Introduction: COVID-19 disproportionally affects health care workers (HCWs). We assessed the protective practices toward COVID-19 among HCWs in Sierra Leone.
Methods: We interviewed 465 HCWs on their behavioral practices and captured their responses on the Likert Scale. Poor scores ranged from 8 to 29, and good scores from 30 to 40. We calculated proportional ratios (PR) and 95% confidence intervals (CI) to identify factors associated with good practices.
Results: All 465 (100%) HCWs responded. Fifty-nine percent (95% CI 54-64%) scored "good practice", 55% reported consistently washing their hands, and 57% wore masks most of the time. Of the 265 who wore a mask most of the time, only 74 (28%) wore the mask correctly, and 106 (40%) did not wear a mask during their interview. Working in Freetown (PR = 0.6; 95% CI, 0.4-0.7) and having a high perception that COVID-19 can be severe (PR = 0.6; 95% CI, 0.4-0.8) were associated with poor COVID-19 preventive practices. However, having a colleague who had COVID-19 (PR = 1.3; 95% CI, 1.1-1.5), and having a low perception that COVID-19 is a problem in a health facility (PR = 1.4; 95% CI, 1.1-1.6) were associated with good COVID-19 preventive practices.
Conclusion: The majority of the HCWs had good protective behavior practices towards COVID-19. We initiated continuing education and encouraged the enforcement of infection prevention and control procedures among HCWs with poor COVID-19 preventive practices.
COVID-19, Protective practice, Health care workers, Sierra Leone
Worldwide, Health care workers (HCWs) are at high-risk of contracting COVID-19 infection [1]. While HCWs represent 2% of the general population, they account for 14% of COVID-19 illnesses [2]. COVID-19 transmission in health facilities is an important route of COVID-19 transmission and ranged between 3% and 17% of overall COVID-19 infections [3,4]. Infection among healthcare workers can lead to staff shortages at health care facilities and negatively affect healthcare service delivery [5].
Even though the Government of Sierra Leone started implementing measures to prevent importation in early February 2020, the country recorded the first case of COVID-19 in a returning traveler on March 30, 2020. As of July 8, 2021, the Sierra Leone Ministry of Health and Sanitation reported 5,887 confirmed COVID-19 cases and 109 deaths. Of the total cases, 260 (4.4%) were health workers (COVID-19 Situation report as of May 22 nd , 2021).
Sierra Leone has inadequate human resources for healthcare. This exists across all health care levels with the greatest need in highly skilled doctors, nurses, midwives, and pharmacists in the primary level. The 2014-2016 Ebola outbreak added to this shortage [6]. The ratio of skilled health personnel per 10,000 population decreased from an already low level of 17.2 prior to the Ebola outbreak to 3.4 during this outbreak. This is far below the WHO recommended? ratio of 25 per 10,000 population [7].
This project will provide information necessary for planning infection prevention and control activities and baseline data to assist in measuring the future impact of IPC interventions in Sierra Leone and other similar settings. The objectives of this study are to describe personal protective behavioral practice among health care workers and to assess risk perceptions of health workers towards COVID-19.
This public health practice survey was conducted from 29 November to 15 December 2020 in 24 healthcare facilities: Four tertiary, eight secondary, and 12 primary healthcare facilities in Sierra Leone. The country has three levels in their health care system: Primary, secondary, and tertiary. The primary level is the first level of care, which is comprised of the peripheral health units including community health centers (CHC), community health posts (CHP), and maternal-child health posts (MCHP). District hospitals provide secondary care with bed capacity of 26 to 57. Regional/national hospitals provide tertiary care with bed capacity range of 100 to 300. I At the time of this survey, the country had 56 tertiary hospitals, 237 CHCs, 378 CHPs, and 606 MCHPs. The Western Area region is divided into the Western Area Rural and the Western Area Urban. The regions are subdivided into 14 districts which have at least one district hospital.
