Cholera is a diarrheal infectious disease that continues to cause morbidity and mortality in Zimbabwe. This study reviews the morbidity and mortality data of cholera in Zimbabwe during the 2008/2009 and 2018/2019 outbreaks, critically discussing the factors responsible for the outbreaks and then suggests recommendations for public health actions. The data used for this study was obtained from the National Health Information and Surveillance Unit under the Ministry of Health and Child Care, Zimbabwe, and other published literature. The 2008/2009 cholera outbreak represents the largest outbreak with a total of 98592 cases and 4288 deaths, Case Fatality Rate (CRF) 4.3%. The most recent outbreak occurred from September 2018 to March2019 where a total of 10730 cases and 69 deaths were recorded, (CRF 0.64%). The deterioration of the water and sewerage infrastructure in the country due to historically low or poor investment in this area together with the declining health infrastructure, and reduced health care staff are the main drivers of outbreaks. Improving these areas is critical for cholera elimination in the country.
Cholera, Mortality, Risk factor, Challenges, Public health, WASH
MoHCC: Ministry of Health and Child Care; UN: United Nations; NEOC: National Emergency Operation Centre; UNICEF: United Nations Children’s Fund; WASH: Water Sanitation and Hygiene; SDG: Sustainable Development Goals; WHO: World Health Organization; GTFCC: Global Task Force on Cholera Control; ECHO: European Civil Protection and Humanitarian Aid Operations; NCTF: National Cholera Task Force
Cholera is an acute, diarrheal illness caused by infection of the intestine with the toxigenic bacterium Vibrio cholerae serogroup O1 or O139 [1]. Approximately10% of the infected persons will have severe disease characterized by profuse watery diarrhoea, vomiting, and leg cramps [1]. Without treatment, death can occur within hours. The disease remains a major public health problem and mainly affects developing world populations where access to adequate water and sanitation resources and health care is a challenge [2]. Cholera is simple and inexpensive to treat when knowledgeable, committed health workers are available and provide with adequate medical resources [3]. Unfortunately, mortality rates remain way too high in several areas of the developing countries including Zimbabwe that recorded 4.3% case fatality rate during the 2008-2009cholera outbreak [4].
The disease continues to affect more than 47 countries worldwide, predominantly developing countries where access to clean and safe water and sanitation remain a serious challenge. Worldwide, an estimated 4 million cholera cases and over 140,000 deaths are reported annually [2]. Approximately 1.3 billion people are at risk of cholera in endemic countries [5]. Sub‐Saharan Africa bears the brunt of global cholera burden. The region is broadly affected by many cholera outbreaks that can spread across countries [2,6]. In 2017, over 150,000 cholera cases and 3000 deaths (CFR of 2.3%), were reported from 17 countries in Africa [7]. Cholera outbreaks have been reported across Africa and the ecological zones have broadly been defined on the basis of case reporting.
Persistent cholera outbreaks in Zimbabwe reflect the lack of access to basic sanitation, clean water and health care [8]. Due to the increasing recognition of the threat cholera epidemics pose to the global security, beyond its impact on human health, cholera has been identified as one of the diseases for control and elimination [9]. According to Hotez, et al. [10], (2020), cholera has been recognized by PLoS Neglected Tropical Diseases because of its global public health impact and its high prevalence in impoverished countries. Low-income countries, where the burden of infectious diseases is also generally high and the health systems are ill equipped to even respond to the basic health needs of the population, face greater vulnerabilities to the consequences of epidemics, setting back hard-earned health and socio‐economic gains.
In line with the United Nations (UN) Sustainable Development Goal (SDG) 6, the government of Zimbabwe through the Ministry of Health and Child Care (MoHCC) has prioritized improving quality of life for all its citizens. In July 2019, the National Cholera Task Force (NCTF) declared the elimination of cholera in the country by 2028 and endorsed the development of an inclusive Roadmap, guided by the Global Task Force on Cholera Control (GTFCC). The aim of this review is to describe the morbidity and mortality data of the 2008/2009 and 2018/2019 cholera outbreaks in Zimbabwe as well as critically discuss the factors responsible for the outbreaks and provide recommendations for public health actions.
