As community transmission of COVID 19 peaks in our environment, more children are presenting with moderate to severe disease, as against the earlier notion of asymptomatic to mild disease severity in children. Mortality from COVID-19 infection in children with no apparent comorbidity is still rare. Our aim is to describe a fatal case of COVID-19 in a Nigerian girl with no background medical conditions.
The 8-year-old girl presented with fever, cough and difficulty with breathing. She was febrile, in severe respiratory distress with SPO2 of 74%. Her chest X-ray showed extensive patchy and ground glass air space opacifications with some peripheral distribution. Diagnosis of SARS-CoV-2 infection was confirmed with GeneXpert platform using the Xpert Xpress SARS-CoV-2 assay on nasopharyngeal sample. She died on the 4th day on admission. Children admitted for COVID-19 with or without comorbidity should be closely monitored for early detection and prompt management of complications that may occur in them.
COVID-19, SARS-CoV-2, Comorbidity, Children, Nigeria
Coronal virus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in China in Dec 2019 [1] and has rapidly spread to other parts of the world since then. The first case of COVID-19 was reported in Nigeria in March 2020 and the country is currently having over 148,500 confirmed cases and over 1779 deaths from complications of COVID-19 infection [2].
The clinical manifestation of COVID-19 in children is generally reported to be of lesser severity and of better outcome when compared to adults [3-7]. Among the proposed factors for the reduced severity in children include the high levels of angiotensin-converting enzyme 2 (ACE-2) activity, trained immunity due to routine live vaccines and frequent viral infections, cross immunity to other coronal virus infections as well as the absence of ageing related immune-senescence [8]. Children also have good lung regenerative capacity which could explain the early recovery of COVID-19 in them [9].
COVID-19 infection mortality is rarely reported in children and most of the few reported cases occurred in children with comorbidity [3,9]. A cross-sectional study [5] and a case series report [4] of Nigerian children with COVID-19 infection reported no mortality. However, in another larger retrospective National study [7], 2 cases of COVID-19 fatalities were reported in children aged 0-13 years but the authors did not indicate whether the 2 children had any underlying comorbidity or not. We report a case of an 8-year-old girl who had no apparent underlying medical conditions but died of COVID-19 related complication.
An 8-year-old girl presented to our facility with a week history of fever, 5 days' history of cough and difficulty with breathing of 4 days prior to presentation. Fever started as low grade but later became high grade and continuous. Cough was insidious in onset, and gradually worsened in frequency and intensity and persisted till presentation. It was productive of non-foul smelling, whitish coloured sputum. Difficulty in breathing started 3 days into the illness, insidious in onset and characterised by fast breathing and chest wall indrawing. No orthopnoea, paroxysmal nocturnal dyspnea, nor body swellings. This was the first episode of difficulty with breathing in her life.
There was neither history of contact with anybody with similar symptoms nor history of any one died of similar symptoms in the neighbourhood. She lived in a village and no history of recent travels.
She was not a known asthmatic, diabetic or sickle cell anaemic patient. No history of past hospital admissions, blood transfusions or surgery. She was growing well compared to peers and siblings.
On account of the above symptoms, she was admitted for 2 days at a General Hospital where some parenteral and oral drugs were administered without significant improvement in her clinical condition. She was thereafter discharged on request and presented to a private hospital from where they were verbally referred to our facility.
She came in with severe respiratory distress (laboured breathing, flaring ala nasi, subcostal and intercostal recession and SPO2 - 74% in room air), febrile (axillary temperature of 39.4 °C), moderately pale, anicteric, nil palpable peripheral lymphadenopathy, and no pitting pedal oedema. Her weight was 21 Kg (10th percentile) and height was 123 cm (25th percentile).
She was tachypneic (respiratory rate of 80 cycles/minute), had a symmetrical chest with centrally located trachea. Percussion note was dull globally but worse on the right hemithorax, with poor air entry and wide spread crepitations (worse on the right hemithorax).
Her pulse rate was 160 beats/minute (tachycardia) regular, moderate volume and her blood pressure was 100/70 mmHg. Apex beat was displaced to the anterior axillary line on the 6th left intercoastal space. Normal heart sounds were heard.
Her abdomen was full and moved with respiration. Her liver was 3 cm below right coastal margin soft and tender. The spleen was not palpably enlarged. She was conscious but agitated. Musculoskeletal examination was essentially normal.
An initial working diagnosis of severe pneumonia with congestive heart failure was made with a differential diagnosis of severe COVID-19 infection. She was commenced on intranasal oxygen via nasal prong at 3 L/min, intravenous Ceftriaxone 75 mg/kg/day and intravenous Frusemide 1 mg/kg 12 hourly.
