Coronavirus disease 2019 (COVID-19) is the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first discovered in Wuhan, China. The disease has caused over 80 million total cases recorded globally with deaths nearly reaching 2 million. In the Philippines, more than 400,000 cases were recorded at the start of the year 2021 [1,2].
The clinical presentation of COVID-19 disease ranges from a mild common cold-like illness to severe viral pneumonia leading to acute respiratory distress syndrome that is potentially fatal. Pneumonia in the setting of COVID-19 infection is classified as moderate, severe, and critical all of which require hospital admission [3].
Prognostic scoring systems were used to aid in identifying the disease severity in diseases with high incidence and risks of mortality. In patients with pneumonia, CURB-65 (Confusion, Urea, Respiratory rate, Blood pressure and Age) and PSI (Pneumonia Severity Index) are the ones proven and designed to optimize care and treatment outcomes [4].
The CRB-65 score is a rapid clinical prediction rule derived from CURB-65 to determine the severity of CAP and to help the physician in determining clinical plan of action. It ranks patients into strata of low (1.2%), intermediate (8.2%), or high (31.3%) risk of mortality based on the presence of the following features: Confusion; Respiratory rate ≥ 30/min; Blood pressure (SBP < 90 mm Hg or DBP ≤ 60 mmHg); and Age ≥ 65 years [5].
Modified Early Warning Score (MEWS) is a simple bedside tool that can even be used by nursing staff in the clinical are to identify patients who are at risk of deterioration and need more active management. It is based of five physiological parameters: systolic blood pressure, pulse rate, respiratory rate, temperature and AVPU score. A score ≥ 5 is statistically linked to increased likelihood of death or admission to an intensive care unit [6].
The quick Sepsis-related Organ Failure Assessment (qSOFA) is also a bedside clinical scoring system used to rapidly assess patients with a suspected infection that are at greater risk for a poor outcome. The following clinical criteria are observed: altered mental status; respiratory rate ≥ 22; and systolic blood pressure ≤ 100. A qSOFA Score of 2 or higher was associated with a 3- to 14-fold increase in the rate of in- hospital mortality [7].
This study aims to identify which easy-to-use scoring systems (CRB-65, MEWS, and qSOFA) has a better predictive accuracy in terms of clinical outcome of adult COVID-19 patients with severe and critical pneumonia.
Tondo Medical Center can adapt a predictive tool which can be beneficial for its patients in terms of appropriate treatment. The medical team can be more prepared with possible outcomes of the patient.
• To determine which tool has better predictive accuracy among CRB-65, MEWS and qSOFA in determining clinical outcomes in adult patients with severe and critical COVID-19 infection.
• To compare the predictive accuracies of CRB-65, MEWS, and qSOFA scoring systems in predicting mortality among adult patients with severe and critical COVID-19 infection.
• To compare the predictive accuracies of CRB-65, MEWS, and qSOFA scoring systems in predicting the need for mechanical ventilation among adult patients with severe and critical COVID-19 infection.
• To compare the predictive accuracy of CRB-65, MEWS and qSOFA scoring system in predicting the length of hospital stay among adult patients with severe and critical COVID-19 infection.
• There is no significant difference in the predicting clinical outcomes among patients with severe and critical COVID-19 infection using CRB-65, MEWS and qSOFA.
• There is significant difference in the predicting clinical outcomes among patient with severe and critical COVID-19 infection using CRB-65, MEWS and qSOFA.
The researcher has coordinated and sought the approval of the Chairman of the Department of Internal Medicine of Tondo Medical Center, as well as that of the Ethics Committee.