The review of the literature was conducted using PubMed and Hinari. The data was obtained from the National Health Information and Surveillance unit under the Ministry of Health and Child Care. Interpretation of the results was done according to local contexts using published literature and national reports (Figure 1).
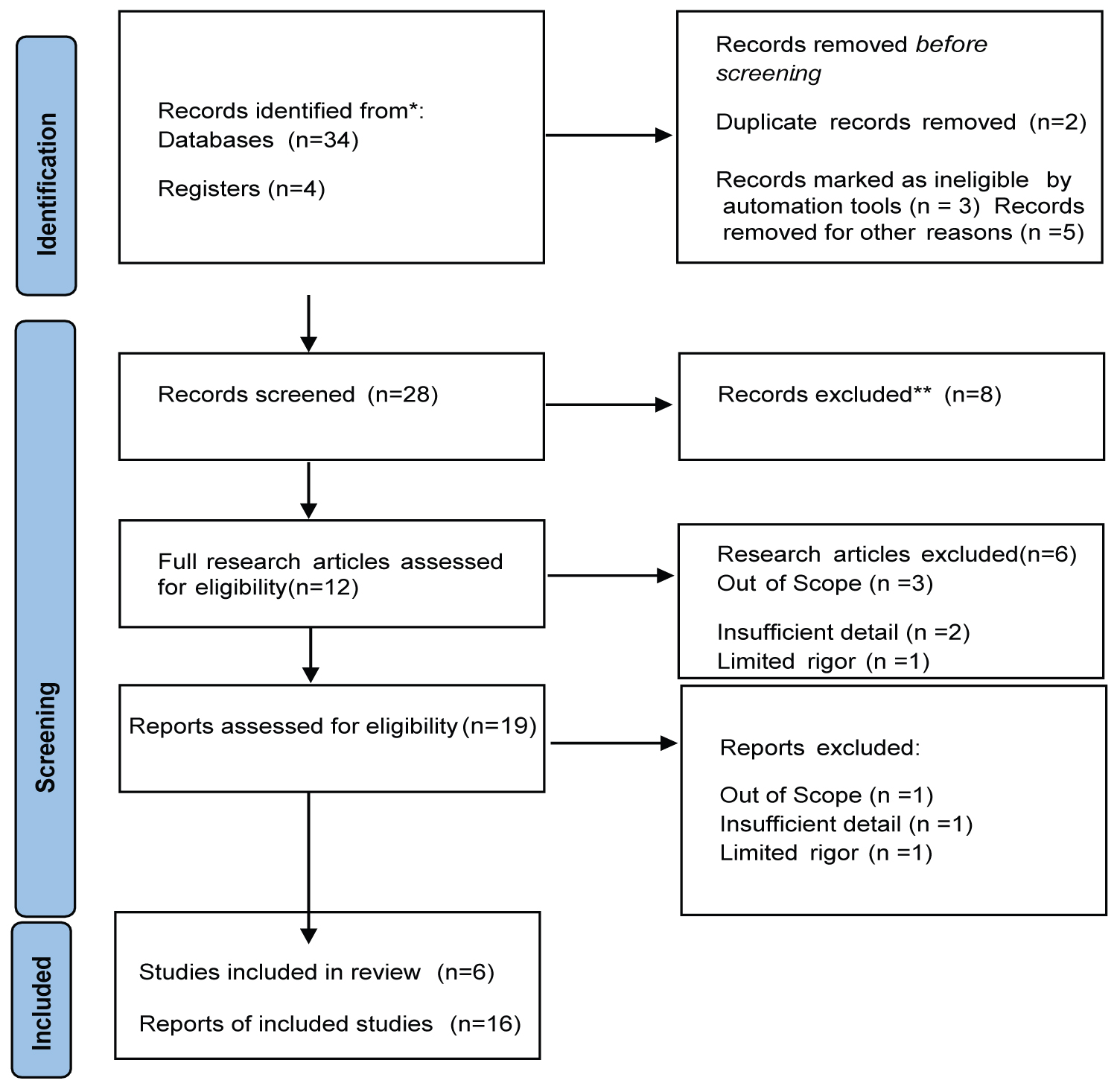 Figure 1: Number of cholera cases, mortality, and risk factors: Study Selection Review.
