Little information exists on maternal deaths related to COVID-19 disease. We investigated maternal death due to COVID-19 infection and identify risk factors in Sierra Leone, 2021. We collected demographic and clinical data, reviewed medical records, and COVID-19 vaccination status. The decedent was nurse, 34-years-old, pregnant, 20 weeks gestation, and working at the district hospital. The pregnant woman died on June 26, 2021 with positive COVID-19 result. Deceased took one dose of COVID-19 vaccine. Delay to diagnosis COVID-19 infection caused death of the pregnant women. We recommended prioritizing COVID 19 testing for pregnant women particularly health care workers.
Maternal death, COVID-19, Pregnant women, Case report, Moyamba, Sierra Leone
COVID-19 was first documented in Wuhan, China at the end of 2019, and spread all over the world, infecting and killing millions of people [1]. Data from the World Health Organization (WHO) indicated that 80% of COVID-19 infections are mild or asymptomatic and the common symptoms include shortness of breath, fever, headache, sore throat, chest pain, diarrhoea, and anosmia [2]. No doubt, COVID-19 pandemic has an impact on perinatal health either through infection or indirectly through their consequences such as changes in health care, social and economic circumstances [3].
Pregnant women infected with COVID-19 may experience more severe outcomes compared with non-pregnant women. Pregnant women experience significant physiological and immunological changes that help the fetus to grow. These changes may increase the risk of getting diseases in pregnant women, particularly respiratory diseases. So, this implies that pregnant women and their fetuses are at high risk to get COVID-19 infection. Most pregnant women infected with COVID-19 are asymptomatic or present with mild symptoms [4].
Pregnant women infected with COVID-19 may experience more severe outcomes compared with non-pregnant women. Pregnant women experience significant physiological and immunological changes that help the fetus to grow. These changes may increase the risk of getting diseases in pregnant women, particularly respiratory diseases. So, this implies that pregnant women and their fetuses are at high risk to get COVID-19 infection. Most pregnant women infected with COVID-19 are asymptomatic or present with mild symptoms [4].
In Sierra Leone, the first case of COVID-19 case was reported on the March 31, 2020 in the capital Free town [9]. As of July 2022, Sierra Leone has reported 7722 COVID-19 cases, of them, 125 (1.6%) cases died as a consequence of the infection [10]. There was no published information on the impact of COVID-19 on pregnant women in Sierra Leone. Given the consequences' severity of COVID-19 infection, this may impose a greater risk in pregnant women compared to other non-pregnant women. On June 27, 2021, the Moyamba District Surveillance Unit was alerted of a maternal death at one hospital in the district. This investigation was conducted to verify and confirm the maternal death, and identify causes and factors associated with maternal death in Moyamba District, Sierra Leone.
This is a case report study conducted to investigate and describe COVID-19 related maternal death at a hospital in Moyamba District in June 2021. Moyamba District is one of the four districts in the southern region with a total projected population of 434,153 in 2021., Of the total population, 96,382 (22.2%) were women of childbearing age, among them 19,103 (4.4%) were pregnant women (2015 National population census). There are 106 Functional Peripheral Health Units (PHUs) and 3 hospitals in the district Antenatal care (ANC) services are conducted at all 109 health facilities. For the year 2021, 15,494 pregnant women attended first visit of ANC and 14,656 attended forth visit of ANC with a dropout rate of 5.4%. Out of a total of 11,284 deliveries conducted in the district in 2021, 1650 (14.6%) were conducted by doctors, midwives or surgical CHO and 9,634 (85.4%) conducted by the other cadres. There are five medical doctors in the district but no obstetrician/gynecologists. The surface area is both land and riverine with hard-to-reach areas making accessibility very difficult. The district has 14 chiefdoms in 143 sections and 1617 towns or villages.
We maternal death and COVID-19 definitions to verify and confirm maternal death at a hospital in Moyamba District. We collected demographic and clinical data about the death. This data included age, occupation, education level, gravida, date of symptoms onset, date of seeking medical care, date of notification and investigation and the result of the blood, urine and swab tests. We interviewed health care workers, community and family members, and community health workers to collect more information related to the case-patient death. We also reviewed records, reports and registers, including patient charts and other records at the hospital to assess and outline the causes of the death. We also assessed the possibility of delays; delays in making decision to seek delivery service, delays in reaching to facility or delays in accessing delivery service and care after arrived at health facility associated with the case-patient death.
