Background: COVID-19 does not necessarily affect the respiratory system only and can cause life threatening systemic condition. I present a case of pulmonary hemorrhage and (ANCA) C vasculitis with type I respiratory failure as a presentation of COVID-19.
Case presentation: 45-year-old Saudi lady with no history of chronic medical problems, non-smoker, no history of any drug intake, married with 3 off springs, presented to our ED with massive hemoptysis with severe shortness of breath. On arrival: Patient was conscious, oriented & pale, Hypoxic on Oxygen via face mask 15 L/min, No clubbing, No L.L. edema, No palpable L.Ns. Chest: B/L inspiratory fine crepitation. CXR: B/L mid & lower zone consolidations sparing the apices & the angles. Lab investigations done revealed her Hb was 5.2 gm/dl, with disturbed kidney functions (urea: 11, creatinine: 284) so patient received 2 units PRBCs urgently, then shifted to ICU isolation where Swab screen for COVID19 was taken. CT chest without contrast findings are likely suggestive of diffuse alveolar hemorrhage. After 12 hours: Patient became hypotensive BL/p 80/50 with disturbed level of consciousness so intubated and mechanically ventilated (MV).ECG and echo cardio done and showed: No abnormalities detected and the Swab result was positive for COVID19 so started levophed infusion with continuous renal replacement therapy and gave patient pulse steroid for 3 days then plasma pharesis for 5 days. After that, intravenous immune-globin was added With Caspofungin being added on and tigecycline i.v. The results of serology and immunology showed negative for HIV and hepatitis and other connective tissue diseases while (ANCA) C was highly positive. After 3 weeks: Patient still on MV, we gave patient anti-CD20. Patient condition was deteriorated and after 4 weeks: Patient arrested and died on MV.
Conclusion: Has evidence of diffuse alveolar hemorrhage and vasculitis as a complication of COVID-19 with poor prognosis.
COVID-19, Alveolar hemorrhage, Vasculitis
ANCA: Antinuclear Cytoplasmic Antibody; (AGBM) AB: Anti-Glomerular Basement Membrane Antibody; CPR: Cardiopulmonary Resuscitation; DAH: Diffuse Alveolar Hemorrhage; ED: Emergency Department; GPA: Granulomatosis with Polyangiitis; HIV: Human Immunodeficiency Virus; IV IG: Intravenous Immune-Globin; WG: Wegener's Granulomatosis
COVID-19 is primarily a disease with respiratory manifestations, this virus has different clinical presentations including; vascular thrombosis, gastro-intestinal [1], dermatological and other organs involvement which are highly suggestive of the presence of systemic vasculitis [2]. There are some speculations that the virus could be a direct invader of endothelial cells of blood vessels all over the body thus; vasculitis could be a major pathological pattern of this disease [3,4].
Vasculitis is an inflammation of the blood vessels. The blood vessel wall become weakened, thin that it ruptures resulting in bleeding into the tissue [5]. Granulomatosis with polyangiitis (GPA) previously known as Wegener's granulomatosis (WG) is a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys [6]. GPA can be affect the lung and cause diffuse alveolar hemorrhage (DAH) which is a life-threatening and medical emergency and presents with hemoptysis, anemia, and diffuse alveolar infiltrates [7].
Many causes of DAH as vasculitis, coagulation disorders, drugs, inhaled toxins, cardiac causes as mitral valve disease or organ transplantation [8]. Vasculitis with DAH has poor prognosis (75% died) especially if associated with renal affection and protease 3 was positive [9]. In this case, other causes of DAH not present (no history of any medical illness, drug intake or organ transplantation), no mitral valve diseases and toxicologist saw the patient who said this condition not with inhaled toxin as iso-cyanide or cocaine and toke blood and urine samples for detection of any toxins, the blood sample came negative So the emerging evidence of diffuse alveolar hemorrhage and vasculitis as a complication of COVID-19 with poor prognosis.
