Malaria remains a major public health issue in the world especially in the resourced-limited countries. Ghana is not left out as the incidence of malaria still accounts 40% of all OPD cases.
A descriptive cross-sectional study was used to evaluate the quality of malaria case management at Damongo Municipal Hospital. The specific objectives were to: determine the mode of malaria diagnosis, assess the treatment of malaria cases and evaluate the health record management system in the Damongo hospital. A sample size of three hundred (300) malaria cases from November to December, 2019 were reviewed using purposive and multi stage sampling methods.
Results of this study were presented in simple tables and figures. The findings from the study indicated that, most of the cases reviewed were 18 years and above (49%) and majority of them were females (65.3%). Generally, only few clients (31.7%) went through laboratory confirmation before diagnosis was made, but majority (68.3%) were not tested but treatment was on symptom-based diagnoses. Out of those that were tested, 14.3% were positive to malaria parasitaemia. Drugs that were used for the treatment of malaria by the prescribers included Artemether Lumefantrine (AL), Artesunate Amodiaquine (AA) and Quinine (Qn). Majority (73.3%) of them were treated with AL. Regarding adherence to the treatment protocol, 14.3% adhered to the guidelines. Considerable number of clients correctly diagnosed both in the consulting room registers and clients' folders.
Based on the findings of the study, it is recommended that the hospital management should ensure that clinicians are guided by case management protocols to minimize treatment for unconfirmed cases which would reduce unnecessary treatment cost and prevent resistance to anti-malaria drugs.
Malaria, Case management, Quality, Rural health facility, Ghana
The use of quality case management practices or standards has been shown to improve decision-making and services delivered to clients who reported to health with signs and symptoms of malaria, this has helped to reduce undesirable consequences associated with malaria such as; severe morbidity, disabilities deaths, and socio-economic challenges [1].
Malaria is an infectious disease caused by the Plasmodium parasite, which is transmitted by female Anopheles mosquitoes; it is an endemic disease in Ghana and has a perennial transmission which affects all age groups. Some of the typical clinical manifestations are; shivering, fever, and sweating [2]. Malaria is still a burden in many countries around the world, especially in Africa and some Asian countries, including Vietnam. As reported by the World Health organization (WHO), in 2016, there were 91 countries in which malaria is endemic and an estimated 216 million cases of malaria, an increase of 5 million cases compared with 2015. There are 445,650 deaths from malaria, a decrease of 0.11% compared to 2015.
Case management is a process practiced by health clinicians using standard and approved procedures to detect, coordinates, diagnose, treat, monitor, and evaluates any medical condition, usually communicable disease but not always. It begins when a person is identified as having signs and symptoms of the disease requiring medical care; this is achieved through collaboratively assessing the clients by other professionals [3]. Whilst malaria remains the most important diagnosis in most of Africa, and in peripheral settings it is often missed [4]. Several preventive measures/interventions have been put in place to reduce the incidence of malaria in sub-Saharan Africa, such as; free distribution of Long Lasting Insecticide Treated Bed Net (LLIN) [5], Chemoprevention for both pregnant and children under-5, indoor residual spray, killing of mosquito larvae, etc. yet still most of the African countries still battle with malaria management and prevention [6].
Effective case management of uncomplicated malaria is a major strategy for malaria control. This requires appropriate clinical assessment, laboratory proof of the disease either by microscopy or rapid diagnostic test (RDT) prior to treatment with an effective antimalarial [7]. Moreover, in the Abuja declaration of May 2006, aims at achieving and sustaining universal access to appropriate interventions for all populations at risk of malaria. As a result, the goal of malaria control in Ghana is to reduce morbidity and mortality by 75 percent by 2015 [2].
It is important for health workers to adhere to the new guidelines which have been designed to give optimum care to most of the population. Supervision of healthcare centers is needed to ensure quality healthcare, this will allow problematic areas to be identified and subsequently improved upon to make service delivery better [8]. In recent years, many organizations have been working on the development of improved Malaria Case Management (MCM) standard operating procedures, training materials and program guides. These are intended to strengthen the ability of the health care clinical professionals to carry out effective case management practices [1].