Blood and urine samples were collected from the pregnant woman for laboratory analysis when she arrived at the hospital. Hemoglobin and White blood cell count in addition to urinalysis were done. Also, a nasopharyngeal swab was collected to test COVID-19 infection using Polymerase chain reaction (PCR) test at Kenema Regional Hospital Laboratory.
We investigated and line listed five primary contacts to the deceased including three health care workers (nurses) hospital, and two family members (husband and son).
We assessed the decedent pregnant women COVID-19 vaccination status by reviewing vaccination registries at Static 2 Community Health Centre (CHC) in Moyamba Government Hospital.
We interviewed staff and reviewed records, registers and reports at all health facilities within Moyamba Township to ascertain if the patients received any Antenatal care services.
The case-patient was a pregnant woman (20 weeks gestation), 34-years-old (gravida 2, para 1 alive), with tertiary education and a nurse working in a hospital in Moyamba District. On June 19, 2021, the case-patient started feeling the clinical symptoms and sought medical care in the maternity ward. On June 22, 2022, the pregnant women presented herself to the maternity ward with respiratory symptoms signs. She was complaining of difficulty in breathing, side pain and coughing. Laboratory investigation for Malaria was negative, hemoglobin was slightly low (HB = 11.5 gram per deciliter) (normal range for women 11.6-15 grams per deciliter) and White Blood Cells (WBC) was high, WBC = 14000 gram per microlitre (normal range of WBC = 4000-10000 grams per microliter. The urine analysis revealed that specific gravity was 10.0, PH was 6.0, protein, glucose and ketone were nil, Urobilinogen was normal, Leucocytes was (+), Bilirubin was nil, and epithelia was 9-10 g/deciliter. The initial diagnosis of the case-patient was Upper Respiratory Tract Infection (URTI) and was treated with Amoxicillin (250 mg 3 times a day for 5 days), in addition to tabs Paracetamol.
On June 24, 2021, case-patient was admitted for severe pneumonia and was treated with erythromycin tabs 500 mg, 3 times a day for 5 days, tabs Paracetamol 1g 3 times a day, tabs Fefol 2 daily and Inj. Diclofenac 75 mg stat. Her symptom persists while on the above treatment in the ward for 3 days. On June 25, 2021, an injection of Ceftriaxone 1g two times a day was added to the above treatment. On June 26, 2021, her condition became worse with dyspnea and coughing. Her condition was reviewed, and then she was suspected for COVID-19 infection. The surveillance unit was also notified. Dextrose 50% was given and oxygen was fixed. On June 26, 2021, the case-patient started gasping with secretions from the mouth, Cardiopulmonary Resuscitation (CPR) was done but the patient died on the same day (Figure 1). From the information gathered from all stakeholders, there was no evidence of self-medication by the deceased.
