De-escalation of empirical antibiotic therapy according to the results of microbiological cultures will effectively target the causative pathogen, besides reducing broad-spectrum antibiotic exposure and minimizing the selection pressure on the development of resistant microorganisms.
Primarily, the study aimed to assess the practice of broad-spectrum antibiotic de-escalation in General Intensive Care Unit (GICU). Secondary objectives were to describe the indications of broad-spectrum antibiotics use, to explore the range of frequently isolated microorganisms in the ICU and to determine the association between different antibiotic agents in the Carbapenem group and their practice of antibiotic de-escalation.
This was a retrospective cross-sectional study performed in GICU Penang General Hospital using antibiotic monitoring sheet from November 2018 to November 2019. Carbapenem or Vancomycin cases were identified. All patients who were given Carbapenem or Vancomycin with results of microbiological cultures were included. Data was analyzed using SPSS version 16.
A total of 382 cases with broad-spectrum antibiotics use were included in this study. Among 250 patients who were on an empirical broad-spectrum antibiotic, de-escalation was successfully done in 241 (96.4%) patients 72 hours after initiation according to microbiological cultures. Nine cases were not de-escalated in view of clinical deterioration of patient's progress. The commonest documented indications for broad-spectrum antibiotics use were pneumonia (46.6%), catheter related blood stream infection (14.9%) and intraabdominal infection (8.9%). The frequently isolated microorganisms included Klebsiella pneumoniae ESBL (15.7%), followed by Methicillin-resistant Staphylococcus aureus (6.0%) and Enterococcus faecium (2.9%). There was no statistically significant association between different antibiotic agents in Carbapenem groups and practice of antibiotic de-escalation upon comparing the trend of de-escalation for Imipenem and Meropenem.
Antibiotic de-escalation has been increasingly recognized in line with combating antibiotic resistance. High antibiotic de-escalation frequency was observed in our study. Of all the 250 cases with broad-spectrum antibiotics which were potentially being de-escalated, more than 90 percent of the empiric cases were successfully de-escalated. This clearly demonstrated that antibiotic de-escalation practice is feasible in critical care setting.
Antibiotic, De-escalation, Broad-spectrum, Intensive care unit
CRE: Carbapenem-Resistant Enterobacteriaceae; ESBL: Extended Spectrum Beta-Lactamase; GICU: General Intensive Care Unit; ICU: Intensive Care Unit; MIC: Minimal Inhibitory Concentration; MRO: Multi-Resistant Microorganism; RCT: Randomized Controlled Trial; VAP: Ventilator-Associated Pneumonia
Septic shock is present in 10% of intensive care unit (ICU) patients with a mortality rate of 60%. Early administration of broad-spectrum, empiric antibiotic reduces mortality and improves outcomes in patients with sepsis and septic shock [1,2]. However, broad-spectrum therapy favors the emergence of drug-resistance and adds excessively to the costs of care [3]. Streamlining or de-escalation of empirical antibiotic therapy according to the results of microbiological cultures and elimination of redundant combination therapy can more effectively target the causative pathogen, resulting in decreased antibiotic exposure and substantial cost savings [4]. The successful use of antibiotics in de-escalation has indicated that such use does not increase the recurrence or mortality rates for sepsis [5]. Several studies have shown that de-escalation therapy leads to reduced antibiotic use, shorter duration of therapy and reduced mortality [6]. Although de-escalation might be safe and feasible in most patients and during most infections, a surprisingly low number of studies have evaluated this strategy. Thus, further information regarding the practice of de-escalation in critically ill patients is clearly needed [7,8].