According to WHO, malaria is diagnosed clinically and by laboratory findings. Microscopy remains the most established and widely used technique in confirming blood parasitemia. However, in most some developing countries, the lack of microscopic examination in most health facilities, due to lack of equipment and or trained staff, means that health workers must rely on clinical judgement or discretion to treat malaria [9]. Guidelines have been developed by WHO for situations where there are limited diagnostics [9]. A study conducted by Clare, et al. [10] has revealed that, quality of diagnostic support, involving resource management, motivation and supervision greatly affects malaria case management rather than following national guidelines for the diagnosis of febrile illness, clinician behaviour appeared to follow 'mindlines':
In Africa, most health care providers do not fully follow the standards for malaria case management procedures due to inadequate/lack of equipment or technical know-how to detect, diagnose and treat malaria cases. This results in over-diagnosis and or missing other diseases with overlapping symptoms, which is costly financially and in terms of morbidity, mortality, and recovery. Clinicians were found to follow their clinical judgement sometimes rather than guidelines, which incorporated multiple social influences operating in the immediate and the wider context of decision making [10].
According a study in Namibia by Van Jong &Wendte [11], the over-diagnosis of malaria at hospitals and health centers has been widely reported. The over-diagnosis involved both the prescription of anti-malarial to patients without evidence of malaria parasitaemia and the frequent absence of treatment for alternative causes of disease.
In Ghana, the Standard Treatment Guidelines (STG) and the Antimalarial Drug Policy, stipulate how malaria should be managed. However, facility surveys in Ghana have shown that health workers frequently do not comply with treatment guidelines [8]. The disease has a crippling effect on the economic growth and perpetuates vicious cycles of poverty [12]. Malaria control and prevention have been recognized as an essential prerequisite, this requires accurate, adequate and reliable testing and treatment regimen which could improve the quality of Malaria Case Management (MCM) in the country. A survey conducted at the coastal, forest and savannah regions of Ghana by Ama, Kristia, Ulrik & Asante [13], reported that, "assessments such Parasitological needed to identify suspected malaria were generally low in all the facilities visited, with some differences in the quality of malaria treatment given to clients or patients".
The situation in the West Gonja Municipality was similar to the national phenomenon, the municipality recorded progressively high prevalence of malaria cases; 17% in 2016, 29% in 2017 and 39% 2018 of 50,504. This study, therefore, sought to determine the mode of malaria diagnosis, treatment and health record management system in the Damongo Municipal Hospital (DMH). The general objective of the study was to evaluate the quality of the management of malaria cases among clients who attended Damongo Municipal Hospital (DMH) in the Savannah region.
A Cross-sectional survey was conducted to evaluate the quality of care in the management of malaria cases through review of existing records. A descriptive cross-sectional study was chosen because; It is relative quick and easy to conduct without follow ups. It also provided a "snapshot" and can accurately explore the characteristics of the population of at once. With a randomized sampling, the study could represent the entire patients who reported of malaria in the Damango Municipal Hospital (DMH).
The study population was all clients/patients who attended the rural health facility within the last three months in 2019. The sample of all malaria cases recorded in both children and adults in the last three months of 2019.
The Dependent variable was quality of malaria case management.
The independent variables of this study included: background information, mode of malaria diagnosis and treatment of malaria cases and also health record management system. The Background variables included age and sex. Mode of malaria diagnosis focused on the number tested or untested, status of those tested (+/-) of malaria. The treatment of malaria cases included; treated with Artemether-Lumefantrine (AL), Artesunate Amodiaquine (AA), and adherence to management protocol. On evaluating record management system; comparison was made on consulting register and patients' folder regarding diagnosis on principal and additional diagnosis.
A sample size of 300 existing patients' records on malaria was reviewed. Purposive and Multi stage (with simple random) sampling methods were used for selecting three consulting rooms for the 300 existing records for the last 3 months of 2019, because there were many consulting rooms. Three consulting rooms were chosen at random, thus 100 malaria cases from each which sum up to 300.
A systematic sampling technique with an interval of two (2) was used from the first folder in each consulting room to select all the 300 existing records. The format for the selection of the patients' records was;
r, (r+1k), (r+2k), (r+3k), (r+4k), (r+5k), (r+6k), (r+7k),......(in that sequence)
Where r = 1 (thus the first sample taken)
K = 2 (thus the sampling interval used or the constant)
Sample = 1, (1+2x1), (1+2x2), (1+2x3), (1+2x4), (1+2x4), (1+2x5), (1+2x6), (1+2x7),......