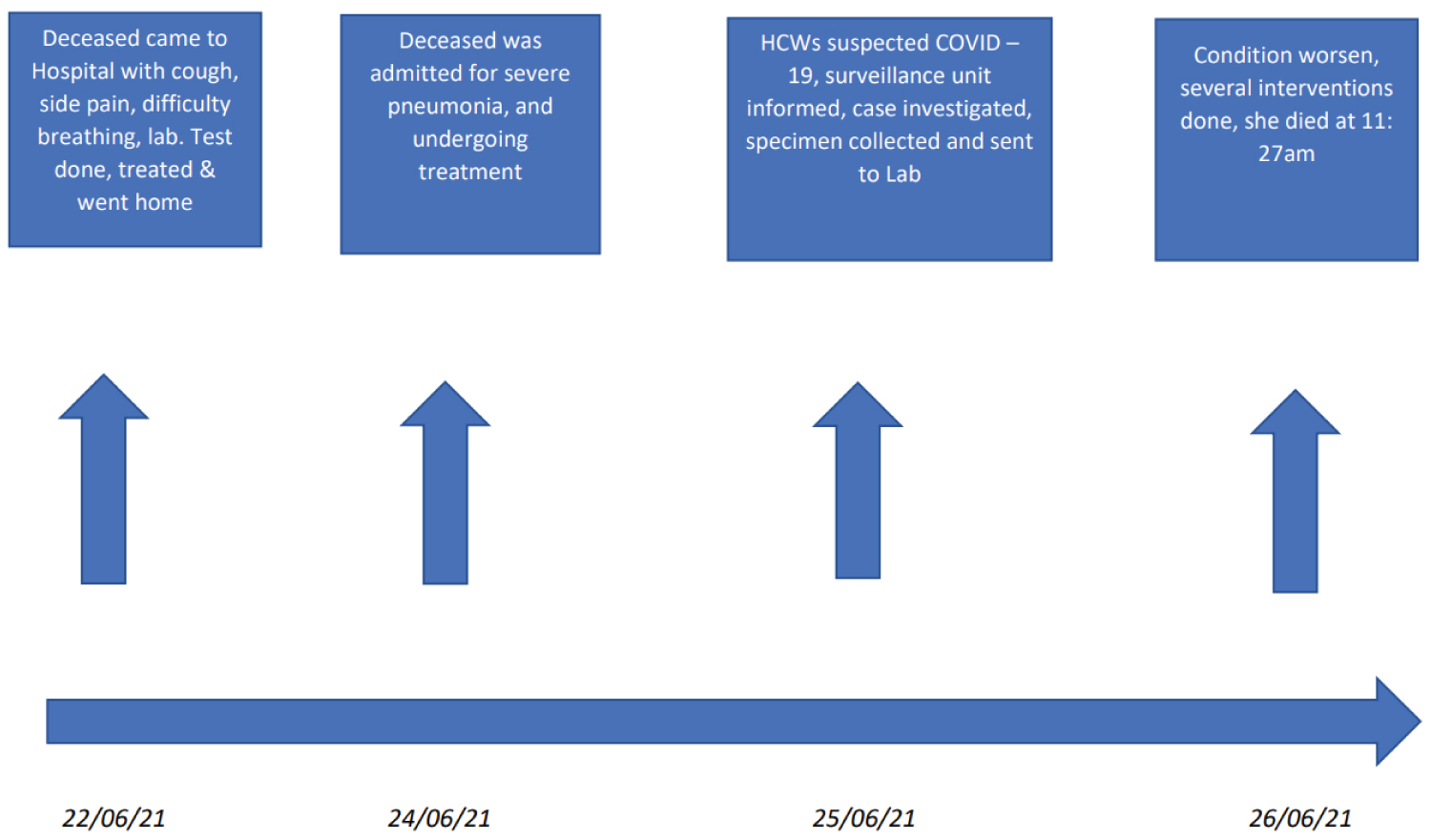 Figure 1: Timeline of the event.
View Figure 1
Figure 1: Timeline of the event.
View Figure 1
There was no clear evidence to show that the decedent had direct contact with a confirmed COVID-19 case but it is likely that she might have been exposed to a COVID-19 confirmed case while working in the female ward where COVID-19 cases have previously been identified and confirmed. The case-patient was investigated by the surveillance team and the specimen was collected and sent to the reference laboratory in Kenema and result came positive for COVID-19 by using PCR test.
Three nurse and two family members (husband and child) were identified as primary contacts and were quarantined for 14 days. We monitored them daily for 14 days. None of them was positive at the end of the quarantine period. No suspected cases were identified after the monitoring period. We found out that the deceased case-patient had never registered for ANC at any of the health facilities in Moyamba town and therefore had no ANC record. We found out that the deceased received her first COVID-19 vaccines on March 24, 2021 at Static 2 CHC. The vaccine type was Sinopharm (Batch number 2021010035). No evidence that case-patient received her Tetanus-Diphtheria (TD) vaccine during the pregnancy period.
Coronavirus disease 19 (COVID-19) has recently emerged as a major threat to human health. Infections range from asymptomatic to severe or critical with multi-organ failure or dysfunction or respiratory failure which requires urgent mechanical ventilation or high-flow nasal cannula [11]. This study shows the death of a pregnant woman was due to a COVID-19 infection during active service in a hospital in Sierra Leone. Pregnant women are more likely to get very sick when they are infected with COVID-19 compared with non-pregnant people. COVID-19 infection can affect women in pregnancy and increase the risk of complications. Current evidence suggests that pregnant women are at increased risk of serious illness, specifically hospitalization, ICU admission, and the need for mechanical ventilation and if this is accompanied by infection with an emerging pathogen may be further complicated by the pregnancy [12].