45-year-old Saudi lady with no history of chronic medical problems, non-smoker, no contact to birds nor animals, no history of any drug intake, married with 3 off springs, presented to our ED with massive hemoptysis.
On arrival: Patient was conscious, oriented & pale, O2 saturation was 90% on Oxygen via face mask 15 L/min, pulse 120/min regular, BL/P 110/65 mmHg, respiratory rate 25/min. No clubbing, No L.L. edema, No palpable lymph node. Chest: B/L inspiratory fine crepitation.
Lab investigations done revealed her Hb was 5.2 gm/ dl, with disturbed kidney functions (urea: 11, creatnine: 284).
CXR: B/L mid & lower zone consolidations sparing the apices & the angles. ECG: Sinus tachycardia rate was 120/min so patient received 2 units PRBCs urgently, then shifted to ICU isolation where Swab screen for Covid-19 was taken Patient was kept on BIPAP alternating with high flow nasal cannula with septic workup being sent and started on broad spectrum antibiotics (Figure 1).
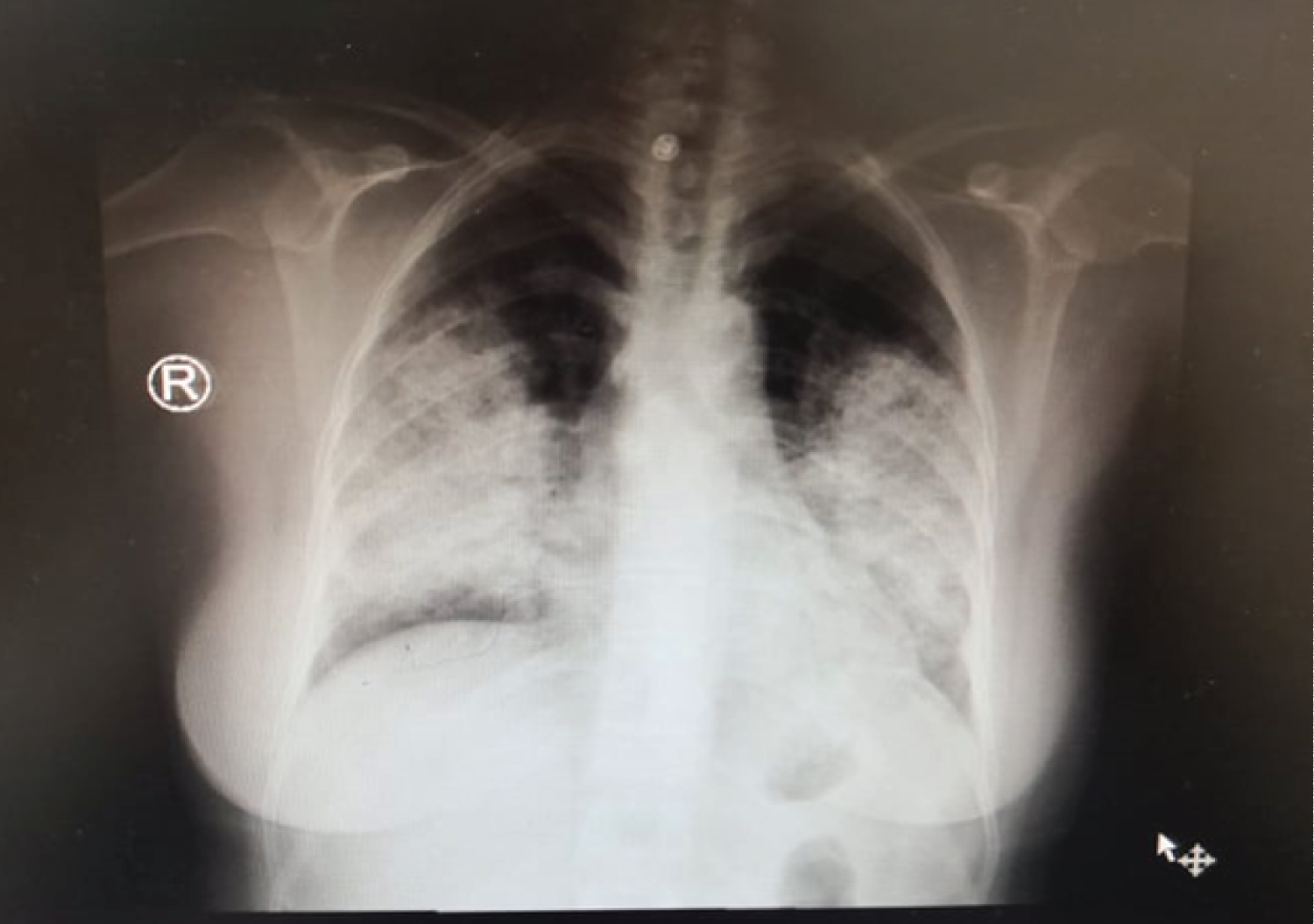 Figure 1: CXR: B/L mid & lower zone consolidations sparing the apices & the angles.