We used a cross-sectional design to describe and analyze the personal protective behavioral practices and risk perceptions of health care workers towards COVID-19 in Sierra Leone.
Our target population consisted of health workers who provided direct care for patients or health care facility staff who had direct contact with the patient’s body fluids or potentially contaminated items or environmental surfaces at the tertiary, secondary and primary levels in Sierra Leone. The health care professionals or health care facility staff included physicians, nurses, other allied health workers and auxiliary health workers such as cleaning and laundry personnel, X-ray technicians phlebotomists, respiratory therapists, nutritionists, social workers, physical therapists, laboratory personnel, admission/reception clerks, patient transporters and catering staff. The project was conducted in all four regions of the country.
Inclusion criteria: Any HCW involved directly or indirectly in the provision of care for patients.
Exclusion criteria : Any HCW involved directly or indirectly in the provision of care for patients but not able to provide answers due to illness or was not present at the time of the interview.
Selection of health facilities and health care workers: We purposely selected the nine of fifteen districts where there is an Intermediate Field Epidemiology Training Program (FETP) resident. We stratified by level of care (tertiary, secondary, primary). One referral teaching hospital at the national level and three referral hospitals of the four regions (tertiary level) were included in the project. At the district level, four district hospitals (secondary level) and four primary health units (primary level) were randomly selected from the list of district health care facilities in the selected regions (Figure 1). We created a sampling frame of all HCWs by profession (doctor, nurse, etc.) in each health facility and sampled proportional to population.
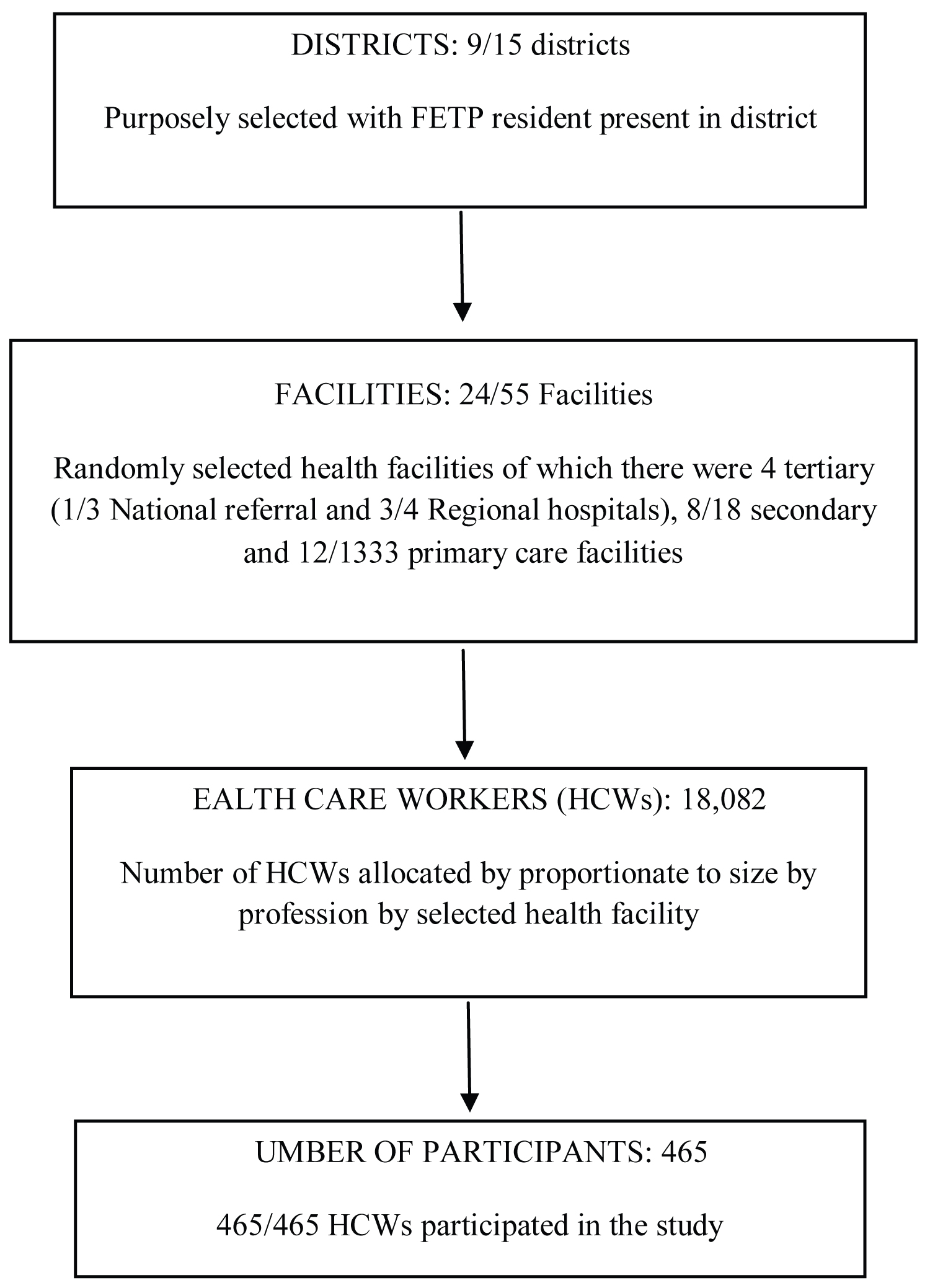 Figure 1: Flow chart of enrollment of health care facilities for study on protective behavioral practices against COVID-19 among health workers in Sierra Leone, 2020.
View Figure 1
Figure 1: Flow chart of enrollment of health care facilities for study on protective behavioral practices against COVID-19 among health workers in Sierra Leone, 2020.
View Figure 1
