Following the gradual easing of the inter-regional travel ban and restrictions on domestic air travels associated with the corona virus pandemic by Government due to economic reasons, confirmed cases of the covid-19 infection across states seems to have shown continual increase and the transmission curve show increasing trend particularly in Nigeria. Awareness of travelers' level of exposure to the spread of the covid-19 disease relative to the travel distances is a sure prerequisite to limit vulnerability and infection, to flatten the curve of transmission of the disease across spatial locations and prevent further spread. The study estimated the exposure of air travelers to the spread of the covid-19 disease, in terms of the concentration of human-covid-19 pathogen carriers they face the risk of interacting with per square kilometer of travels from the airports to-and-fro City centers and suburbs, in various air travel infective pathways in the various states and regions in Nigeria. The proximity model was used to analyze data obtained from secondary sources. It developed a covid-19 exposure risk matrix categorizing the different air travel infective pathways and corridors into extremely high, very high, moderate, low and negligibly low exposure infective pathways. It noted the policy implications of prioritizing the implementation of approved and standard covid-19 preventive guidelines on extremely and very high exposure infective travel pathways and regions; the deployment of greater health facilities, personnel and personal protective equipment (PPE) in high risk pathways was also noted as measures to limit exposure induced vulnerability and to flatten the curve of transmission and prevent further spread.
Proximity, Exposure, Travelers, Spread, Covid-19
The United Nations Environmental Programme [1] views exposure assessment as the measurement of the quantum, magnitude, frequency, and duration of a health hazard relative to human presence and position in the domain and environment of health hazard, disease and/or threatening danger; and depicts a situation of contact with a harmful environment that increases the vulnerability to infection, health injury and death. Thus exposure assessment basically measures the magnitude of the hazard, disease carrying pathogen and/or infective host that poses risk of infection, health injury and/or death to the human population and other populations exposed to it. It equally measures the frequency and duration of human presence in contact with the domain of the infective host. Exposure to hazards according to the UNEP [1] also represent presence of people, livelihoods, species, objects, ecosystem, functions and services, infrastructure, resources, etc, in places and settings in a disease and hazard prevalent environment which leads to vulnerability to infection, health injury, death, etc. Thus, exposure to health hazards or other forms of hazards indicates proximity/nearness to the environment of the health hazard. Dolores and Burt [2] argue that disease infections and the associated health injuries and deaths occur mostly to vulnerable members in a population and that exposure increases vulnerability defined by UNEP [1] as the likelihood, probability, propensity or predisposition to be injured, harmed and/or adversely affected following exposure to health hazards and diseases. From the foregoing, it is deductable that without exposure to hazards, vulnerability will be limited and the associated injuries, damages, deaths, etc as consequences of exposure occurring to vulnerable individuals in the population cannot occur.
The implication is that vulnerability to infectious disease like the covid-19 pandemic, the associated risks of injury, death, etc is dependent on exposure to infective hosts of the covid-19 pathogens among human and non-human populations. Vulnerability will also be influenced by the ability of the exposed individuals, organizations and institutions to take action to limit getting harmed; and while vulnerability is a function of exposure, exposure is a function of the concentration/magnitude of the infective host and proximity to it [3,4].
The Italian citizen index case of covid-19 disease in Nigeria reportedly flew into country via Murtala Mohammed International Airport, (MMIA) Lagos, en-route Ogun state where he was diagnosed positive with the disease in February subsequently transmitted and spread the disease to individuals directly exposed to him as the first infective host of the covid-19 disease in Nigeria [5]. Following continued road, rail and air travel interactions across all states and spatial locations in Nigeria, covid-19 quickly spread with the speed of light to the entire 36 states and regions and the associated work and residential built environments (WRBEs), infecting thousands of citizens. Clearly, an interstate and inter-regional travel interaction was identified as the early fastest channel of direct human to human transmission and spread of the covid-19 infection [6]. This informed the ban on interstate travels by government in all modes, including domestic and international air travels ban and a lock-down policy directive aimed at flattening curve of transmission by limiting exposure to infective hosts of the disease along all infective travel pathways as a preventive measure to further spread of the disease. In view of the economic hardship and hunger caused by compulsory lockdown of cities and ban of interstate travels in all modes of transportation, Government on June 26, 2020 eased the ban on interstate travel and commenced domestic flights while the opening of the airports for commencement of international flights to commenced soon.