View Figure 1
Figure 1: CXR: B/L mid & lower zone consolidations sparing the apices & the angles.
View Figure 1
CT chest without contrast was done revealing wide spread lung patchy consolidations with central & peripheral distribution, permeated by GGO & crazy paving pattern. The apices & lower zones are relatively spared. Findings are likely suggestive of diffuse alveolar hemorrhage.
After 12 hours: Patient became hypotensive BL/p 80/50 with disturbed level of consciousness so intubated with too much blood came from endotracheal intubation & put on MV and cardio consultant saw the patient and ECG: Sinus tachycardia rate 125/min & echo-cardio done has normal left ventricular function, ejection fraction 65% with no valve abnormality and right side of the heart not dilated with systolic pulmonary arterial pressure was 28 mmHg so started on levophed infusion and put patient on CRRT and gave patient pulse steroid 1 gram methylprednisolone for 3 days and Swab result was positive for COVID-19.
After 2 days: Patient started on plasma pharesis for 5 days. After finish plasma pharesis, IVIG was added With Caspofungin being added on and tigecycline i.v. Some results came: PT-14.4, PTT-26, INR-1.1, ESR-100, CRP-252, D-dimer-1, feritin365 and the serology and immunology showed negative for HIV and hepatitis C&B and (ANCA)C was highly positive 135 AU/ml (normal range up to: 13), C3 was highly positive 254 AU/ml (normal range up 15) while (ANA, RF, Anti-double stranded DNA, Anti-scleroderma 70, anti RU and LA, and (AGBM) antibody were negative. All serology and immunology tests repeated after 1 week to confirm results and still were nearly the same results. While after 2 weeks 2nd swab for COVID19 was taken and still positive. After 3 weeks: Patient still on MV, we gave patient anti-CD20 (Rituximab 500 mg). After 4 weeks: Patient arrested on MV; Cardiopulmonary resuscitation (CPR) started according to protocol with adrenaline ampoules being given, unfortunately patient didn't revive & declared dead (Figure 2).