With 18,082 HCWs in the country, a sample size of 376 was calculated using EpiInfo with the following assumption parameters: 95% confidence level, 80% statistical power, 5% margin of error, and 50% HCWs with good practice of personal protective measures towards COVID-19. Ten percent of the calculated sample size was added for non-response rate, yielding a final sample size of 413. The sample size was distributed across the selected facilities proportional to the population and categories of health care workers.
The questionnaire was pre-tested to ascertain whether respondents understand the questions and to estimate the required time to collect data.
A questionnaire was developed to collect data on socio-demographic background (gender, age, level of education, work history, and job description), and preventive behavioral practices. Eight questions were asked for behavioral variables and eighteen questions for perceptions. Responses were recorded on a Likert scale of five (Strongly disagree, Disagree, Neutral, Agree and Strongly agree) for both behavioral and perception questions. Each question was given a possible score ranging from 1 (for Strongly disagree) to 5 (for Strongly agree). The behavioral practice score ranged from 8 to 40 with a score of 8 to 29 graded as “poor” and scores of 30 to 40 as “good” practice. and perception towards COVID-19 (eighteen questions). For perception, the score ranged from 18 to 90 with scores less than 75 classified as having “low” risk perception and scores of 75 to 90 classified as having “high” risk perception.
Data were captured and analyzed using EpiInfo version 7. Frequencies and proportions for the various variables were calculated and summarized in terms of person, place, and time. Results were displayed in frequency tables, charts, and graphs. Proportional ratios (PR) were calculated to test for statistically significant associations among different dependent and independent variables. Statistical significance was determined at a p -value of < 0.05.
Practice: is how respondents demonstrated their knowledge and attitude through their actions. In this project, we observed compliance to precautionary behaviors to prevent COVID-19 transmission such as wearing a face mask, hand washing and social distancing.
Risk perception: is how the respondents answered questions on the likelihood as well as the consequences of SARS-CoV-2 infection. The variable “COVID-19 Risk Perception” accessed different domains covering affective, cognitive, and temporal-spatial dimensions. The survey instrument included items capturing participants’ perceived seriousness of the COVID-19 pandemic, perceived likelihood of contracting the virus themselves over the next 6 months, perceived likelihood of their family and friends catching the virus, and their present level of worry about the virus.