The study was performed in GICU Penang General Hospital, a 26-bed ICU in a tertiary care hospital in Northern region of Malaysia with case mixed of medical and surgical patients. This was a retrospective cross sectional study. GICU antibiotic monitoring sheet from November 2018 to November 2019 were retrieved and reviewed. Data were collected using data collection form by two investigators. Carbapenem or Vancomycin cases were identified in GICU antibiotic monitoring sheet. Information regarding the indication of antibiotic initiation, empiric or targeted therapy, microbiological cultures isolated, the presence of 72 hours review of empiric antibiotic and decision to continue broad-spectrum antimicrobial after 72 hours review base on microbiological cultures were being documented. Carbapenem or Vancomycin were empirically initiated in hemodynamically unstable patients as per local ICU protocol. Patients who were being initiated with Imipenem, Meropenem or Vancomycin with the results of microbiological cultures from November 2018 to November 2019 were included. Patients who passed away before the results of microbiological cultures were obtained and cases with incomplete or missing results of microbiological cultures were excluded. Data was analyzed using Microsoft excel and Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA), version 16. A descriptive analysis was performed, and the data are expressed as means and standard deviations for the continuous variables and the frequencies and percentages for the categorical variables. Inferential statistics was employed to determine the association between different antibiotic agents in Carbapenem group and de-escalation practice using Chi-squared test or Fisher's exact test for categorical data, and p-value < 0.05 was considered as statistically significant. The study was approved by the National Medical Research Register and Ethic Committee under registration number NMRR-19-1696-48754. An informed consent form was waived by the committee as this was an observational study where data were all retrieved from medical records.
A total of 382 cases with broad-spectrum antibiotics were included in this study where 115 (30.1%) patients were on Vancomycin, 47 (12.3%) patients were on Imipenem and 220 (57.6%) patients on Meropenem. A total of 250 (65.4%) patients were initiated with empiric broad-spectrum antibiotics, and 132 (34.6%) patients were on targeted broad-spectrum antibiotics Table 1.
Table 1: Empiric and targeted broad-spectrum antibiotics use according to antibiotic agents. View Table 1
Among the 250 patients who were on empiric broad-spectrum antibiotics, de-escalation were successfully done in 241 (96.4%) patients after 72 hours as soon as microbiological cultures were obtained. Nine cases were not de-escalated in view of clinical deterioration of patient's progress. Antibiotic were also discontinued for 68 patients among the 250 cases of empiric antibiotics with the microbiological finding of no growth and clinical progress Figure 1.