The Italian citizen index case of covid-19 disease in Nigeria reportedly flew into country via Murtala Mohammed International Airport, (MMIA) Lagos, en-route Ogun state where he was diagnosed positive with the disease in February subsequently transmitted and spread the disease to individuals directly exposed to him as the first infective host of the covid-19 disease in Nigeria [5]. Following continued road, rail and air travel interactions across all states and spatial locations in Nigeria, covid-19 quickly spread with the speed of light to the entire 36 states and regions and the associated work and residential built environments (WRBEs), infecting thousands of citizens. Clearly, an interstate and inter-regional travel interaction was identified as the early fastest channel of direct human to human transmission and spread of the covid-19 infection [6]. This informed the ban on interstate travels by government in all modes, including domestic and international air travels ban and a lock-down policy directive aimed at flattening curve of transmission by limiting exposure to infective hosts of the disease along all infective travel pathways as a preventive measure to further spread of the disease. In view of the economic hardship and hunger caused by compulsory lockdown of cities and ban of interstate travels in all modes of transportation, Government on June 26, 2020 eased the ban on interstate travel and commenced domestic flights while the opening of the airports for commencement of international flights to commenced soon.
Since the current government decision to open the airports for commencement of domestic flight in the face of increasing transmission and infection rates is motivated by economic considerations rather than safety and health considerations; the need to provide empirical information on the levels of exposure to spread of covid-19 disease along identified air travel pathways, as safety guide for air travelers, airport authorities, users and other stakeholders. That is the motivation for this study. Understanding the likely concentration of human-infective covid-19 pathogen carrier per square kilometer of travel from city suburbs to-and-fro airports to which travelers are exposure in the use of identified travel pathways will necessitate informed safe behavior aimed at limiting vulnerability of travelers to infections in Nigeria.
In the study, we used about 26 airports in located in Abuja, Lagos, Enugu, Kano, Calabar, Port-Harcourt, Kaduna, bauchi, Maiduguri, Sokoto, Jos, Yola, Kebbi, Asaba, Owerri, Gombe, Minna, Uyo, Katsina, Makurdi, Ibadan, Jalingo, Akure, Benin and Ilorin; in different states and regions of Nigeria, from which travelers currently access domestic flights. These different states currently have varied confirmed covid-19 cases based on empirical evidence from the NCDC [5]. The implication is that given the proximity of the airports to the city centers and suburbs, air travelers in Nigeria will certainly experience disproportionate rates of exposure to covid-19, which equally implies disproportionate degrees of vulnerability to covid-19, as they access air transport services in various airports in different airports in Nigeria. It is believed that once travelers are able to understand the level of exposure risk they face on travel pathways and take serious steps as provided in the covid-19 prevention guidelines by the WHO [6] to limit their individual vulnerability; the curve of transmission and spread of the covid-19 disease will be flattened and the disease prevented from spreading further as airlines and airports prepare to commence full flight operations in the coming weeks. In the study therefore, the major infective air travel pathways in individual airports in Nigeria will be identified and the risk of exposure to the spread of covid-19 posed by each identified air travel pathway estimated based on proximity metrics. Disproportionate exposure and vulnerability to the covid-19 pandemic determined will be used to develop a risk matrix and group the states and regions into low and high exposure risk zones for serious and proactive implementation of vulnerability limiting/reduction strategies and safety guidelines for air travels in the different airports locations in Nigeria.
The work of Jose, Willem, Piet, Jean-Marie, Jamshid and Pol [7] was able to establish the use of Gravity Model like the proximity model to estimate the spatial spread and exposure of vector-borne diseases. The proximity models and gravity models depict spatial interaction models formulated in line to Newton's laws of motion which expresses attractive force (interactive force) forces between two charges apart as the been directly proportional to the product of the charges and inversely proportional to the square of their distance apart. Economist and epidemiologists over the years developed variants of the model for estimating trade flows and exposure to spread of epidemics and diseases between two regions separated by space, based on their interactions with each other. For epidemiologists, the spatial spread to an infectious disease is dependent on the magnitude/concentration of the disease and the proximity/nearness to the source of infection. Thus exposure to the source of infection and epidemic is dependent on the proximity (distance) of individuals and spatial locations to the sources and the concentration/magnitude.