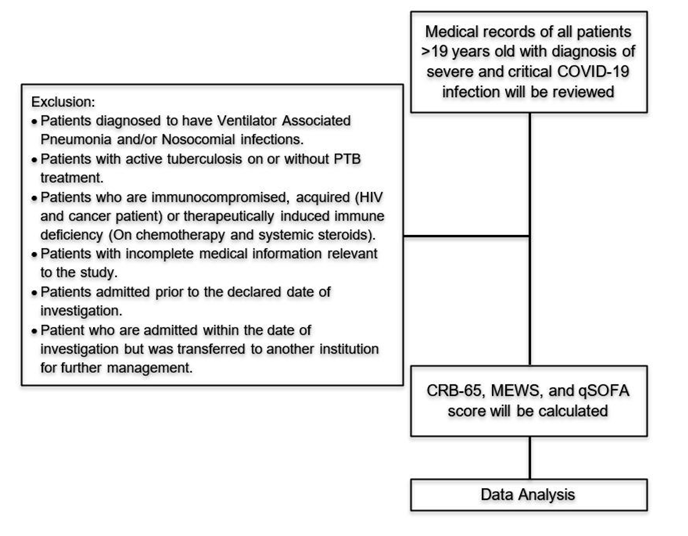
The researcher collected information from the Department of Internal Medicine of Tondo Medical Center as to the total number of patients to be included based on the primary study subject. Medical charts were reviewed upon approval of the Hospital Information Management Section Head. Information collected was relative to all cases of severe or critical COVID-19 patients with primary diagnosis of Community Acquired Pneumonia admitted at Tondo Medical Center from July 1, 2020 to December 31, 2020 [8,9].
Records review of the select patients was done to calculate the scoring systems – CRB-65, MEWS, and qSOFA; and to collect the data relevant to the study which includes: Age; presence or absence of confusion or altered mental status which can be seen on the admitting clinical history and physical examination’s general survey or neurologic exam; the admitting vital signs such as systolic and diastolic blood pressure, heart/pulse rate, respiratory rate, and temperature; the length of hospital stay; the mechanical ventilation status; and the treatment outcome classified whether the patient survived or died based on the disposition. Data gathered was encoded in MS Word and MS Excel.
Descriptive statistics was used to summarize the clinical characteristics and outcomes of the patients. Frequency and proportion was made for categorical variables and mean and SD for normally distributed continuous variables. Mann-Whitney U test and Fisher’s exact test was used to determine the difference of rank and frequency, respectively, between patients with and without a specific outcome. Odds ratio and corresponding 95% confidence intervals from binary logistic regression was computed to determine if the scores were a significant predictor of each clinical outcome. Area under the receiver operating characteristics curve as well as its diagnostic parameters was used to determine the diagnostic accuracy of CRB-65, MEWS and qSOFA score to discriminate a clinical outcome. All statistical tests were computed using two tailed test. Computation of the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR (+)) and negative likelihood ratio (LR (-)) was also done. Shapiro-Wilk was used to test the normality of the continuous variables. Missing values was neither replaced nor estimated. Null hypotheses were rejected at 0.05α-level of significance. STATA 13.1 was used for data analysis.
The necessary data was collected using chart review done at the medical records section of Tondo Medical Center. Information was encoded and managed in a password protected Microsoft excel spreadsheet. The charts and the encoded information can only be accessed by the primary investigator. No identifiable data will be encoded.
The study commenced upon the approval of TMC-IRB REC and was conducted in accordance with the ICH GCP and NEGHHRR 2017. All data gathered will be kept confidential and will be stored after 5 years, after which, will be permanently deleted. All information taken was used only for the purposes of this study. Since this is a records review, beneficence and nonmaleficence are not directly applicable. A waiver for informed consent was requested from the TMC-IRB since it is not feasible to obtained from each patient and there was no communication between the researcher and the patient. The study results, however, explore and recommend future management plan for patient with severe and critical COVID-19 infection.