Wearing mask properly: was the practice of wearing a mask covering month, nose, and chin during all routine activities throughout the entire shift. This was assessed by direct observation of HCWs by investigators.
Physical and social distancing measures: included physical distancing, reduction, or cancellation of mass gatherings, and avoiding crowded spaces in different settings. For physical distancing, we observed whether HCWs followed the World Health Organization recommends a minimum distance of at least one meter between people to reduce the risk of interpersonal transmission. This was assessed by direct observation of HCWs by investigators.
Ethical approval was obtained from the Sierra Leone Ethics and Scientific Review Committee. Permission was obtained from the administration of each health facility that we conducted the study. Written informed consent was obtained from each respondent before participating in the study, and information obtained was kept confidential.
Storage, analysis, and reporting of all data has been done in formats that do not reveal the identity of the respondents. This was done using identification codes instead of names in the analysis and reporting process. This project was determined as non-research under the “Field Epidemiology Training Program (FETP) Umbrella Protocol for Field-Based FETP Training Activities involving data collection by FETP residents”.
All 465 healthcare workers recruited for the study were interviewed. There were 344 (74%) females. The mean age of the workers was 35 ± 8 years and the age group 30-39 years accounted for 215 (46%). Three hundred and fifty-nine (77%) had a minimum of a diploma or certificate. There were 321 (69%) nurses and 131 (28%) other allied health workers in the medicine/emergency department. One hundred and eleven (24%) participants were from the Western Area Urban district and 200 (43%) respondents had a minimum of seven years working experience. One hundred and forty-three (31%) participants were involved in the care of COVID-19 cases (Table 1).
Table 1: Sociodemographic characteristics of health care workers in Sierra Leone, 2020. View Table 1
Two hundred and fifty-seven (55%) respondents received training on COVID-19 patient care and 352 (76%) received COVID-19 Infection Prevention and Control (IPC) related training. Most HCWs, 247 (70%), received their training within 3 to 6 months prior to being interviewed for this study. Of those 352 who received IPC training, the most common mode of training was practical, 322 (91%), as compared with online trainings, 31 (9%) (Table 2).
Table 2: Logistic regression of factors associated with COVID-19 preventive practice behaviors among health care workers in Sierra Leone, 2020. View Table 2
Thirty-six (8%) HCWs reported having been infected with SARS-CoV-2, 27 (6%) had a family member with COVID-19, 136 (29%) reported that a colleague that had been diagnosed with COVID-19, and 53 (12%) reported having a neighbor that had tested positive to SARS-CoV-2.
Overall, 275 (59%; 95% CI: 54-64%) of HCWs had good COVID-19 preventive practice. Specific good practices included avoiding large gatherings, public places and people who sneezed or cough outside the healthcare setting. Preventive practices we observed were hand washing, wearing masks and gloves, and social distancing (Figure 2).