= 1, 3, 5, 7, 9, 11, 13, 15,..................................
An observational/review check list was used in gathering data for the study. It comprised four sections; Background information (age and sex), mode of diagnosis (number tested or not tested, status of those tested), treatment of malaria cases (treated with Artemether-Lumefantrine (AL), Artesunate Amodiaquine (AA), and adherence to management protocol) and also health record management system (comparison was made on consulting register and patients' folder regarding diagnosis on principal and additional diagnosis).
The data collection instrument (observational checklist) was written in English language, the records review lasted 20 minutes on the average. Data was entered in the checklist personally from the consulting rooms. After this, respective folders in the OPD were tracked to ensure validity of documentation.
Statistical Package for the Social Sciences (SPSS) version 22.0 software was used for data analysis. Frequency distributions were obtained and these were summarized in tables. The tables comprise of measurement items, frequencies and percentages.
To reinforce and assess reliability of the instrument in this research, it was pre-tested from March 15, 2021 to March 16, 2021 on nine existing medical records with similar characteristics as the study population at the consulting room (thus Damongo Municipal Hospital). Analyzed results demonstrated an increasing degree of precision with each question. The reason for choosing the above-mentioned setting was it represented the study area with the same characteristics.
The study was approved by the Ethics Review Committee of the Ghana Health Service (GHS) with reference number GHS-ERC: 057/02/21 before data were extracted from patients' records. Community entry and exit procedures were duly followed at the rural health facility during the study. Permission was also sought and granted, from the various in-charges of the consulting rooms. Again, the MHD and the hospital were assured that data collected would be used for the intended purpose. All data collected were kept confidential and anonymous which were only accessible to the research team.