The case patient reported in this study was in the second trimester of pregnancy (week 20) which might increase her risk. A study suggested that pregnant women in the second and third trimesters infected with SARS-CoV-2 had a higher rate of maternal mortality, intubation and intensive care unit (ICU) compared with non-pregnant women [13]. The poor outcome of pregnancy is due to the fact that COVID-19 infection causes immunity changes which cause immune-suppressive status during pregnancy and diminished cell-mediated immunity has been also documented. This situation decreases the pregnant woman immunity which provides an appropriate condition for the coronavirus to replicate [14]. In Latin American countries, It was observed that morbidity and mortality due to COVID-19 infection were high where two out of three deaths occurred in pregnant women in the second and third trimesters [15].
In this investigation, there was a delay in identifying a COVID-19 infection on the pregnant women which might have led to severe complications and final death. COVID-19 infection in pregnant women required rigorous care due to the severity of infection in this group. Pregnant women infected with SARS-CoV-2 badly need for respiratory support [16]. The delay in the administration of artificial ventilation may lead to multi-organ or respiratory failure which may be complicated by pregnancy. Although there is a 20% Oxygen demand during pregnancy, COVID-19 infection causes a 25% decrease in both expiratory volume and residual volume, causing a total decrease in lung capacity [17]. A systematic review of studies on the impact of COVID-19 on pregnancy reported that COVID-19 infection is associated with an increased risk of adverse pregnancy outcomes. It was observed that hospital people who are infected with SARS-CoV-2 show a hyper coagulate state which increases the risk of venous thromboembolism, particularly during pregnancy [18].
COVID-19 pandemic affects the routine essential healthcare services, particularly antenatal care services for pregnant women. A study conducted in India indicated that the COVID-19 pandemic decreased 22% points in antenatal care coverage. This decrease occurred because health care workers fear of getting COVID-19 infection during the pandemic [19].
Despite that, no evidence was provided that the patient got an infection at the workplace, working with COVID-19 patients put health care workers at high risk to get an infection. Healthcare workers have a high risk to get COVID-19 infection [20]. So, following infection prevention and control (IPC) measures including provisions of materials, monitoring of healthcare workers' compliance (at triage and wards) and monitoring of patients and visitors flow are crucial when dealing with infectious diseases, particularly COVID-19. Limitation related to this case was that the case died before getting more information from her. Based on our investigation a pregnant woman died due to COVID-19 infection. Delay in accessing health care services might complicated the deceased condition. No evidence of the source of infection with a possibility of nosocomial infection. We recommended prioritizing pregnant women to test for COVID-19 infection specially those who have contact with COVID-19 patients particularly those who are working as health care workers.
We reviewed the standard case definition of all immediately reportable diseases especially COVID-19 with the entire staff at the hospital to search for additional cases. Staff working at female and maternity wards were advised to apply Infection prevention and control (IPC) measures such as wearing face mask, proper use of hand glove and regular hand washing with soap and clean water. Also, disinfection of bed and linens used by the deceased was done. Primary contacts were line-listed, quarantined and monitored for 14 days.
Authors declare no conflict of interest.
Conception and design of study: Brima A. Gamanga, Adel Hussein Elduma, Gebrekrstos Negash Gebru, Jean Leonard Hakizimana; Acquisition of data: Brima A. Gamanga, Gbessay Saffa; Analysis and interpretation of data: Brima A. Gamanga, Gbessay Saffa, Adel Hussein Elduma, Amara Alhaji Sheriff; Drafting the manuscript: Brima A. Gamanga, Adel Hussein Elduma, Amara Alhaji Sheriff; Revising the manuscript critically for important intellectual content: Adel Hussein Elduma, Gebrekrstos Negash Gebru, Jean Leonard Hakizimana, Amara Alhaji Sheriff, Kassim Kamara; Approval of the version of the manuscript to be published: Brima A. Gamanga, Amara Alhaji Sheriff, Adel Hussein Elduma, Gebrekrstos Negash Gebru. All authors have read and agreed to the final manuscript.
I would like to thank the African Field Epidemiology Network/Sierra Leone Field Epidemiology Training Program staffs and mentors for their continuous support. My thanks also extended to the Medical Superintendent and the entire staff of Moyamba Government Hospital District Medical Office and all staff of the Moyamba DHMT, and the National Ministry of Health and Sanitation. Further, I thank my colleagues and family members for their support during my residency.