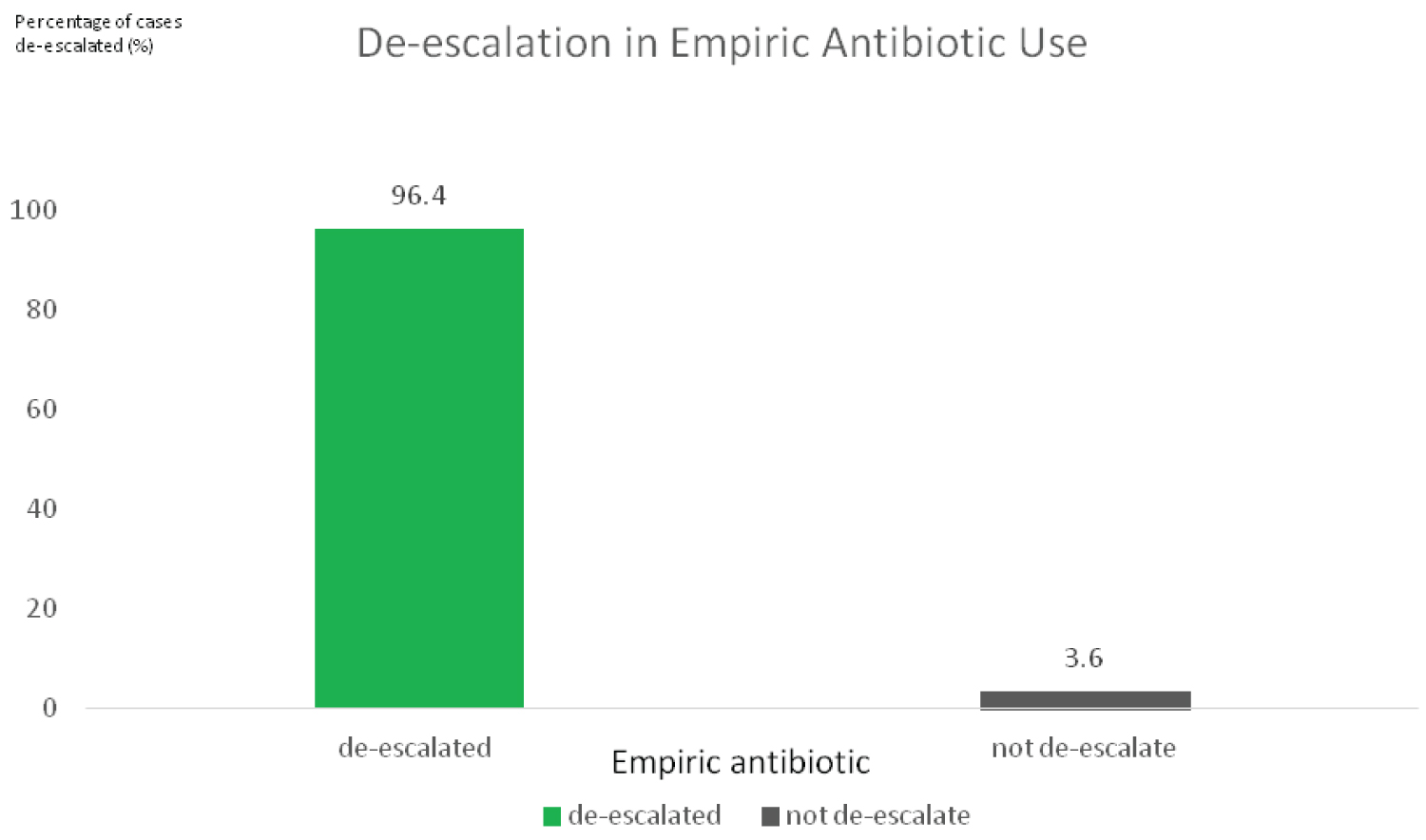 Figure 1: Antibiotic de-escalation practice in empiric antibiotic use.
View Figure 1
Figure 1: Antibiotic de-escalation practice in empiric antibiotic use.
View Figure 1
For Vancomycin, all 74 cases (100%) of the empiric Vancomycin were successfully de-escalated after 72 hours. 61 cases of Vancomycin were discontinued as the results of microbiological cultures showed no growth, with no indication of continuing Vancomycin according to microbiological results and patient's progress. In Imipenem group, 25 (96.15%) cases where being de-escalated from a total of 26 cases. For Meropenem, 142 (94.66%) among 150 cases were successfully de-escalated. 7 cases of Meropenem were discontinued as the results of microbiological cultures showed no growth Figure 2.
 Figure 2: Antibiotic de-escalation practice according to different antibiotic agents.
View Figure 2
Figure 2: Antibiotic de-escalation practice according to different antibiotic agents.
View Figure 2
The frequently isolated microorganisms were Klebsiella pneumoniae ESBL (15.7%), followed by Methicillin-resistant Staphylococcus aureus (6.0%) and Enterococcus faecium (2.9%). Other than the tests which reported as no growth of microorganisms, 33.4% of the total microorganisms cultured were gram negative microorganism and 13.7% were gram positive microorganism. There was no statistically significant association between different antibiotic agents in Carbapenem groups and the practice of antibiotic de-escalation (p > 0.05). The occurrence of antibiotic de-escalation was not related to either Imipenem or Meropenem as empiric broad-spectrum antibiotic. Both empiric cases of Imipenem and Meropenem were de-escalated according to the results of microbiological cultures available.
The commonest documented indications for initiation of broad-spectrum antibiotics were pneumonia (46.6%), catheter related blood stream infection (14.9%) and intraabdominal infection (8.9%) Table 2.
Table 2: Indications of broad-spectrum antibiotics. View Table 2
Adequate empirical antibiotic therapy is crucial for the survival of critically ill patients with severe infection. Moreover, inadequate empirical therapy significantly increases the length of hospitalization in critically ill patients with sepsis or septic shock. With these premises, when microbiological information was pending, the use of broad-spectrum antibiotics constitutes the backbone of the empirical therapy in critically ill patients [9].
Studies found 68% of ICU patients were being administered with broad-spectrum empiric therapy [10]. Antibiotic de-escalation strategy has been recommended to reduce the overall use of broad-spectrum antibiotics. By limiting the prolonged exposure to broad-spectrum antibiotics, this might reduce selection pressure and subsequently prevent the emergence and acquisition of resistant to antibiotic [11].