Her full blood count showed WBC - 12 × 103/µl, Lymphocytes - 2.8 × 103/µl (23.1%), Neutrophils - 7.6 × 103/µl (63.6%), Other white cells - 1.6 103/µl (13.3%), PCV - 43.1%, HBG - 13.8 g/dl, MCV - 78.5 FL, MCH - 25.1 pg, MCHC - 32.0 g/dl, Platelets - 342 × 103/µl. Serum electrolytes, urea and creatinine results showed Na - 127 mmol/l (135-150), K - 4.3 mmol/l (3.4-5.3), Chloride - 105 mmol/l (98-110), HCO3 - 25 mmol/l (24-32), Urea - 3.2 mmol/l (2.5-6.5), Creatinine - 71 µmol/l (9-126). Malaria parasite blood film was negative.
Chest X-ray (Figure 1) showed extensive patchy and ground glass air space opacifications with some peripheral distribution involving almost the entire right lung fields. Similar but to a lesser extent patchy opacity are seen involving the left lung fields more within the middle and lower lung zones. The diaphragmatic outlines are indistinct due to the aforementioned opacities. The cardiac size could not be measured due to the opacities which had silhouetted the cardiac borders.
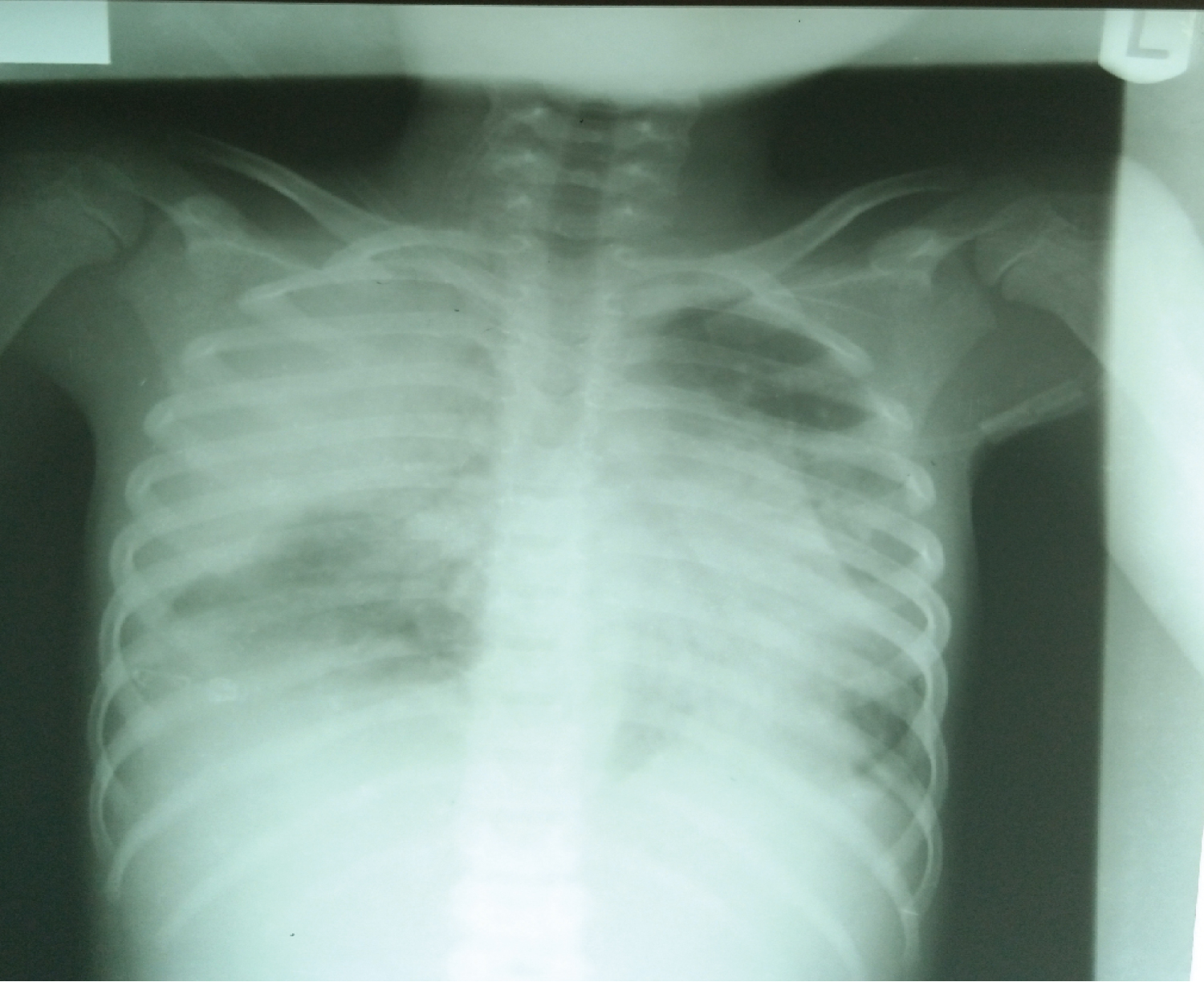 Figure 1: Chest radiograph.