A total of 158 patients who satisfied the set of criteria with complete required data were included in the analysis. Clinical characteristics and outcomes are presented in Table 1. There were 128 (81.01%) patients with CRB-65 score of zero to one and 30 (18.99%) patients who scored two points or more. 109 (68.99%) patients were noted to have zero to four MEWS score and 49 (31.01%) patients have 5 or more points. There were also a greater number of patients who scored zero to two than those who scored three to four in qSOFA which was tallied at 115 (72.78%) and 43 (27.22%) respectively. There were 40 patients (25.32%) who were intubated. Out of the total number of patients, 63 (39.87%) of them expired and 140 (88.61%) of the patients only stayed in the hospital for twenty-one days or less.
Table 1: Clinical characteristics and outcomes (n = 158). View Table 1
Table 2 shows the comparison of scores in terms of mortality. Higher scores in CRB-65, MEWS, and qSOFA are more associated to patient death than those who has lower score (P-value < 0.001). Figure 1 shows the area under the curve, sensitivity and 1 – specificity of the three scoring systems for the assessment of mortality. Based on AUC, the three scoring systems are of the same performance as predictor of mortality. All AUC values are significantly greater than 0.5 (Table 3).
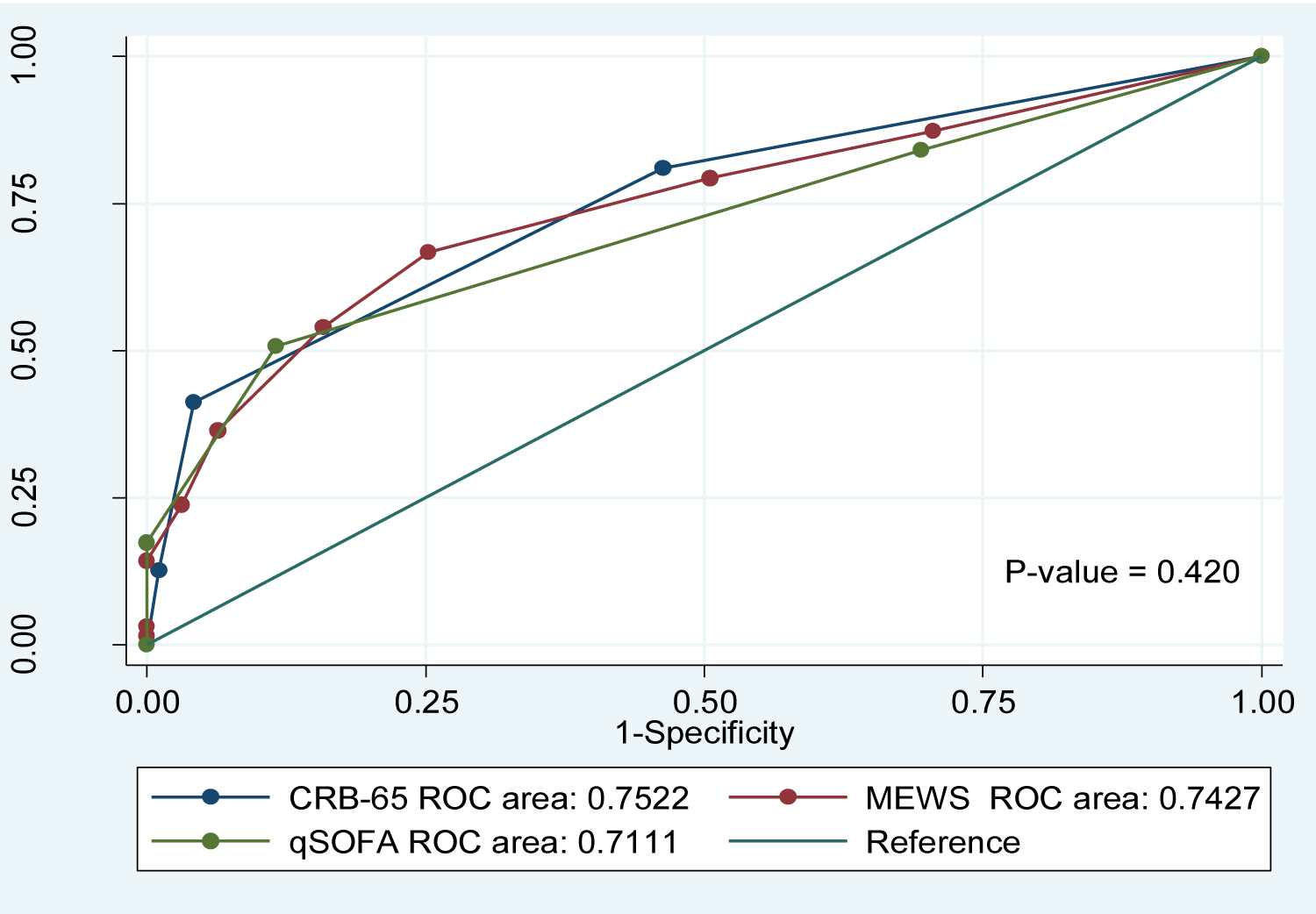 Figure 1: Comparison of AUCs to predict mortality.
