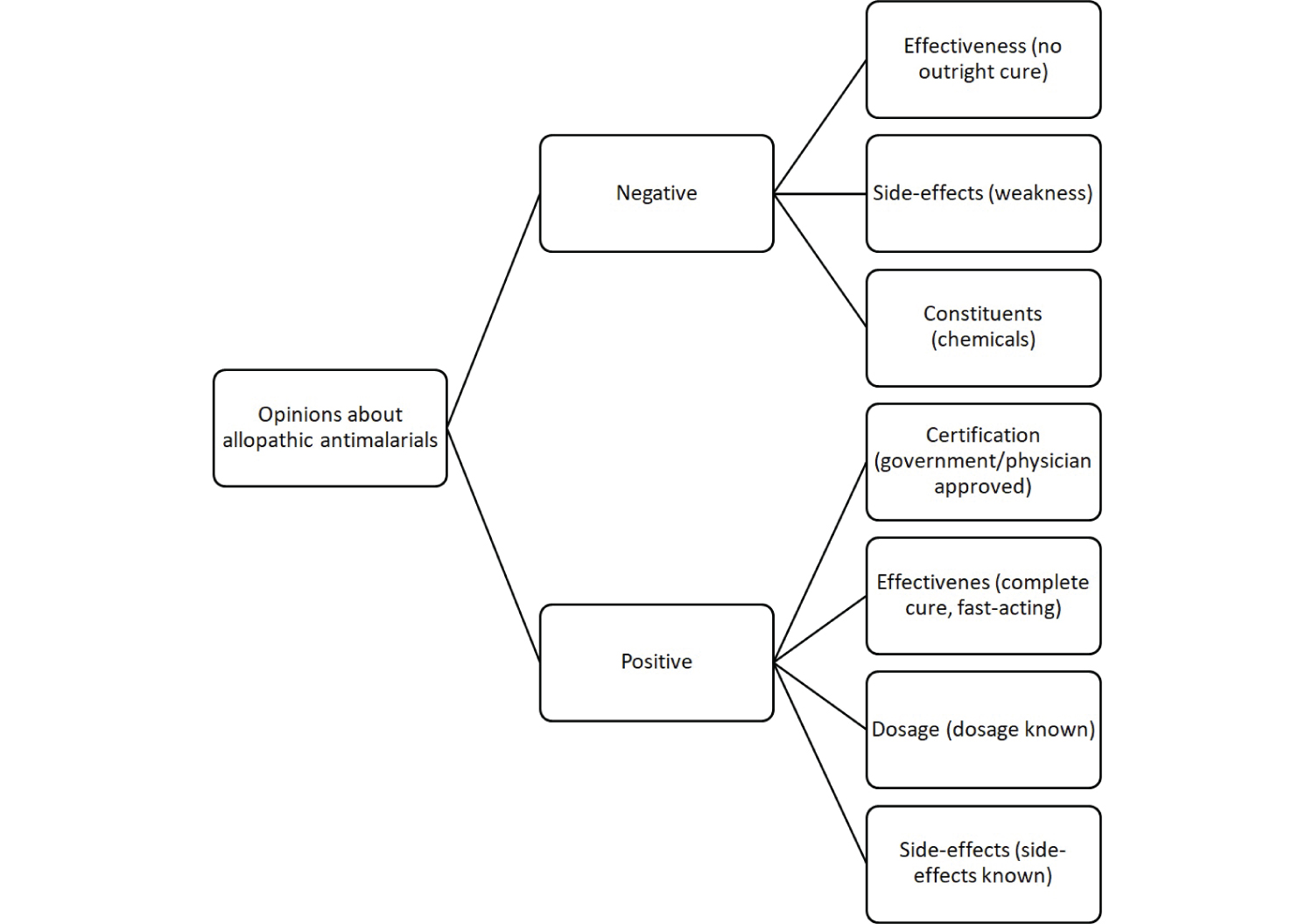 Figure 3: Opinions on Allopathic antimalarials.