View Figure 1
Figure 1: Chest radiograph.
View Figure 1
As at 48 hours on admission, a suspicion of severe COVID-19 infection was strengthened based on the persistence of her symptoms, worsening SPO2 despite intranasal oxygen, coupled with the chest radiographic findings. She was isolated and Nasopharyngeal swab was taken for Gene Xpert Xpress Assay for SARS-CoV-2. Azithromycin 5 mg/kg daily and intravenous hydrocortisone 4 mg/kg 8 hourly were added to her treatment based on our COVID-19 management protocol. Oxygen delivery was increased to 5 l/minute.
Her clinical condition further deteriorated and unfortunately died on the 4th day of admission. The Xpert Xpress Assay for SARS-CoV-2 result came out Positive after her demise.
This is a case report of fatal SARS-CoV-2 infection in an eight-year-old Nigerian girl who was previously healthy, without histories of underlying diseases, including sickle cell anemia, asthma, cardiac disease, diabetes mellitus, hepatic disease, or malignancy. Mortality from COVID-19 infection in children with no apparent comorbidity is generally rare and to our knowledge, a similar case has not been reported from Africa.
In a study in the United states by Bixler, et al. [10] where 121 case of COVID-19 related deaths were reported in children below the age of 21 years, 30 (25%) were previously healthy (no reported underlying medical condition), 91 (75%) had at least one underlying medical condition, and 54 (45%) had two or more underlying medical conditions. The most frequently reported medical conditions were chronic lung disease, includ¬ing asthma (34 [28%]), obesity (33 [27%]), neurologic and developmental conditions (26 [22%]), and cardiovascular conditions (22 [18%]). In another study from United Kingdom, Swann, et al., [3] reported a mortality of 1% (6 of 627) among children admitted for COVID-19 with all the fatal cases having profound comorbidity. Soumana, et al. [11] reported a fatal case of COVID-19 in an infant with severe acute malnutrition admitted to a Paediatric Ward in Niger.
Our patient presented with fever, cough and difficulty with breathing which are the commonly reported symptoms of COVID-19 [3,8,12]. However, these symptoms are not peculiar to COVID-19 as other acute respiratory tract infections (like bacterial pneumonia) can present the same way. Our initial working diagnosis was pneumonia because this is very common in our environment and it is a major cause of mortality in children.
Her chest radiography findings of extensive patchy and ground glass air space opacifications with some peripheral distribution involving both lungs strengthened our suspicion of viral pneumonia most likely due to SARS-CoV-2. Although, there is no single feature of COVID-19 pneumonia on a chest radiograph that is specific or diagnostic but the published literature reveals general hallmarks of SARS-CoV-2 infections to include CXR findings of bilateral pulmonary infiltrates with a tendency toward the lung periphery [13,14]. Also Chest CT findings of bilateral and peripheral ground glass and consolidated opacities, with an absence of concomitant pulmonary nodules, cavitation, adenopathy and pleural effusions are generally considered as features of COVID-19 pneumonia [14]. Chest CT could not be done on account of the cost and it was not readily available.
Diagnosis of SARS-CoV-2 infection was confirmed in our patient with GeneXpert platform using the Xpert Xpress SARS-CoV-2 assay on nasopharyngeal sample. The GeneXpert, is a cartridge-based nucleic acid amplification machine that makes use of the polymerase chain reaction. It is a reliable PCR-based test with over 95% sensitivity and specificity [15].
The management of this case was challenging in view of our resource-constraint setting. Confirmatory diagnosis of SARS-CoV-2 pneumonia could not be made until after the demise of the patient. Rapid collection and testing of appropriate specimens from patients for COVID-19 is crucial to clinical management and favourable outcome. Our hospital had no functional paediatric intensive care unit with facilities necessary to provide organ function support as needed.
Although, COVID-19 infection is generally reported to be mild in children and less fatal, however, children admitted for COVID-19 with or without comorbidity should be closely monitored for early detection and prompt management of complications that may occur in them.
There was no sponsorship in cash or in kind.
We declare no conflict of interests.