View Figure 1
Figure 1: Comparison of AUCs to predict mortality.
View Figure 1
Table 2: Comparison of scores in terms of mortality. View Table 2
Table 3: Summary of ROC curve of CRB-65, MEWS and qSOFA scores in association with Mortality. View Table 3
Comparisons of scores in terms of need for mechanical ventilation were shown in Table 4. Collected data showed that lower scores in CRB-65, MEWS, and qSOFA will less likely be intubated during the hospital stay. Conversely, higher scores on all the three scoring systems were associated with increased need for mechanical ventilation (P-value < 0.05). Figure 2 shows the area under the curve, sensitivity and 1 – specificity of the three scoring systems for the assessment of mechanical ventilation requirement. Based on AUC, the three scoring systems are of the same performance as predictor of mechanical ventilation requirement. All AUC values are found to be significant and greater than 0.5 as seen on Table 5.
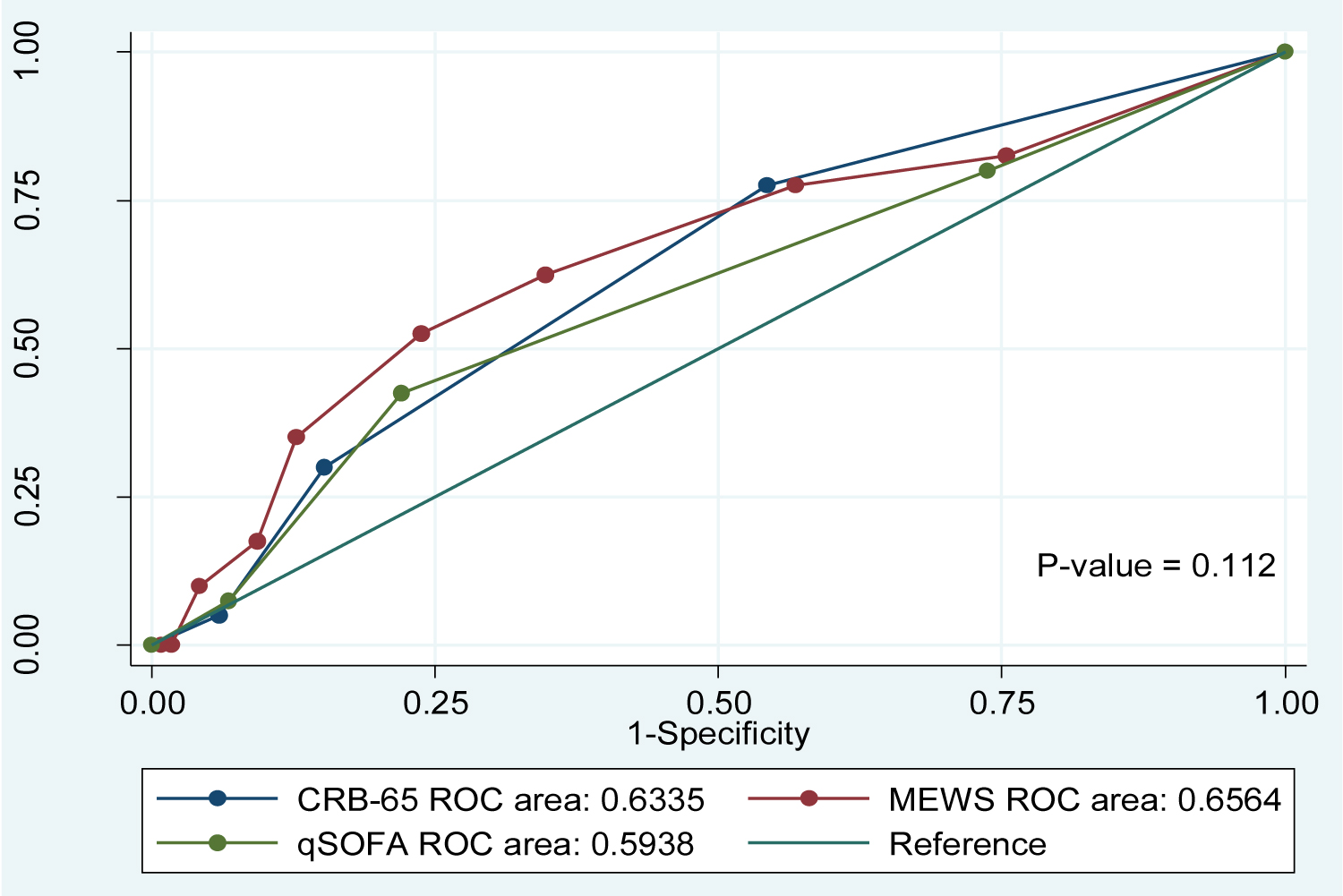 Figure 2: Comparison of AUCs to predict need for mechanical ventilation.
View Figure 2