Published literatures estimated the frequency of antibiotic de-escalation ranged from 10 to 70% [12,13]. Our study found that the de-escalation were successfully done in 96.4% of patients after 72 hours as soon as the microbiological cultures were identified, where the frequency of de-escalation was higher compared with majority of the studies in critically ill population. The frequency of de-escalation observed in this study was higher resulted from established antibiotic stewardship program in the hospital, as antibiotic de-escalation was the key function of this program.
Many factors has been found to affect the de-escalation process, which included inadequate initial antibiotic (10.7%), lack of microbiological documentation (50%), initial appropriate antibiotic therapy that could not be de-escalated which was narrow-spectrum (20.5%), and clinical worsening despite appropriate antibiotic therapy [7]. In this study, 9 cases required the continuation of broad-spectrum antibiotics with the justification of clinical deterioration despite the availability of microbiological culture. The de-escalation process was indeed challenging when taking into consideration of patient's clinical progress.
A retrospective observational study performed in a tertiary hospital acute care center looking at antibiotic de-escalation program found the commonly documented indications for the initiation of broad-spectrum antibiotic were pneumonia (38%), sepsis (27%), and skin and soft tissue infections (11%) [8]. Compared to our study, the commonly documented indications were pneumonia (46.6%), catheter related blood stream infection (14.9%) and intraabdominal infection (8.9%). Our study's finding were almost similar with other studies, where pneumonia was the commonest indication to initiate broad-spectrum antibiotics in critical care setting [14].
Gram negative infections are very common in critical care setting. A study looking at the prevalence of antimicrobial resistance in intensive care unit reported the common microorganisms isolated in ICU population as Klebsiella (90.6%), Acinetobacter (28.1%) and Pseudomonas aeruginosa (21.9%) [15]. Our study reported the frequently isolated microorganisms as Klebsiella pneumoniae ESBL (15.7%), followed by Methicillin-resistant Staphylococcus aureus (6.0%) and Enterococcus faecium (2.9%). According to Malaysian Registry of Intensive Care Report Year 2017, common bacteriological culture in VAP were Acinetobacter spp. (41.4%) including multi-resistant organism (MRO) & non-MRO (41.1%), followed by Pseudomonas aeruginosa (21.4%) and Klebsiella spp. (21.4%) including non ESBL, ESBL, and CRE. For catheter related blood stream infection, common bacteriological culture included Klebsiella spp. (39.4%) including ESBL, CRE and non-MRO, followed by Coagulase negative Staphylococcus (15.2%) and Pseudomonas aeruginosa (12.1%) [16].
As for the 267 Carbapenem cases observed in this study, there were 47 (17.6%) patients on Imipenem and 220 (82.4%) patients on Meropenem, with a higher proportion of Meropenem use. Imipenem was found to be 2 to 4-fold more active than Meropenem against Gram-positive aerobes. On the other hand, Meropenem was 2 to 16-fold more active than Imipenem against Gram-negative aerobes [17,18]. In our study, majority (70.5%) of the infections were gram negative microorganisms, where the infections were mainly gram-negative infections in our study's population. In view of a lower MIC for Meropenem compared with Imipenem in treating gram-negative microorganisms, the use of Meropenem as initial empiric or targeted antibiotic were more common compared with Imipenem, anticipating majority of the infection were caused by gram negative microorganisms in this critically ill population.
The success of antibiotic de-escalation has indicated that such practice does not increase the recurrence of infection and mortality rates in sepsis & septic shock. On the contrary, this practice improved survival rates and length of hospital stay in cases of ventilator-associated pneumonia.
Furthermore, de-escalation has been reported as a safe strategy in patients with sepsis and septic shock admitted to the intensive care unit [5]. In a randomized, prospective trial of 81 intensive care unit (ICU) patients with ventilator-associated pneumonia, the study concluded that patients whose antibiotic regimens were de-escalated were less likely to develop antibiotic-resistant superinfections compared to those whose regimen was not de- escalated (15 vs. 35%, p = 0.017) [19].