From the Figure 1, it was revealed that, 147 (49%) of the cases reviewed were 18 years and below, whiles 83 (27.3%) and 14 (4.6%) were 5-17 years and children under one year respectively.
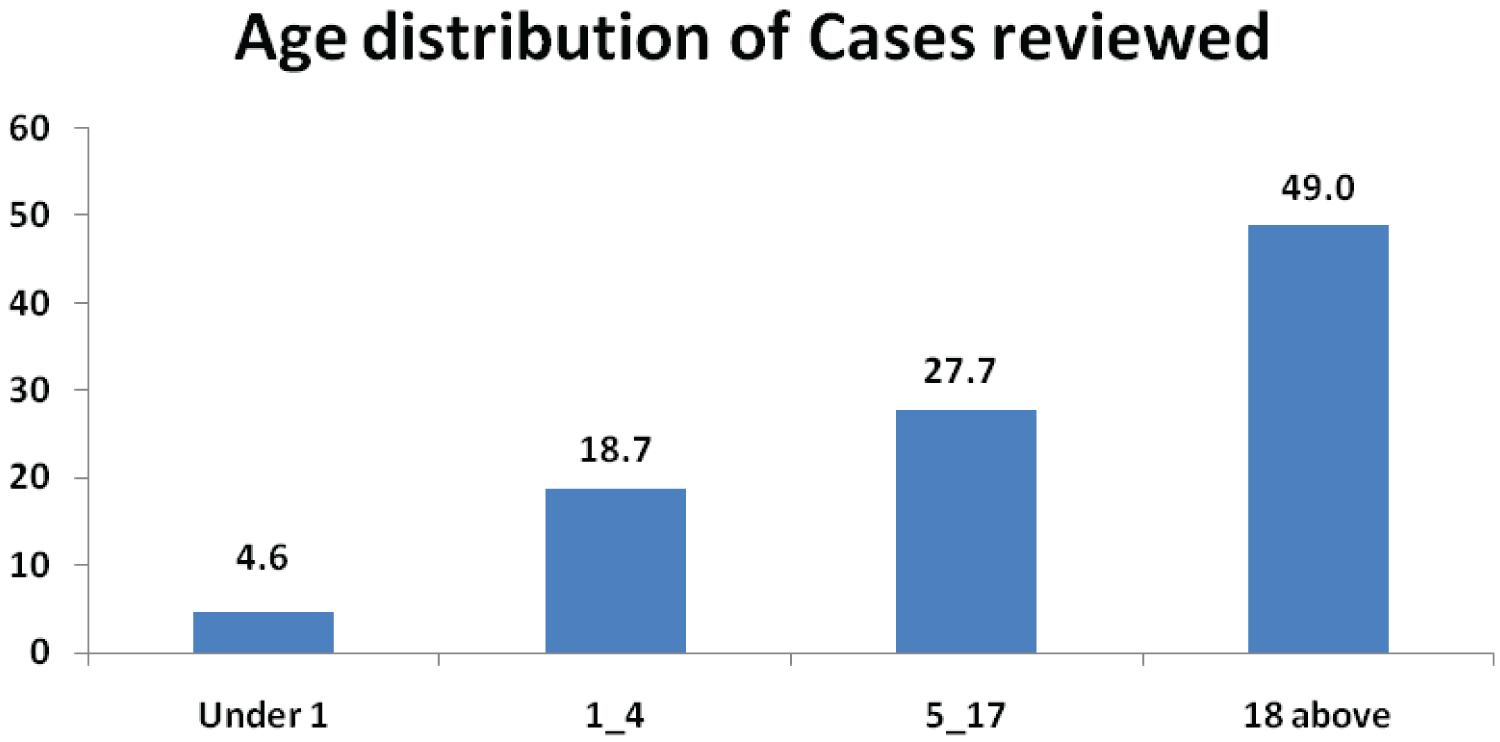 Figure 1: Age distribution of Cases reviewed.
View Figure 1
Figure 1: Age distribution of Cases reviewed.
View Figure 1
Figure 2 shows that, 196 (65.3%) of the cases reviewed were Females and 104 (34.7%) males.
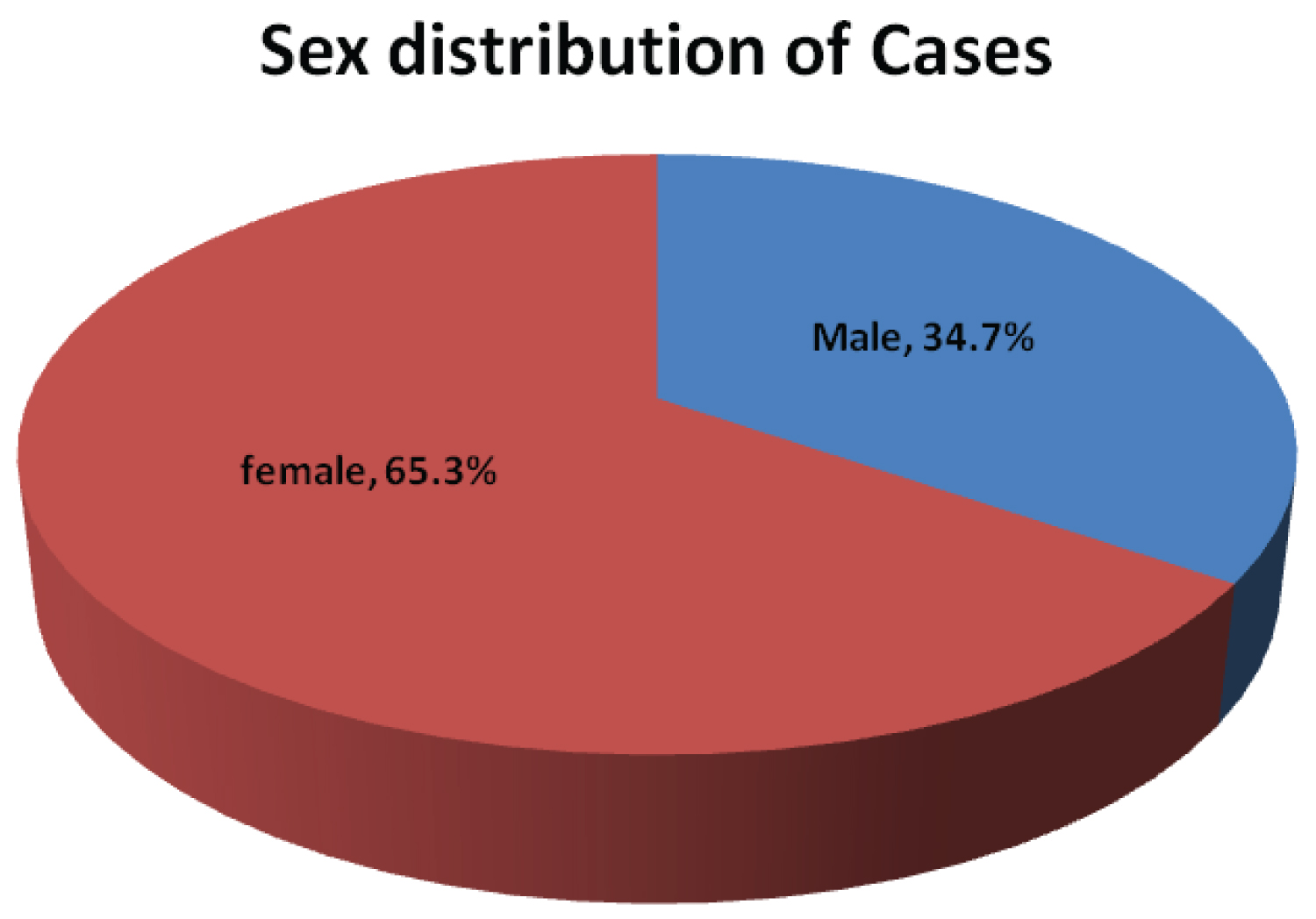 Figure 2: Superselective angiography: Determined by the right recurrent artery of Heubner and normal perforating arteries extending from the aneurism neck.
View Figure 2
Figure 2: Superselective angiography: Determined by the right recurrent artery of Heubner and normal perforating arteries extending from the aneurism neck.
View Figure 2
Table 1 indicates that, out of the 300 cases, 95 (31.7%) were confirmed by laboratory investigations before diagnosis was made. But majority 205 (68.3) were not tested before treatment.
Table 1: Cases confirmed by Laboratory Investigations. View Table 1
Table 2 above, out of the 95 cases tested, 14.33% and 17.33% were positive and negative respectively. Whiles 205 (68.34%) were not tested before by the laboratory unit before treatment.
Table 2: Outcome of laboratory investigation. View Table 2
From the Table 3, 95.5%, 23.3%, and 3.3% were prescribed Artemether-Lumefantrine (AL), Artesunate Amodiaquine (AA), and Quinine (Qn) respectively. However, 4.5% of cases prescribed with AL were given the wrong dosage, 7.1% for AA. Whiles 20.0% were give Qn incorrectly.
Table 3: Status of malaria treatment to clients' (Prescribed medication). View Table 3