Figure 2: Comparison of AUCs to predict need for mechanical ventilation.
View Figure 2
Table 4: Comparison of scores in terms of need for mechanical ventilation. View Table 4
Table 5: Summary of ROC curve of CRB-65, MEWS and qSOFA scores in association with need for mechanical ventilation. View Table 5
Table 6 shows the comparison of scores in terms of the length of hospital stay. Lower scores in CRB-65, MEWS and qSOFA were associated with twenty-one days or less hospital stay. However, data showed that even those with higher score on all three scoring systems were also associated with twenty- one days or less hospital stay. Hence, there is no significant difference between a higher versus a lower score on all three scoring systems in term of the length of hospital stay (Table 7 and Figure 3).
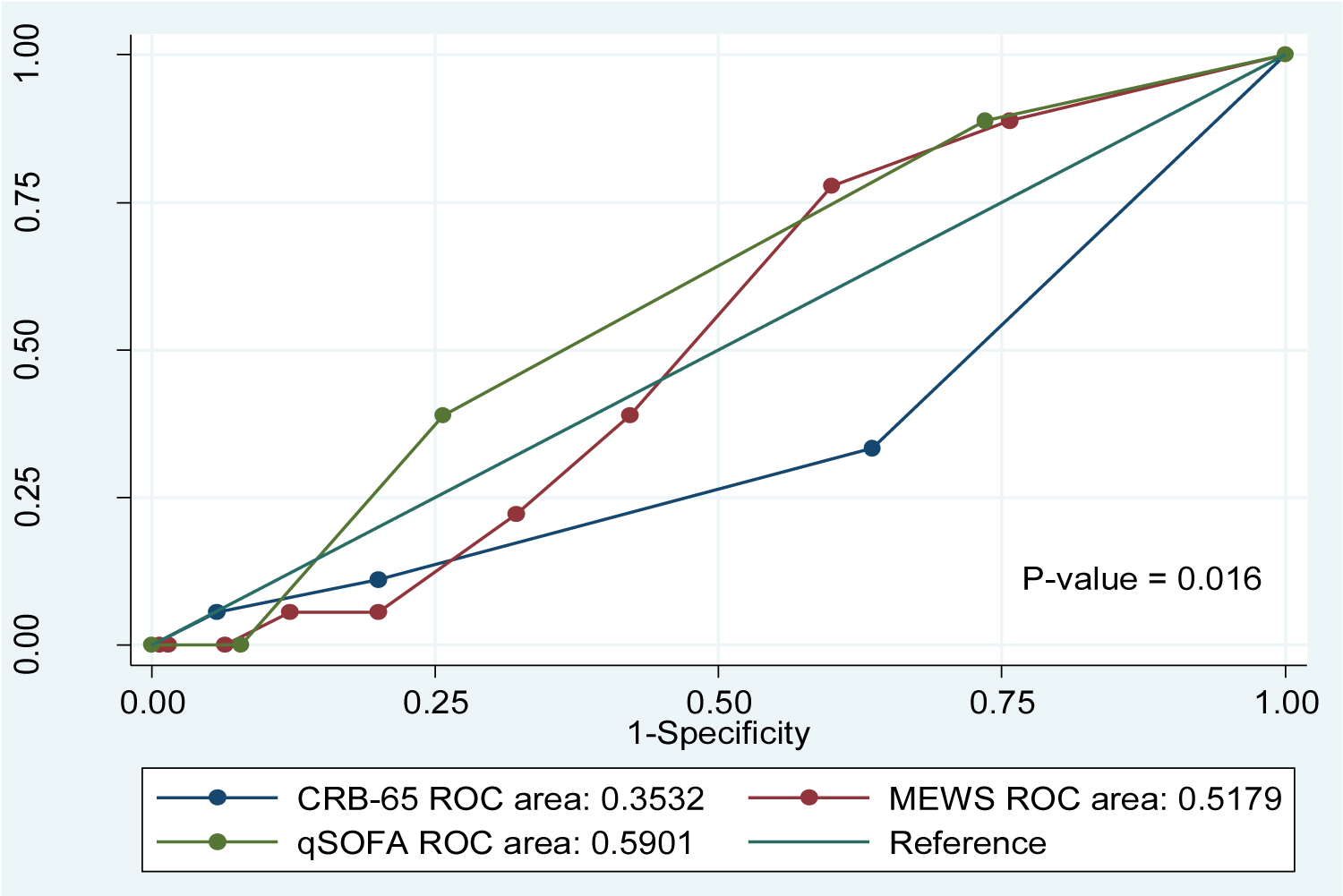 Figure 3: Comparison of AUCs to predict prolonged hospital stay.
View Figure 3
Figure 3: Comparison of AUCs to predict prolonged hospital stay.
View Figure 3
Table 6: Comparison of scores in terms of length of hospital stay. View Table 6
Table 7: Summary of ROC curve of CRB-65, MEWS and qSOFA scores in association with prolonged hospital stay. View Table 7
Summary of the association of scores to clinical outcome were listed on Table 8. Patients with a CRB-65 score of 2 or more were 15.9865 times more likely to expire compared to patients with a CRB-65 score of 0 to 1. Patients with a MEWS score of 5 or more were 6.2529 times more likely to expire compared to patients with a MEWS score of 0 to 4. Patients with a qSOFA score of 3 to 4 were 7.8827 times more likely to expire compared to patients with a qSOFA score of 0 to 2. Patients with a CRB-65 score of 2 or more were 2.381 times more likely to expire to need for mechanical ventilation compared to patients with a CRB-65 score of 0 to 1. Patients with a MEWS score of 5 or more were 3.5526 times more likely to need for mechanical ventilation compared to patients with a MEWS score of 0 to 4. Patients with a qSOFA score of 3 to 4 were 2.6154 times more likely to need for mechanical ventilation compared to patients with a qSOFA score of 0 to 2. There is no association seen between the scores in each scoring system in relation to the length of hospital stay.