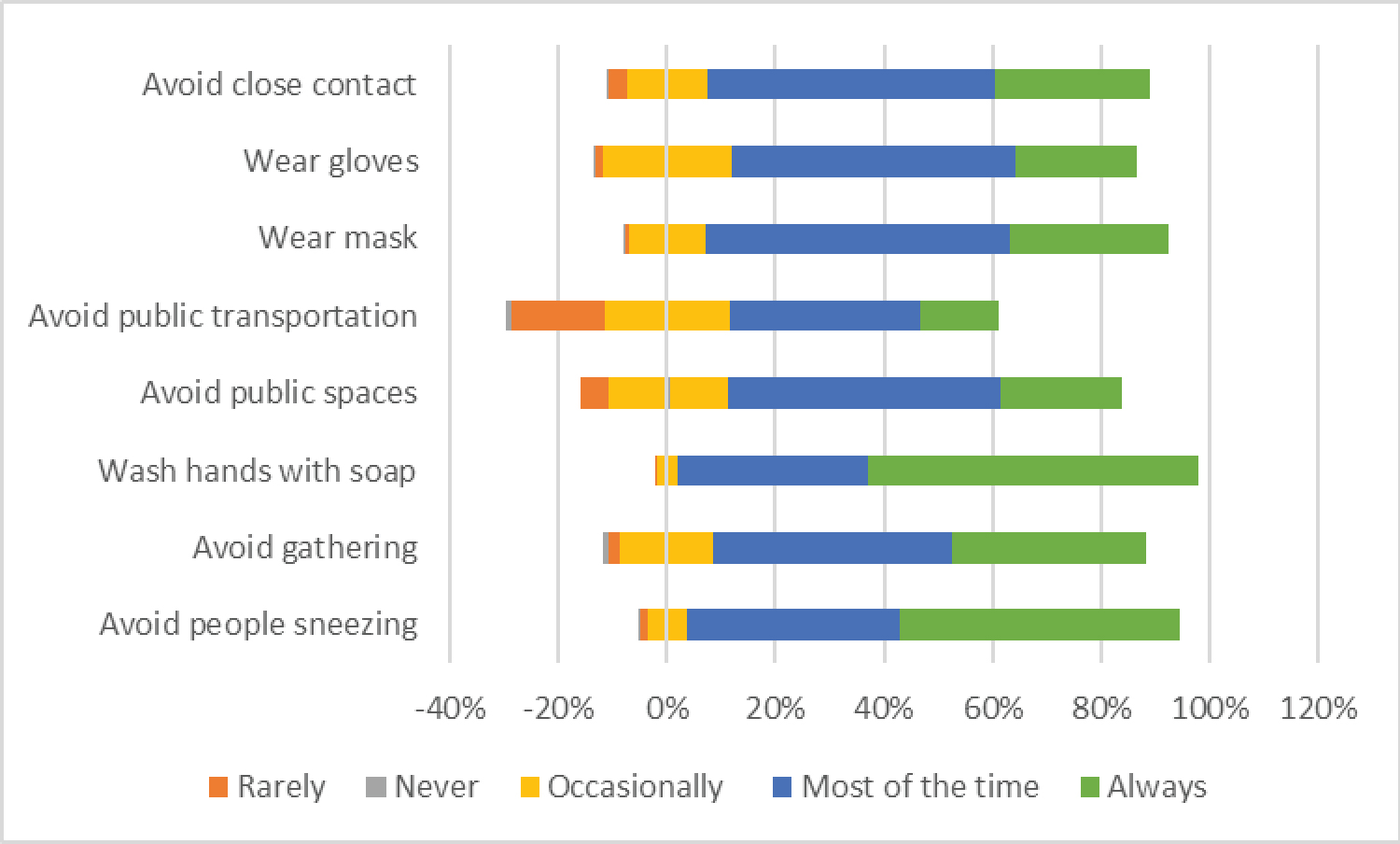 Figure 2: Preventive behavior of health care workers in Sierra Leone, 2020.
View Figure 2
Figure 2: Preventive behavior of health care workers in Sierra Leone, 2020.
View Figure 2
Overall, a total of 254 (55%) HCWs had a high-risk perception towards COVID-19. Most felt that COVID-19 is worldwide problem, and strongly agreed that it is a problem in Sierra Leone and in their health facility (Figure 3). The majority of HCWs strongly agreed that COVID-19 poses a problem to their health and family and to their neighbors and community at large. More than half of the respondents agreed that COVID-19 will affect many people, agreed that COVID-19 can be serious and that they are at risk of catching COVID-19. Also, 32% (150) of the HCWs were worried that they will likely catch COVD-19, while 80% (372) and 76% (354) strongly agreed that hand hygiene and wearing facemasks respectively can prevent COVID-19. In addition, majority agreed that social distancing (61%, 282) limits the spread of the virus and lockdown (40%, 184) and closing borders (47%, 214), airports (49%, 229), and schools (46%, 215) was an effective means of limiting the spread of the SARS-CoV-2.