In Table 4, 43 (14.3%) of cases reviewed were followed according to the protocol, thus; laboratory investigations were done and given the right dosage of anti-malaria treatment. But 85.7% of the cases were not followed according to the protocol/standards, thus; were either not tested before treatment or given incorrect dosage or both.
Table 4: Adherence to Case Management Protocol. View Table 4
From Table 5, 294 (96.3%) of principal diagnosis matched with the consulting register against clients' folders, whiles 6 (3.7%) were unmatch.
Table 5: Comparing Principal Diagnosis on clients' records to Consulting room Register. View Table 5
Table 6: Comparing Additional Diagnosis on clients' records to Consulting Room Register. View Table 6
From Table 5, 294 (96.3%) of principal diagnosis matched with the consulting register against clients' folders, whiles 6 (3.7%) were unmatch.
The study reviewed 300 attended malaria cases in 2019 in three consulting rooms: a response rate of 100% was achieved. Results revealed that most 147 (49%) of the cases reviewed were 18 years and above, 27.7% and 4.6% were 5-17 years and children under one year respectively. 196 (65.3%) of the cases were Females and 104 (34.7%) males.
Only few, 95 (31.7%) were confirmed by laboratory investigations before diagnosis was made, but majority 205 (68.3) were not tested before diagnoses and treatment made. It was observed after data collection that; this practice was not in line with the guidelines for managing malaria cases. The consulting rooms selected mostly rely on laboratory microscopy for testing and diagnosis with few occasions where RDTs were used. On the contrary, the national standards for investigating malaria cases thus all cases of suspected malaria must be tested (with parasitological test, microscopy and Rapid Diagnostic Test), and should be supported by the quality assurance programmes amongst others.