View Figure 1
Figure 1: Number of cholera cases, mortality, and risk factors: Study Selection Review.
View Figure 1
The 2008 to 2009 outbreak is the most devastating outbreak recorded in Zimbabwe. The outbreak quickly escalated owing to the dilapidating economic structure of the nation. The outbreak, which started in August 2008 in a district (Chitungwiza) located close to Harare, the country’s capital city, rapidly extended to several surrounding districts before spilling into other various provinces including Mashonaland East, West, Central provinces, the Midlands province, Masvingo Province and the Manical and province [4]. A total of 98592 cases and 4288 deaths had been recorded by the end of April 2009 during which time the epidemic had affected over 95% of the country’s districts [11]. The case fatality rate was 4.3%.
Epidemiological studies implicated a small epidemic that occurred in districts near Harare from January to April 2008 as a precursor for the larger epidemic that emerged in August, while blaming inadequate health care services for the failure to detect and extinguish further transmission of the bacteria. Further worsening the situation was the great economic collapse within Zimbabwe which saw forced closure of several of the country’s hospitals as they could not afford to buy essential medicine and pay healthcare practitioners. By early December people had to rely on unclean water as stocks of government-provided water-purification chemicals had run out whereas the sanitary conditions declined in many affected areas, mostly in Harare urban, where the dilapidated sewage systems caused environmental contamination by raw sewage, particularly streets and rivers.
On the 4th day of December, 2008, the Zimbabwe an government declared a national state of emergency and appealed for international aid. Organizations such as the World Health Organization and the International Committee of the Red Cross intervened to improve disease surveillance, to deliver medical supplies, and to provide essential health care personnel. These organizations also ensured that communities received clean and safe water. Despite the efforts of relief organizations, by late December 2008, the disease had spread to almost all of the 10 provinces of Zimbabwe. The struggles to prevent new infection cases and further deaths due to cholera were impaired by acute food scarcities and the closure of numerous hospitals and clinics, these factors furthered a remarkable rise in the cholera mortality rate in Zimbabwe, which reached 5.7%, significantly exceeding the 1% death rate classically associated with large-scale cholera epidemics [11]. Mortality rates inflated to 50% in Budiriro a high-density suburb of the capital city, Harare [12]. The estimated basic reproductive numbers were highly heterogeneous, ranging from a low value of just above unity to 2.72 [13]. Partial reproductive numbers were also highly heterogeneous, suggesting that the transmission routes varied by province and human-to-human transmission accounted for 41-95% of all transmissions [13].
In addition to the spread of cholera within Zimbabwe, the outbreak took on a sub regional dimension with cases being reported from neighbouring countries. In South Africa as of 4 March 2009, 12115 cumulative cases and 59 deaths (CFR of 0.5%) have been recorded, with the bulk of the cases in the provinces of Limpopo (5165) and Mpumalanga (6644) [14]. In Malawi, as of 8 February, 2635 cases including 67 deaths (2.5%) were reported in 18 districts [14]. Of these 1478 cases and 44 deaths have been reported in Lilongwe [14]. Cases have also been reported in Botswana (Palm Tree), Mozambique and Zambia [14]. The spread of the diseases across the countries raises the need for international coordination during times of pandemics (Figure 2).