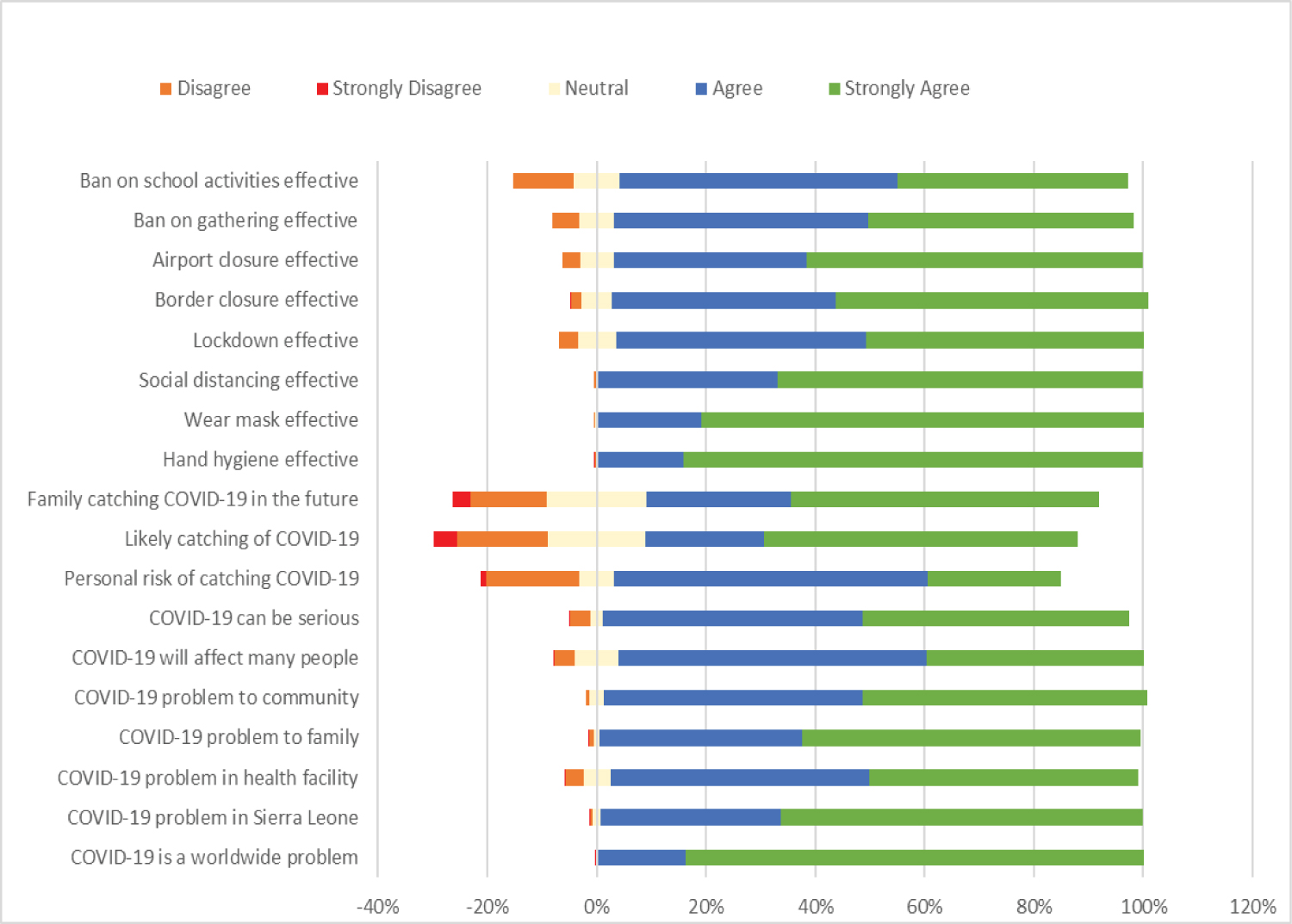 Figure 3: Risk perception of health care workers in Sierra Leone, 2020.