View Figure 3
Figure 3: Opinions on Allopathic antimalarials.
View Figure 3
This research was conducted through a cross-sectional survey of Ghanaians on the antimalarial health seeking habits, with a focus on herbal medicine. The results are discussed below.
On the sources of herbal information, of the options provided, respondents indicated that television was primary source or herbal medicine information. This was followed by radio, friends, and vehicular advertising in that order. This suggests that multimedia plays a big role in the dissemination of health information as television and radio were higher than all other option combined. At the time of the study, between 2013 and 2014, social media was not indicated by any of the respondents as they had the chance to choose “other”. Nonetheless, other studies, like that by Munisi, et al. [36] noted that among Tanzanians, the most common source of malaria information was Television followed by radio. This has also been corroborated by Konlan, et al., [37] who reported that among indigens of Godokpe, a suburb of Ho, Ghana, the major source of malaria information was also television. Television and radio thus hold both promise and warning in the fight against malaria and proper malaria health information. For promise, it suggests that any efforts to inform or educate Ghanaians on herbal antimalarial use must be targeted through television and radio. The warning however is that any malaria health misinformation will spread like “wild-fire” on the television and radio waves if unchecked. For example, a recent expose by the Fourth Estate, an investigative journalism project in Ghana, revealed that a fake concoction was able to be marketed across major television and radio stations in Ghana as a potent cure-all herbal medicine [3].
When it comes to where Ghanaians prefer to go for malaria treatment, this study revealed that most preferred to visit the hospital. The second most popular venue was the drugstore. Friends, self-medication with herbs and self-medication with painkillers were the next in that order. However, “hospital” and “drugstore” alone accounted for 93.6% of all the choices. This means an overwhelming majority of Ghanaians prefer to go to drugstores and hospitals when they suspect malaria. This is in line with the guidelines provided by the Ghana Health Services (GHS) which specify hospitals and pharmacies/licensed drug stores to be acceptable sources of antimalarial healthcare through testing and drug administration. Only a small majority of Ghanaians self-medicate.
The choice of a treatment venue however was significantly dependent on the gender of the person seeking healthcare. This study revealed females chose hospitals more than males who also chose drugstores more than females. Males preferring drugstores have also been reported by Quaresima, et al. [38] who noted that men in peri-urban areas buy medicine from drugstores or pharmacies when they suspect malaria. This difference in treatment choices may be due to various factors but may center on men’s reluctance to seek healthcare help [39]. This may be why the little autonomy provided by going to the drugstore and picking a choosing a drug is more favored by men. This finding also reveals the need for tailored malaria healthcare interventions and education to reach both men and women.
When it comes to anti-malarial drug preference, the drug chosen by most respondents was ACT. This was followed herbal preparations. The other options, chlogoquine, leaves or herbs, malafan, etc., accounted for less than 10% of the choice. It’s safe to say ACTs and commercial herbal medicines were the most chosen drugs. In contrast to the study by Yeboah, et al. [4] this study revealed that most Ghanaians preferred ACTs over herbal medicines.
The choice of antimalarial drug among these two options was also gender dependent. While both genders chose ACTs the most, females were more likely to choose ACTs more than males. Males were also more likely to choose herbal preparations (herbal medicines) than females. This is in striking contrast with other literature. Stjernberg, et al. [40] reported that Swedish females were more likely than males to use herbal medicine/supplements. In Saudi Arabia women were also found to have more knowledge on herbal medicine sources than men [41].
In both the preferred antimalarial and the effect of gender on choice, this study presents an alternate view on prevailing thoughts on anti-malarial preference and the effect of gender.
Even though analysis showed that Ghanaians preferred allopathic medicines for treating malaria more than herbal medicine, there were still positive and even negative opinions about both allopathic and herbal medicines/preparations. Both drug options were perceived by respondents to be efficacious by some and not efficacious by others.