Table 8: Association of scores to clinical outcomes. View Table 8
Given the limitations in the early days of the pandemic together with the consideration for the rational use of laboratory tests for proper allocation of hospital funds, it is imperative to use alternative tools and resources in the evaluation of COVID-19 patients. The three scoring systems that were chosen in the study can all be assessed without the need for diagnostic examination and can be easily done at the emergency department upon receiving the patient.
CRB-65, qSOFA, and MEWS were all found to be acceptable as a prognostic tool for determining mortality based on the result of AUC as shown in Figure 1. The predictive value of qSOFA was also studied by Liu, et al., where they found out that qSOFA is an acceptable tool to use for determining mortality risk [10]. Likewise, MEWS has also been shown to be efficient in predicting mortality consistent with the study done by Wang, et al. in 2020 which concluded that it is also as effective as the tools which use diagnostic tests such as PSI, CURB-65, and APACHE II [11]. Out of the three scoring systems, CRB-65 has the highest specificity (95.79%), while qSOFA has the highest sensitivity (88.42%) in predicting mortality in severe and critical COVID-19 infection.
Predicting the need for mechanical ventilation also provides information for both the patient and relatives when it comes to the severity of the disease, the cost of the management, and the possible clinical outcome of the patient. The results were able to identify that a higher score on all three scoring systems predicts the possibility of mechanical intubation in patients with severe and critical COVID-19 infection. A similar study using CRB-65 and qSOFA was also done to predict the need for intensive respiratory or vasopressor support (IRVS). The result of the said study showed that CRB-65 is superior to qSOFA in predicting the need for IRVS since it includes age as a variable which was identified as an independent prognostic factor in COVID-19 patients in another study [12,13]. The study did not find a significant difference in predicting the hospital stay in between the three scoring systems. However, we did not factor in this study the association of early mortality with a shorter hospital stay.
Higher scores in CRB-65, MEWS, and qSOFA are significantly associated with a higher risk of patient death. Likewise, higher scores on all three scoring systems are associated with an increased need for mechanical ventilation. The three scoring systems can be used independently in predicting mortality and mechanical intubation. Furthermore, none of the three scoring systems were identified to significantly predict the length of hospital stay of the admitted patients.
Further research and validation are recommended for the application of the three scoring systems to determine the effectiveness of these tools. Once proven to be useful in providing prognosis, these scoring systems can be used as part of the initial assessment and admission pathway for the evaluation of all adult COVID-19 admissions in the absence of laboratory results. A study can also be made specifically regarding the use of these scoring systems in predicting hospital stay considering the association between the severity of COVID-19 and the length of hospital stay.
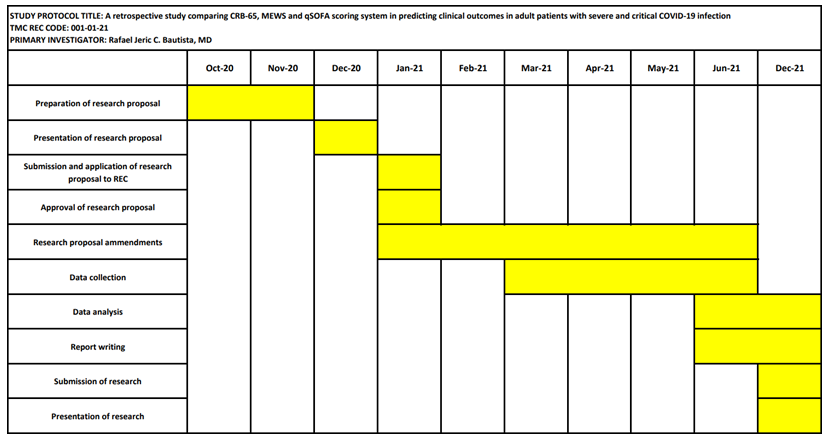
Gantt Chart