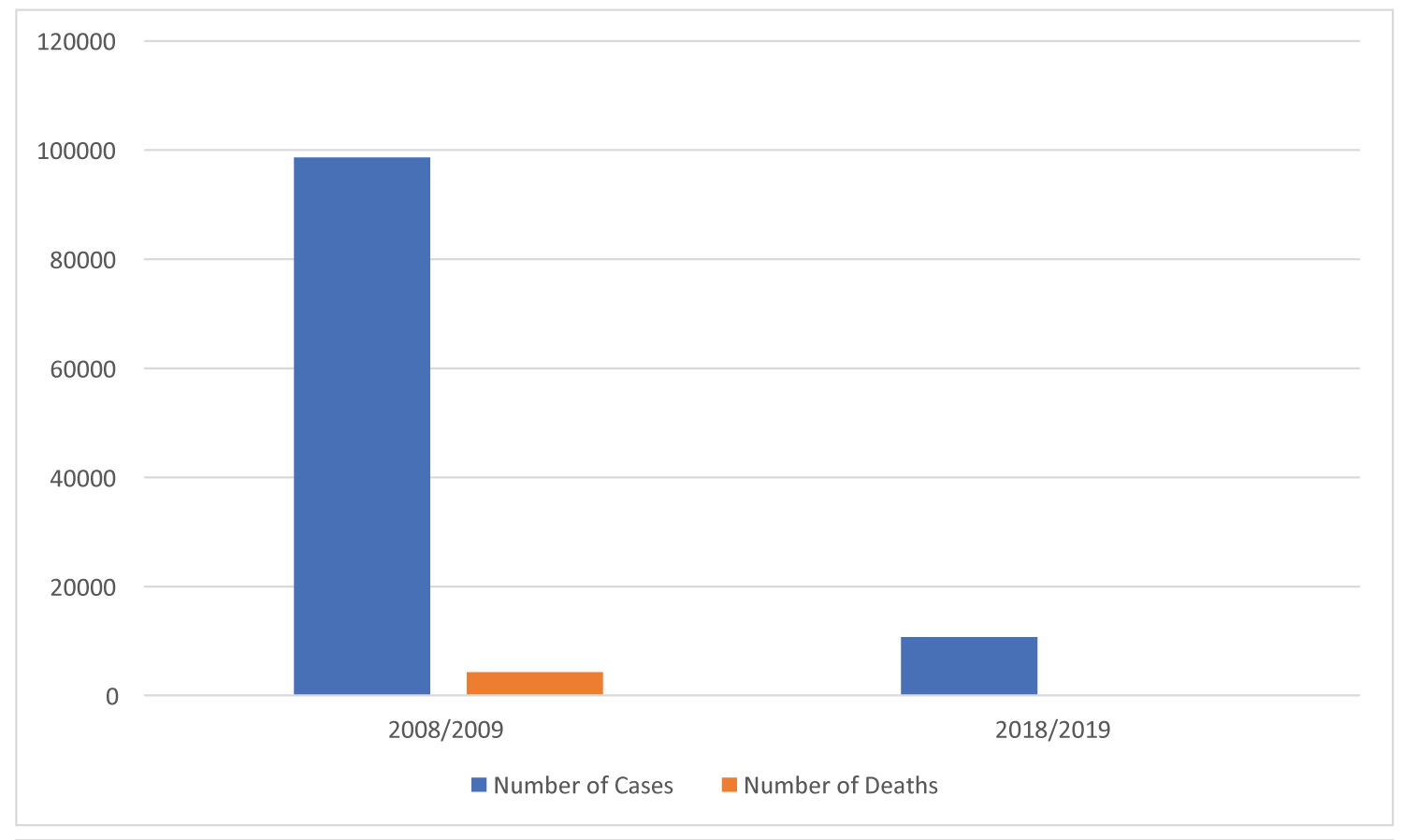 Figure 2: Recorded Cholera Cases and Deaths during the 2008/2009 and 2018/2019 Outbreaks.
Figure 2: Recorded Cholera Cases and Deaths during the 2008/2009 and 2018/2019 Outbreaks.
Source: National Health Information and Surveillance unit under Ministry of Health and Child Care, Zimbabwe [21,22].