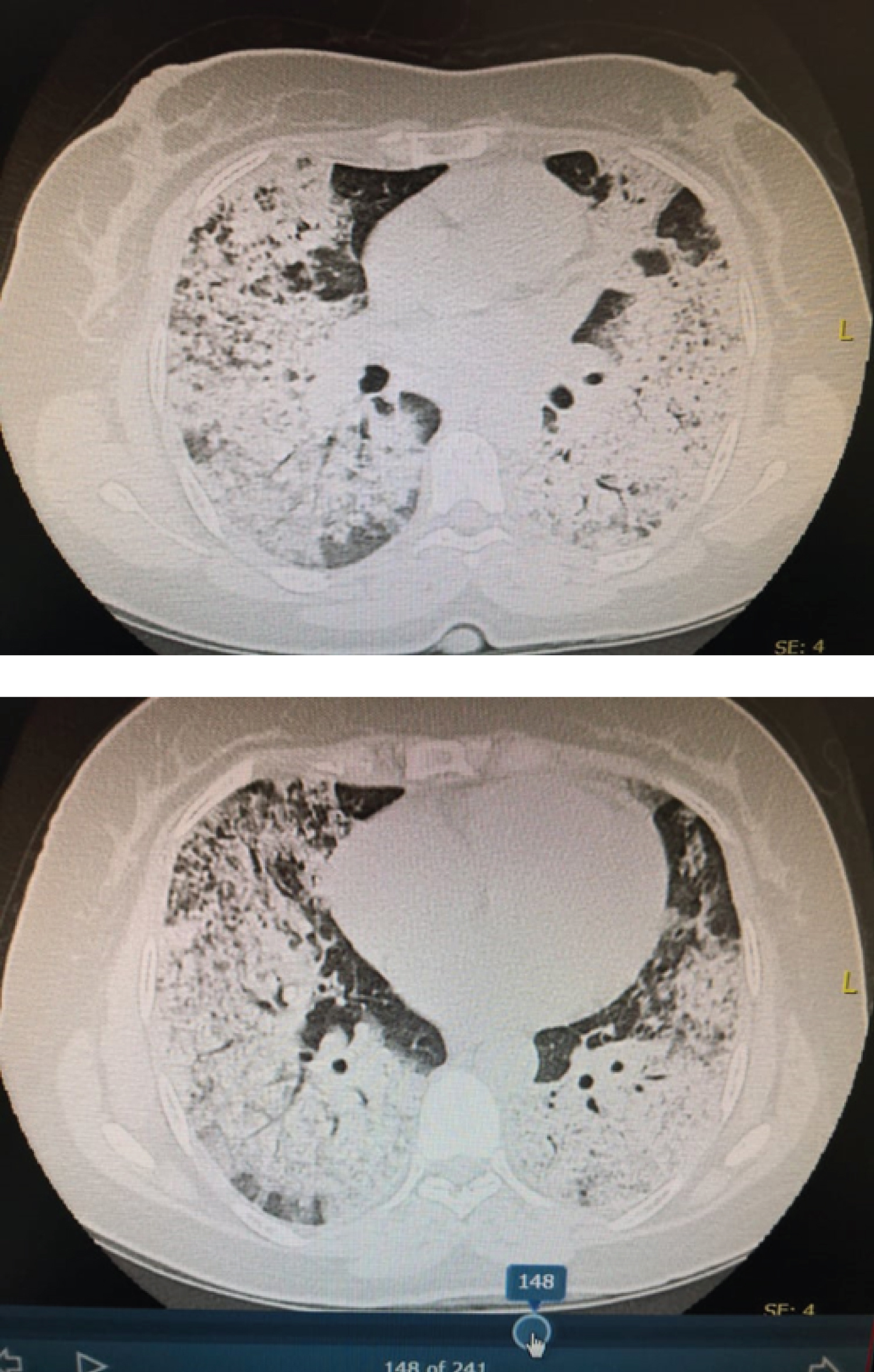 Figure 2: Diffuse alveolar hemorrhage. View Figure 2
Figure 2: Diffuse alveolar hemorrhage. View Figure 2
Table 1: Some laboratory parameters of the patient. View Table 1
COVID-19 can cause diffuse alveolar hemorrhage and vasculitis with a poor prognosis. Need more studies to explain that its immune-pathogenesis.
• Ethics approval and consent to participate: is available when need.
• Consent for publication: The written consent (from relative of the patient): Is available when need.
• Availability of data and materials: All data of the patient is available on computerized patient file in recording department of King Fahd hospital-Almadina Almonoura-KSA. www//KFHM-moh.gov.sa.
• Competing interests: Not present in this section.
• Finding: WHO, up to date, Google search.
• I responsible for data collection interpretation of data and writing the manuscript.
• Author's contributions: All authors have read and approved the manuscript. AE: interpreted of CT; MF: analysis and interpretation of serology results.
• Acknowledgments: Dr /Mohamed EL-Sayed and to all stuff of chest diseases.