By implication, spatial interactions between non infected settlements (spatial locations) and infected settlements exposes the initial to the epidemic. The proximity model for estimation of spatial exposure to infectious diseases based on interaction between settlements views that the likelihood of exposure to infectious disease between two interacting locations as dependent on its proximity to the domain of the infective host. This suggests that proximity is a determinant factor of exposure to sources of disease infection. The farther a location is from the source of infection, the less exposed it is to the disease and the less vulnerable the individual populations in the settlement are to injuries, death and damage risks associated with infection.
Transport and communication increase spatial interaction and causing the death of distance. Depending therefore on the concentrations and magnitudes of a given disease/epidemic type in the interacting regions and the intensity of interaction, a low risk region may be greatly exposed to the source of the infection and widely infected [7]. This underscores the importance of determining exposure levels between interacting spatial locations so that health and safety facilities and vulnerability limiting measures can be established in line with the levels of exposure to the disease.
This is even more important in the fight against the spread of the covid-19 pandemic as the aviation sector and interstate air and road travels surge in the coming weeks and months following the easing of the lock-down. The situation in the Country today indicates that almost all the airport cities, states and urban and regional settlements are already physical habitats and host of the covid-19 pathogens with humans being the vectors. The product of the disproportionate concentrations of confirmed cases in the various airport cities and work and residential built environments in states relative to the of the distance between any two such interacting travel originating and destination Cities provides information on the level of exposure to covid-19 disease faced by travelers [8].
Maantay, Chakraborty and Brender [9] notes the adverse health outcome effects of exposure to environmental health hazards. According Maantay, Chakraborty and Brender [9], disproportionate impacts of environmental health hazards, diseases and infection is consequent from disproportionate exposure to such environmental health hazards. It implies that spatial locations that are less exposed to sources of environmental health hazards experience less impact and effects. In the case of covid-19, such locations will have fewer infections, injuries to health and death associated with the disease. Maantay, Chakraborty and Brender [9] also support the assertion that maintaining far distances from disease vectors, spatial host, and sources of infection is the proper best practices of avoiding and/or limiting exposure to environmental health hazards. This opinion invariably support the assertion that extent of proximity to sources of health hazards is a measure of exposure. This motivation for the adoption of the social distancing rules and the ban on air travels across regional blocks and residential and work settlements is definitely aimed at limiting spatial interaction, eliminating proximity and limiting exposure to the covid-19 pandemic. Now, following the resumption of domestic flight operations and lifting of ban on interstate as a result of the economic crunch associated with the lockdown measures, travel interaction will make distant locations more proximate and this will cause Cities, sub-urban centers, work and residential locations to be more exposed to and vulnerable to the covid-19 pandemic [9,10].
Studies by Hess, Bachler, Momin and Sexton [11] underscores the need for robust exposure assessment in future analysis of environmental health hazards and disease in order that cautiousness may be adopted in determining and maintaining appropriate level of distances from hazard sources to avoid exposure, infection and harm to vulnerable groups and individuals. According to Hess, Bachler, Momin and Sexton [11], adverse health effects have been made limited by distance-based exposure surrogates. Distance-based exposure metrics thus reflect in variations in vulnerability following the associated distance and duration induced disproportionate exposure. Oliveira, Orrillo, Gamboa [12] notes the importance of accommodation of the home-office (working at home) in a simple model of endogenous growth as a resultant effect of mobility restrictions aimed at lessening workers exposure and vulnerability to covid-19 infection. According to Oliveira, Orrillo, Gamboa [12] due to the strong mobility restrictions imposed on citizens during the COVID-19 pandemic, individuals were made to work in home offices located home in the belief that the long-run effect of working from home offices will eliminate the spread of the disease by flattening exposure to already infected work zones and individuals. Chakraborty, Maantay, and Brenden [13] and Haung and Batterman [14] also provided a documentary overview of methods and models in use in assessing exposure to environmental health hazards for purposes of ensuring environmental justices and safety; and notes the existence of an underlying relationship between proximity to environmental health hazards and potential exposure to adverse health effects. Leslie, Patrick, David, Mark, Jonathan and Kevin [15] in a study observes the rapid spread of severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) that results in corona virus disease 2019 (COVID-19), in corporate entities, federal, state, county, and city governments, universities, school districts, places of worship, prisons, health care facilities, assisted living organizations, daycares, homeowners, and other building owners and occupants. The study notes the importance of the need to reduce the potential for transmission through built environment (BE)-mediated pathways since the isolation of the revealed common pathogen exchange pathways and mechanisms may serve in curtailing the spread of the pandemic. Person-to-person (direct transmission) and object-to-person (indirect transmission) have been identified as the commonest covid-19 pathogen pathways and exchange mechanism in workplaces and residential settlements; implying that limiting human exposure to these pathways flattens exposure and curtails the spread of the disease. The roles of the built environment in curtailing the spread and transmission of the covid-19 pandemic thus entails the development of actionable and achievable guidelines aimed at limiting exposure and vulnerability through the revealed pathways [15,16].