View Figure 3
Figure 3: Risk perception of health care workers in Sierra Leone, 2020.
View Figure 3
Bivariate logistic regression analysis: HCWs working in the capital city, Freetown, were less likely to engage in good COVID-19 preventive practice as compared to those working in other districts of the country (PR = 0.3, CI: 0.2-0.5) (Table 3). There was no association between age, sex, and educational level with engaging in good COVID-19 preventive practice. HCWs were more likely to engage in good COVID-19 practice when working in a high-risk department, worked for less 7 years, and had not received COVID-19 training. Caring for COVID-19 cases, receiving COVID-19 IPC specific training, the mode of training and the time elapsed since the training were not associated with preventive practice. HCWs who engaged in good COVID-19 practice were more likely to have a colleague with COVID-19 (Table 4). Having a family member or neighbor who had been infected with COVID-19 were not associated with engaging in preventive behaviors (Table 2).
Table 3: Multivariate logistic regression analysis for factors associated with good COVID-19 preventive practice among HCWs in Sierra Leone, 2020. View Table 3
Table 4: Association between belief in the effectiveness of selected control measures and practice COVID-19 preventive practice among HCWs in Sierra Leone, 2020. View Table 4
HCWs with good preventive practices did not perceive that COVID-19 was a problem in the community, could be a problem in their health facility, or will affect many people. Perception that COVID-19 could be a problem to self, family or friends was not associated with preventive behavior (Table 5).
Table 5: Association between practice of COVID-19 preventive behaviors among HCWs and risk perception in Sierra Leone, 2020. View Table 5
HCWs who had good preventive practice, they did not feel that the lockdown and a ban on school activities and gatherings was effective to stop the spread of COVID-19.
Multivariate logistic regression analysis for factors associated with good COVID-19 preventive practice: All variables that were found to be associated with good COVID-19 practice in bivariate logistic regression were put into multivariate logistic regression analysis (Table 3). HCWs with good preventive practice were associated with not working in Freetown, having a colleague who had COVID-19, and that COVID-19 is not a problem in their health facility.
This report identifies four important factors regarding protective behaviors of HCWs in Sierra Leone to prevent the spread of SARS-CoV-2. These factors were wearing masks, washing hands, social distancing, and avoiding public gatherings. Work location, knowing a colleague who had been infected with SARS-CoV-2, and perception that COVID-19 was a problem in their health facility was important for protective behaviors.
In our investigation, HCWs had good preventive practice for wearing masks, washing hands, social distancing, and avoiding public gatherings. The overall good practices (59%) found in our project is higher as compared to the finding in a study conducted among HCWs in Ethiopia (38.7%) [8]. and it is lower than what was reported among HCWs in China (89.7%) [9] and in Uganda (74%) [10]. These differences are probably due to the different phase of the pandemic that each study was conducted Our project was conducted in late November 2020 when the number of new cases in the country was on the decline while the studies in China and Uganda were conducted in the early stage of the COVID-19 pandemic in February and April 2020 respectively. The context and stage of the outbreak in each of these countries may also contributed to the compliance of COVID-19 preventive practices. Another factor to explain the differences might be access to availability of Personal Protective Equipment (PPE) and IPC trainings. Our results showed that 27.6% and 42.5% of 28% of the participants always avoided large gatherings and 43% avoided these gatherings most of the time. This is consistent with a study in Uganda where 43% avoided large gatherings most of the time.
This project reported that less than a half of the HCWs always complied with preventive practices such as avoiding people sneezing or coughing (44%) which is lower than the 60% reported in a study conducted in Uganda [10]. The difference may be due to study sites with the Uganda study in Uganda conducted in a teaching hospital and our study in clinics. HCW in Uganda were more likely to comply with preventive practices at work and home because they have a higher educational level, refresher trainings and the mortality and morbidity of COVID-19 was higher in Uganda than Sierra Leone.