View Figure 2
The 2018/2019 outbreak is the most recent outbreak in the country. On the 6th of September 2018, a cholera outbreak in Harare was declared by the Ministry of Health and Child Care (MoHCC) after twenty-five patients were admitted to a hospital in Harare presenting with diarrhoea and vomiting on the 5th of September. The first case was a 25-year-old woman, presented to a hospital and died on the 5th of September. A sample from the woman tested positive for V. cholerae serotype O1 Ogawa. All 25 patients had typical cholera symptoms including excessive vomiting, acute watery diarrhoea and dehydration. The MoHCC declared the outbreak after 11 cases were confirmed for cholera using rapid diagnostic test (RDT) kits and the clinical presentations [15]. Initially thirty-nine stool samples were collected for culture and sensitivity to antibiotics, 17 of which tested positive for V. cholerae serotypeO1 Ogawa [15].
As of 3 October 2018, 8535 cumulative cases, including 163laboratory-confirmed cases and 50 deaths have been reported (case fatality rate: 0.6%) [15]. Of these 8535 cases, 98% (8341 cases) were reported from the densely populated capital city of the country, Harare [15]. The most affected suburbs in Harare were Glen View and Budiriro. Originating in Glenview, a suburb in Harare, the cholera outbreak spread to several provinces in the country including Bulawayo, Manical and, Masvingo, Matabeleland South, Midlands, and Mashonaland Central, East, and West provinces [16]. The disease claimed 69 lives out of a total of 10730 cases during this outbreak with a CRF of 0.64%.
The rapid response was efficient as the Zimbabwean government declared a national emergency five days since the epidemic onset compared to the 2008 to 2009 outbreak when such a declaration was issued more than two months after the first reported case [16]. On the 12th of September 2018, following the declaration of the cholera outbreak as a state of disaster, the Cabinet Committee on Emergency Preparedness and Disaster Management was reactivated and the national government set up an inter-ministerial task- force on the cholera outbreak, involving all major government stakeholders, to provide leadership and to monitor the cholera response efforts and provide regular briefs to the President. The National Emergency Operations Centre (NEOC) was activated on the 21st of September 2018, with the support from local business organizations. The Incident Command Structure (ICS) was finalized and was published by the EOC. The Cholera elimination secretariat began fixing Information and Communications Technology equipment in the EOC in MoHCC of Zimbabwe to support real time reporting. As part of the response four cholera treatment centres were setup in Harare. The WHO began a campaign to vaccinate 1.4 million people in Harare against cholera for people living in areas at most risk of contracting the disease in October 2018 [15].
El T or biotype of V. cholerae O1 is most common in Zimbabwe. Cholera confirmed case in the country is defined as a suspected case in which V. cholerae serogroups either O1 or O139 has been isolated from a stool sample. During the 2008 to 2009 massive outbreak in the country, V. cholerae O1 of either Ogawa or Inaba serotype was identified and many health personnel were not aware of the local and current antibiotic sensitivity patterns of these strains in the country [4] (Ahmed etal.2015). To cover this knowledge gap laboratory tests were conducted and the strains showed variable sensitivity to commonly-used antibiotics, such as tetracycline, doxycycline, and erythromycin; 100% sensitivity was only achieved with ciprofloxacin and azithromycin [4]. Contrastingly during the recent outbreak (2018/2019) V. cholerae O1 serotype Ogawa isolates were found to be multidrug resistant with an unexpectedly high-level of resistance to ciprofloxacin (96.7%, 233/241 of the samples tested)and ceftriaxone (99.6%, 240/241 of the samples tested) [17]. The country’s 2018/ 2019 isolates were susceptible to azithromycin which as a result was used for treatment during the outbreak. However, before this outbreak azithromycin-resistance genes, such asmph(A) or mph(E), were sporadically identified in CTX-M-15-producing 7PET isolates obtained in Zimbabwe from 2010 to 2015 [17]. In future outbreaks the presence of these genes would endanger the use of oral azithromycin or other antibiotic use to treat cholera in Zimbabwe.