In this study, we aimed at bridging the gap in literature by estimating and providing empirical evidences on the risk of travelers exposure to the pandemic on each revealed interaction pathways between the vulnerable zones in Nigeria as domestic flight operations and interstate road movement commences; and to also provide information on potential disproportionate infection on the pathways as basis for covid-19 prevention and management decisions. Pathways and/or zones with higher risks of exposure will demand a higher level of implementation of covid-19 pandemic preventive and management measures.
Data used for the research were obtained from secondary sources. Data on the confirmed cases of covid-19 in the 26 various airport Cities and regions including Abuja and Lagos were sourced from the Nigerian center for Disease control [17]. The distance between each airport and the urban and suburban centers were obtained from the urban planning Department of the Ministries of Land, Housing and Urban Development in various states. This City center was chosen as the datum for measuring the distances to the airports because for purposes of urban planning, the city center represents the centroid of all geospatial distances to the city suburbs. Like most disease and epidemic exposure models, we assumed that the infected population (covid-19 pathogen carriers) in each domain remained carriers cannot be cured in the short-run [18]. Though most of the confirmed cases are usually isolated from the asymptomatic population, the study assumed that where the first carrier in a domain is identified and isolated; at least one individual among the asymptomatic population that in that domain may have been infected with the disease before the isolation. Asymptomatic does not guarantee the total absence of infected pathogen-host but an indication that symptoms have not yet developed [5]. This assumption is validated by the continuous daily increase in trend of confirmed covid-19 cases even with the isolation of confirmed cases in almost all the study areas identified [17]. Given the fact that the NCDC does not provide information on the exact residential and work location, Local Government Area and/or Community/suburb of the confirmed covid-19 pathogen carriers, the study assumed all suburbs of the city to have equal concentrations of the disease while the City centers; having the greatest population of human interaction, host the highest concentration of the confirmed cases such that as the city center is approached from the suburbs and airports, the risk of exposure increases. This assumption validly helped us to overcome the challenge posed by unavailability of information on the exact locations within the urban areas that host the greatest of covid-19 pathogen carriers and enables the overcoming of the fear posed by the lack of that information among the population. Using the statistics on confirmed cases of covid-19 in each airport city and the distance of each airport to the urban center as covid-19 hotspots; we used the proximity model to estimated the risk of exposure of air travelers to the spread of covid-19 in Nigeria in terms of the concentration of human-infective covid-19 pathogen carriers per square kilometer traveled from the airports to-and-fro urban cum sub-urban centers (Appendix).
The proximity model like the gravity model of spatial interaction between regions provided evidence for data requirement for assessing air travelers' exposure to the spread of the covid-19 pandemic based on physical interactions of air travelers between specific airports terminals to-and-fro urban centers and suburbs. With direct human-to-human transmission being the most common transmission mode of the novel covid-19 disease; and NCDC statistics does not provide information on the exact domain/location of the confirmed pathogen carriers but aggregates it for each City/state; the City centers and suburbs are taken as the covid-19 hotspots.
Like the proximity model, the gravity model developed by Isaac Newton in the study of electric flux; underscored the role of distance (proximity) between spatial locations as important requirements determining the exposure to the risk of transmission of the disease [2,11]. Thus exposure as a measure of the quantity/concentration of infective-pathogen-carriers a sample of healthy population is faced to interact with in and per unit of environment is influenced by distance between the pathogen-host domain and the reference healthy environment. The gravity model of spatial interaction between two trading regions for example proposed that the trade flow is proportional to the product of the economic sizes measured by the gross domestic product (GDP) and inversely proportional to the square of their distances apart [19] i.e.:
Where:
Fij = Spatial interaction induced trade flow from origin location (i) to destination (j)
G = Constant term, Mi = GDP represent economic size of origin location (i)
Mj = GDP representing economic size of destination location (j).