Only few, 95 (31.7%) were confirmed by laboratory investigations before diagnosis was made, but majority 205 (68.3) were not tested before diagnoses and treatment made. It was observed after data collection that; this practice was not in line with the guidelines for managing malaria cases. The consulting rooms selected mostly rely on laboratory microscopy for testing and diagnosis with few occasions where RDTs were used. On the contrary, the national standards for investigating malaria cases thus all cases of suspected malaria must be tested (with parasitological test, microscopy and Rapid Diagnostic Test), and should be supported by the quality assurance programmes amongst others.
On treatment of cases, 95.5%, 23.3%, and 3.3% were prescribed with Artemether-Lumefantrine (AL), Artesunate Amodiaquine (AA), and Quinine (Qn) respectively. However, 4.5% of cases prescribed with AL were given the wrong dosage, 7.1% for AA. Whiles 20.0% given Qn were incorrectly. A similar study agreed with our findings that, "a reasonable proportion of doses of ACTs were prescribed incorrectly for clients and proportion of malaria cases were not treated according to the treatment guidelines [15,16].
Also, it was revealed in this study that, 94.2% of them were given their drugs according to the treatment guidelines (thus testing, diagnose, treat given the right treatment), and 5.7% of the cases were not. Although majority of prescriptions conformed to the antimalarial treatment policy, the few proportion (5.7%) not in accordance with the policy may cause unnecessary increases in drug costs, resistance as well as increasing the risk of adverse events.
In addition, the findings also revealed that, 43 (14.3%) of cases were tested before treatment according to the protocol, thus; laboratory investigations were done before given the right dosage of anti-malaria treatment. But the protocol/standards were not adhered to for 85.7% of cases, thus; were either not tested before treatment or given incorrect dosage or both. This implied the providers do not see the importance of investigating malaria cases. But in a previous study by Rowe, et al. [17], it was shown that health care providers' adherence to treatment guidelines remains critical to the success of any new drug policy. However, results from health facility surveys have indicated that health workers frequently do not comply with treatment guidelines (only 31.7% were tested before given treatment).
This study looked at documentation of malaria cases from consulting register to its corresponding folder with two variables taken into consideration thus; principal diagnosis and additional diagnosis. With the principal diagnosis, most (96.3%) of the total cases in consulting register matched with its corresponding folders but 3.7% were unmatched. Whilst in the additional diagnosis 98.0% consulting register matched with the folder, and 2% did not match with the corresponding folder. In their findings, Chilundo, et al. [18] also recorded 81.2% discrepancies between the register and clients' folder, and concluded that this may create inconsistencies either over-reporting or under-reporting of malaria cases. This statement concord with this study's findings.
This research observed, the documentation process and filing system. Despite inadequate space at the OPD, the facility was adhering to the filing system making sure that patient's records are well protected for confidentiality, this contradicts with the research made by [19] revealing misfiling and multiple patients' folder. Also considering how patients' diagnosis and treatment was documented, it was not encouraging due to the fact that the handwritings of the clinicians were not clear.
Comparison made between the principal diagnosis on clients' records to consulting room register revealed that, 294 (96.3%) of principal diagnosis made matched with the consulting register against clients' folders, whiles 6 (3.7%) were unmatched.
Furthermore, the study showed that most (98.0%) of additional diagnoses made matched with the consulting register against clients' folders, whiles 6 (3.7%) were unmatched.
Generally, only few clients went through laboratory confirmation before diagnosis was made, but majority were not tested but rather, some clinicians rely on symptom-based diagnoses. It was revealed that, most of the cases were not given treatment according to guidelines/protocols (thus testing, diagnose, treat given the right treatment). Additionally, undesirable number of cases were tested before treatment whiles majority of the cases were not thus; they were either not tested before treatment or given incorrect dosage or both. Considerable number of clients correctly diagnosed both in the consulting room registers and clients' folders. Lastly, the study revealed some consulting rooms do not have Job Aid for Malaria Case Management protocols. Based on the findings of the study, it is recommended that the hospital management should ensure that clinicians are guided by case management protocols to minimize treatment for unconfirmed cases which would reduce unnecessary treatment cost and prevent resistance to anti-malaria drugs. The hospital management could organize in-service or refresher training for staff on malaria case management protocols which would enhance their current knowledge on malaria treatment and prevention. Future research could be conducted on factors contributing to why clinicians rely on symptom-based diagnoses instead of laboratory investigations.