In our project sex, age, and education level were not associated with good COVID-19 preventive practice. However, other studies reported an association between age over 40 years and females and education level and good practice [8,10]. Older HCWs may have more experience which enables them to follow good preventive practices. Also, HCWs with high education are more likely to compile with good preventive practices during their work. Moreover, females may be more likely to follow preventive practices [11].
In our project, work location was an important determinant of engagement in mitigation behaviors. HCWs working in districts outside of the capital city were more likely to engage in good protective behavioral practice than HCWs in the capital city. A decrease in cases in the capital city leads to relaxation of proactive behavior. Freetown was the epicenter of the COVID-19 pandemic and the decline in number of cases during this survey could have caused HCWs in Freetown to reduce their preventive practice behaviors.
This project reported that, knowing a colleague who had previously been infected was an important determinant in having protective behaviors. This may be the result of first-hand experience which dispels any myth one has about COVID-19 transmission and morbidity.
Regarding the association between risk perception and preventive practice, we found that HCWs who don’t perceive that COVID-19 is a problem in their health facility had higher odds of having good preventive practice. This can result from the belief that someone is not at risk might be influenced by good practice. Our findings are not consistent with study conducted in Ethiopia where HCWs who perceive risk and worry about the COVID-19 showed high [12]. Studies conducted during the early phase of a pandemic reported that perceived personal risk of infection and health effects influenced the engagement in protective practice [13]. A study conducted in G7 nations demonstrated that people who were concerned about the impact of COVID-19 on their health, the health of their family, friends, and their communities were almost three times higher to have good personal protective behaviors [14]. However, in our study, HCWs who don’t perceive that COVID-19 can be serious were less likely to have good preventive practices. This is similar to what was found in study conducted in G7 nations suggesting that those who are concerned by the impact of COVID-19 are more likely to have good precautionary behaviors [14].
Our project had limitations. To evaluate the preventive practice and risk perception, we relied on self-reported data which can be prone to recall bias and socially acceptable responses. Respondents may not know if colleague at workplace or friend or neighbor had COVID-19 because their status was not disclosed. There is selection bias as we purposefully recruited districts with FETP trainees and results are not generalizable to all HCWs in Sierra Leone. The object of this project was to describe protective behavior in HCWs and not to understand why HCWs could not engage in good COVID-19 preventive practice, which could have given more insight to the study. This project did not assess availability of IPC materials which can significantly influence preventive practices.
In conclusion, most HCWs had good preventive COVID-19 behavioral practice and high perception towards COVID-19. The recent Ebola, measles, and cholera outbreaks lead to many HCWs receiving training in IPC than other countries. Although a high proportion of HCWs perceived the effectiveness of personal protective behaviors towards COVID and reported to adhere to personal protective measures, most of them did not wear a mask correctly or were did not wear mask at the time of survey. We suspect this was due to complacency as there was decline in observed COVID-19 cases at the time of study and a shortage of face masks.
Factors strongly associated with good COVID-19 preventive practices were working outside Freetown, having a colleague who got COVID-19, perceive that COVID-19 could be serious, as well as low risk perception that COVID-19 is a problem in the health facility. These variables were probably influenced by workplace culture, training, access to and trust in PPE, increased risk influences behavior, awareness of risk influences behavior change, and belief that COVID-19 can be serious increases odds of preventive behavior, probably because of a firsthand experience.
The Sierra Leone Ministry of Health and Sanitation should develop a comprehensive strategy for improve behavior and adherence and accountability to follow IPC. Health facility authorities to implement strategies for compliance with recommended COVID-19 preventive practice at health facility level to limit nosocomial transmission and further spread of infection to the community. Intensify behavior change communication education among health care workers. Health care workers need to strictly comply with good COVID-19 preventive practice to minimize the risk of transmission among themselves, their family members, and the community. Further qualitative studies are required to find out the reason for non-compliance to IPC.