Dij = Distance between the two airport locations.
The above model clearly evidences the influence of distance/proximity in the flow and spread of trade and other environmental factors. Thus, the nearer (more proximate) two spatial locations are to each other, the greater/bigger the flow between them, and vice versa.
According to Baie and Bergstrand [20], for econometric applications, it is traditional to specify that:
Where: μij = error term.
Where β0 = constant term, β1, β2, β3 = coefficient of terms.
Traditional General linear Model (GLM) estimation involves taking natural log of both sides as shown:
The gravity model concept is viewed to be associated to the concept of entropy maximization since it involves interaction flows between spatial entities [21,22]. Thus it has being in application in modeling trade flows, transportation network, exposure to pollutants and spread of diseases, spread of environmental health hazards between spatial locations [19,23-26].
Xinhai, Huidong, Dejian and Zhibin [18] developed a modified version of the model for measuring the spread and transmission of epidemic diseases based on interaction between spatial locations such that:
Spatial communities:
Where; DISPREADij = disease spread/flow between communities in the spatial locations, Pi = population size of pathogen vector originating and or infecting community, Pj = population size of destination vulnerable community, Dij = distance between the two spatial locations. Where both interacting locations already have infective hosts, the aggregate forms the basis for the spread of the disease. Similarly, the above equation is estimated by linear representation as shown:
Though Santos and Tenreyro [27] argues that the above approach of estimating the log-linear equation by GLM can lead to biases especially where flow and/or interaction value between any two regions is equal to zero such that the DISPREADij becomes zero. They suggested an estimation of the model in its multiplicative form. However, Santos, et al. (2006) did not explain where the source of their result. Martin and Pham [28] argues that using PPML on gravity severely biases estimates when zero flows are frequent.
Hess, Bachler, Momin and Sexton [11] developed a proximity model based on the inverse relation between concentration of hazards and/or infectious diseases in an environment and square of the distance between the host sources of the pathogen and the healthy population of interest as a measure of the exposure of the healthy population to the infective pathways. Hess, Bachler, Momin and Sexton [11] proposed that population exposure to infection/hazards based on proximity to the domain of the infective host is calculated as:
Where: Qi = Concentration and/or quantity the pathogen/hazard (infective host) in the originating infective domain (i).
Dij = distance apart of the infective host domain and the healthy population facing the risk of exposure.
EXPOSUREj = the exposure of the healthy population to the spread of the disease.
n = number of infective host domains or spatial locations constituting infective hosts of the disease.
We modified the above expression to capture the exposure to the spread of covid-19 pandemic and other environmental health hazards faced by a single health population domain (j) in a scenario where more than one spatial location constitute the infective community (multiple infective locations); i.e.: i is more than 1 (i > 1); the exposure to the transmission and spread of the disease is the summation of the exposures from each contributing infective community. For example, where a traveler faces exposure to 4 infective domains/regions as a result of physical interaction with the four different infective spatial locations having varied concentration of the infective pathogen, have i = 4; 4 > 1. The risk of exposure to the spread of the disease is summed as the aggregate of individual exposures faced in each infective domain. We write that:
We used equation - (6) to determine the exposures faced by air travelers between the travel pathways from the airports to-and-from the City centers and suburbs.
Similarly, equation - (7) was used to aggregate the total risk of exposure to the spread of the covid-19 pandemic following the physical interaction of travelers in multiple interstate travel pathways. For example, multiple travel interactions in Lagos (Murtala Murhammed International Airport (MMIA) and/or Abuja (NNamdi Azikiwe International Airport NAIA) airports as major domestic flight routes to other regional locations in Nigeria, exposes the traveler to the aggregate of the exposures faced in Lagos and/or Abuja and the new destination location in which the traveler also accesses the urban center or suburbs of the destination city. We estimated traveler's exposure to the spread of covid-19 disease based on interactions first in both Abuja and Lagos as origin and destination routes using - (7) as shown below:
Where: = of exposure to covid-19 faced in spatial interaction from Abuja to Lagos.