A pre and post-test analysis done in SICU Pakistan aimed to determine the clinical and economic impacts of antibiotic stewardship program through prospective-audit and feedback-mechanism changes showed antibiotic defined daily dose of all the antibiotics reduced in the post-antibiotic stewardship period. Ceftriaxone, Cefazolin, Metronidazole, Piperacillin/tazobactam, and Vancomycin showed statistically significant (p < 0.01) reduction. The duration of antibiotics use reduced significantly (p < 0.01). Length of SICU stays, mortality, and readmission reduced in the post-ASP period. Net cost saving was US$ 6360 yearly, mainly through reduced antibiotics consumption, around US$ 18,000 (PKR 2.8 million) yearly [20]. Implementation of antibiotic stewardship program improved the appropriateness of antibiotics prescriptions and optimization of the duration of antibiotics use. This approach was also found to be cost-effective with the reduced cost of antibiotics. A prospective observational study (DIANA study) done in adult ICU patients who received empiric antimicrobial therapy aimed to evaluate how often antimicrobial de-escalation of empirical treatment is performed in the ICU and to estimate the effect of antibiotic de-escalation on clinical cure at day 7 following treatment initiation. The finding of the study showed unadjusted mortality at day 28 was 15.8% in the antimicrobial de-escalation cohort and 19.4% in patients with no change [p = 0.27; RR 0.83 (95% CI 0.60-1.14)]. The IP-weighted relative risk estimated for clinical cure comparing antimicrobial de-escalation with no-antimicrobial de-escalation patients (no change or change other than antimicrobial de-escalation) was 1.37 (95% CI 1.14-1.64). The observational effect estimated on clinical cure suggested no deleterious impact of antimicrobial de-escalation compared to no-antimicrobial de-escalation [21].
A systematic review and meta-analysis included 23 studies was conducted to analyze the de-escalation therapy for a variety of infections. A search of the MEDLINE (via PubMed), EMBASE, and Cochrane Library databases up to July 2015 for relevant studies was performed. The meta-analysis suggested that de-escalation may improve mortality in both community-acquired and ICU-acquired pneumonia. The review concluded no difference was found in mortality for most infections, and some studies favored de-escalation over non-de-escalation for better survival [22].
Another systematic review and meta-analysis with the aim to assess the safety and effects of antimicrobial de-escalation strategy concluded the de-escalation practice was associated with fewer deaths in the unadjusted analysis (OR 0.53, 95% CI 0.39-0.73), 19 studies, moderate heterogeneity. In the adjusted analysis there was no significant difference in mortality (adjusted OR 0.83, 95% CI 0.59-1.16), 11 studies, moderate heterogeneity and the RCTs showed non-significant increased mortality with de-escalation (OR 1.73, 95% 0.97-3.06), three trials, no heterogeneity. There was a significant unadjusted association between de-escalation and survival in bacteraemia/severe sepsis (OR 0.45, 95% CI 0.30-0.67) and ventilator-associated pneumonia (OR 0.49, 95% CI 0.26e0.95), but not with other pneumonia (OR 0.97, 95% CI 0.45-2.12). Only two studies reported on the emergence of resistance with inconsistent findings. Observational studies suggest lower mortality with antibiotic susceptibility testing-based de-escalation for bacteraemia, severe sepsis and ventilator-associated pneumonia that was not demonstrated in RCTs [23]. These studies demonstrated the feasibility of antibiotic de-escalation in critical care setting.
As this was a retrospective study design with small sample size carried out in a single ICU setting, the result might not be statistically powered for generalization. Moreover, the study measured the frequency of antibiotic de-escalation at a center with established antibiotic stewardship program. Hence the finding might not be representative of all institution with ICU population that has not practice the program.
Antibiotic de-escalation has been increasingly recognized in line with combating antibiotic resistance. High antibiotic de-escalation frequency was observed in our study. Of all the 250 cases with broad-spectrum antibiotics which were potentially being de-escalated, more than 90 percent of the empiric cases were successfully de-escalated. This clearly demonstrated that antibiotic de-escalation practice is feasible in critical care setting.
We would like to thank the Director of Health Malaysia for permission to publish this research. We also would like to extend our heartiest appreciation to the head of anesthesiology department & head of the pharmacy of Penang General Hospital involved for the cooperation. Further, we want to acknowledge all the data collectors and staffs in GICU Penang General Hospital.
The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.