There was agreement however in two themes: certification and dosage. While allopathic medicines were seen to be certified and approved, herbal antimalarials were never indicated by any respondent to be certified and approved. On the contrary, herbal antimalarials were seen to be uncertified. Also on dosage, while respondents indicated that the dosage of allopathic drugs was known, there was no such sentiment expressed for herbal antimalarials. There were however negative sentiments on herbal medicine dosages as respondents indicated that the dosages were unknown.
Opinions on herbal medicines however indicated areas of potential and risk. Potential exists in the prophylactic use of herbal antimalarials to prevent malaria. Risk also exists in the same vein. However, the area of greatest risk is the alternate or unprescribed use of herbal antimalarials indicated as “not safe for pregnant women” as emergency contraceptives.
There is also the need for public education as both drug options were perceived to have known and unknown side-effects. While some respondents were aware of side-effects associated with herbal medicines, others were unaware or insisted there were no side-effects. This, despite the numerous research findings that suggest otherwise [4,21,28,29]. There was also the opinion that allopathic drugs, like the ACTs have certain side-effects in respondents. This is an area that calls for education on the proper way to take some of these drugs and calls for more research that investigates some of these claims. There is also the need for education on the constituents and effectiveness of allopathic drugs as research has established their efficacy [3] and safety [42].
This study investigated antimalarial health-seeking behaviours in Ghana, with a specific focus on herbal medicine. Surveying adults across three major cities, we uncovered critical insights into public health practices.
The research highlights television and radio as primary sources of herbal medicine information, underscoring their pivotal role in health education. Furthermore, Ghanaians overwhelmingly prefer hospitals and drugstores for malaria treatment, aligning with Ghana Health Services' guidelines. Gender emerged as a significant factor, with females opting for hospitals and males for drugstores, emphasizing the need for tailored interventions.
Regarding drug preference, ACTs were favoured, in contrast to previous studies favoring herbal medicines. Gender played a role, with females more likely to choose ACTs than males.
Opinions on allopathic and herbal antimalarials varied but presented areas of potential and risk. Potential exists in that some herbal medicines are being used for malaria prophylaxis, but this also presents risk. Also risky is the tendency of some Ghanaians to use these herbal antimalarials as emergency contraceptives. The study emphasizes the necessity of public education on antimalarial treatments, including usage, side-effects, and constituents, as well as the need for continued research to address misconceptions.
In conclusion, our findings provide nuanced insights into Ghanaians' antimalarial health-seeking behaviours, guiding targeted interventions and educational initiatives for effective malaria control.
This research adds valuable insight into malaria health seeking habits of Ghanaians. The findings of this study will offer crucial input for healthcare policy and practice in Ghana. The findings, specifically the prominence of television and radio as sources of herbal information underscores the need for tailored health interventions via multimedia platforms. Additionally, the choices for treatment and the role of gender in these choices calls for customized healthcare strategies to improve accessibility. The preference for ACTs over herbal medicines also challenges assumptions and perceptions of antimalarial drug preferences in Ghana.
This research also reveals practices such the contraceptive use of possibly teratogenic herbal antimalarials and prophylactic use of herbal antimalarial that are a serious public health concern. Finally, concerns onthe certification and dosage herbal antimalarials and on the side-effects and constituents of allopathic medicines highlights the need for awareness and education efforts for herbal and allopathic antimalarials.
While informative, this study has some limitations. Its temporal context, conducted between 2013 and 2014, may not fully represent current healthcare-seeking behaviours. The study's focus on cities in Ghana reduces its generalizability to the entire Ghanaian population which includes rural areas and peri urban areas. Additionally, self-reported data may be subject to bias, particularly in sensitive areas like self-medication practices.
The study was approved by the University of Cape Cost Institutional Review Board (UCCIRB/28/12/3.1.4). Only individuals who agreed to participate in the study were allowed to participate.
Wilmot: Conception, design, and execution of the study; Data analysis and interpretation; Manuscript drafting; Asare: Ensuring adherence to journal guidelines and formatting; Yeboah: Literature review; Final proofreading of article.
This research was entirely funded using personal means, with no involvement of external financial support. Furthermore, the authors affirm that there are no conflicts of interest associated with this research project.