Further analysis of the Zimbabwean 2018/2019 bacterial genome showed that the epidemic strain belonged to the new lineage T13 [17]. It was observed that the country’s epidemic strain was highly resistant to antibiotics, as opposed to the one from Yemen and fourteen additional antibiotic resistance genes were identified by the genetic analysis of the strain from Zimbabwe [17,18]. As mentioned earlier, before this epidemic, an antibacterial resistance structure in the bacterial chromosome of cholera vibrios prevented the acquisition of such resistance plasmids and thus stabilised the content of resistance genes. This alone raises the need to understand the coexistence of these two resistance structures in this new T13 lineage in future.
The cholera situation in Zimbabwe is closely linked to lack of safe drinking water, poor sanitation, declining health infrastructure, and reduced health care staff. Cholera outbreaks in Zimbabwe tend to start between November-December. Hence, cholera risks in the country increases with the start of the rainy season and decreases with the start of the dry season. Lack of adequate access to safe water, sanitation and access to healthcare is the main risk factor for cholera outbreaks in the country. The Multiple Indicator Cluster Survey of 2014 reports that the national open defecation is at 31.7%; this affects poor rural people mostly, where 44% of the population practices open defecation [19]. During this survey, Matabeleland North Province recorded the highest proportion of household population with no sanitation facilities and 69.9% of them practiced open defecation, followed by Masvingo (54.5%) and Matabeleland South Province (43.5%). Only 58.7% children aged between 0-2 years had their stool disposed safely [19].
Furthermore, access to improved sanitation in Zimbabwe is at low of 62% (97.5% in urban and 48% in rural); and according to the Multi-Cluster Indicator Survey of 2019 almost 60% of water sources in Zimbabwe are not safe [19,20]. The breakdown of both potable water and sanitation systems and the widespread contamination of available drinking-water sources are considered to be responsible for the rapid and widespread distribution of the epidemics throughout the country. The risk factors associated with the outbreaks included erratic water supplies principally in densely populated suburbs town centres. These areas usually act as epicentres. For instance, during the 2008/2009 and2018/2019 outbreaks, Harare city authorities were incapable to supply enough water for their residents due to poor service infrastructure and the increasing urban 2]. These shortages usually lead to sanitation issues as people began to use unregulated wells and boreholes, leading to people drinking contaminated water.
The deteriorating sanitation infrastructure is leading to issues such as raw sewage flowing in areas country’s biggest cities. Another sanitation issue is of the informal traders selling items such as fish, vegetables and fruits on the streets this issue exacerbates the outbreaks in the country. Hence risk factors for cholera outbreaks in the country include but not limited to contaminated environment i.e., open defecation; sewer bursts and blockages in urban or peri-urban areas, high population density or population density per borehole, low elevation in high-density neighbourhoods, and the presence or number of markets or bus stations in the neighbourhood.
Healthcare workers are critical in any public health interventions. If new outbreaks occurred, they need to be equipped with all the necessary tools needed to control the disease. Attention should be mainly directed to early detection and quick referral for medication to avoid unnecessary chains of disease transmission. Since the main causes of emerging outbreaks is centered on poor infrastructure, the Government of Zimbabwe must invest in improved sewerage infrastructure if cholera is to be eliminated in the country. Furthermore, annual vaccination of individuals residing in high-risk locations is required until such a time when the sewerage and water infrastructure has been improved. Additionally, it is also critical for the country to adopt satellite derived hydro-climatic processes for monitoring conditions associated with cholera outbreaks. This technology can be used to capture environmental conditions related to epidemic cholera thereby providing an early warning system. Furthermore, since the cholera etiologic agent cannot be currently eliminated, it is important to note that V. cholerae, is autochthonous to the aquatic environment therefore prediction of conditions favourable for its growth and estimation of risks of triggering the disease in a given population can be used to alert responders, potentially decreasing the infection and saving lives.
The current study does not involve any human or animal laboratory studies. This work is view article that was based on the available data.
No specific funding was provided for this work.
The authors have declared that no competing interests exist.