The travel pathways are decomposed for clarity as follows:
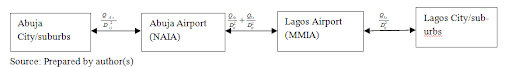
As aforementioned, we used - - (6) to determine air travelers exposure to the spread of covid-19 in air travel pathways airports to-and-and-fro urban centers and suburbs in each state and used - (7) and (8) to determined the air travelers exposure to the spread of covid-19 pandemic for travels interactions in multiple Cities following interstate travels.
The result shows a national average per travelers' exposure to the spread of covid-19 infection of 17.2 human-infective-carriers per square kilometer of travel from airports to-and-fro City centers and suburbs. By implication, the more kilometers traveled to-and-from airport terminals and city centers and suburbs, the greater the exposure to the spread to the pandemic and subsequently the vulnerability to actual covid-19 infection. The coefficients of exposure to the pandemic in the individual airports used in the study indicate a disproportionate traveler's exposure to the spread of the disease in the different airports in the regions. For example, Kano, Yola, Benin-city, show extremely high exposure rates of 119.6, 100, and 97 human-infective-carriers per square kilometers based on the proximity of the each airport infrastructure to the city center and suburbs as covid-19 hotspots. Delta (Asaba), Oyo (Ibadan and Lagos have respective very high exposure risks of 25, 24.45, and 19.7 human-infective-carriers per square kilometer of travel interaction from the airports to-and-fro the city centers and suburbs. Katsina, Enugu, Borno (Maiduguri), Kwara (Ilorin), Ondo (Akure), and Rivers (Port-Harcourt) have high exposure rates of 9.85, 5.16, 5.10, 3.76, 2.80 and 2.02 human-infective-hosts per square kilometer from the airport terminal to-and-fro the urban centers and suburbs respectively. While Makurdi (Benue), Abuja, Minna (Niger), Kaduna, and Bauchi have moderate exposures to spread of covid-19 rates of 1.61, 1.51, 1.25, 1.18, and 1.07 human-infective-hosts per square kilometer respectively; Sokoto, Owerri (Imo), Gombe and Jos (Plateau) show respective low exposure risks of 0.65, 0.61, 0.59 and 0.59 infective-carriers per square kilometer from the airport terminal to-and-fro the city centers and suburbs. The Cities of Calabar (Cross River), Jalingo (Taraba), Uyo (Akwa-Ibom), and Bini Kebbi (Kebbi) show respective negligible low exposure rates of 0.26, 0.17, 0.15, and 0.13 infective-carriers per square kilometer travelled from the airports (Table 1).
Table 1: Air passengers Risk of Exposure to spread of covid-19 disease on infective pathways between airports and WRBE in states. View Table 1
The policy implication is that health workers and covid-19 taskforce committees should prioritize preventive attention on the extremely high, very high and moderately high exposure regions. This is because vulnerability to actual covid-19 infection will be greatest in these regions as increase in rate of spatial interactions between states following the easing of the ban on interstate travels may worsen the risk of transmission across states and regions. More covid-19 preventive kits and personal protective equipment, health facilities and infrastructures, etc is equally needed in far greater quantities to manage and control the spread of the pandemic in high risk zones than in negligible low risk zones. The implication of the proximity approach to individual air travelers and airport users is that the exposure to the spread to covid-19 infection as they interact with each airport city increases as the city center and suburbs is accessed farther from the airport. Since there is disproportionate exposure between the regions, travelers should limit their exposure to the spread of the covid-19 disease by limiting their physical interactions with the work and residential built environments (WRBE) in the city centers and suburbs, particularly for extremely and very high exposure zones which host the greatest numbers of human-infective covid-19 pathogen carriers. For urban planners and transport infrastructure developers, it is important to note the influence of proximity on exposure to health hazards. For example, the Yola airport in Adamawa state and the Kano are the most proximate airports to the city centers, thus they show associated higher exposure rates to the spread of covid-19 disease than Lagos and Abuja with highest numbers of confirmed covid-19 cases. This increases vulnerability to infection to both the individuals in the city and travelers using the infrastructure. It is important to also note that travel interaction in of individuals in multiple exposure regions increases their exposure as the sum of the regional exposures faced by the travelers in each of the regions traveled. For example, see Figure 2 for multiple travel interactions starting from Lagos to other airport locations and regions in Nigeria.
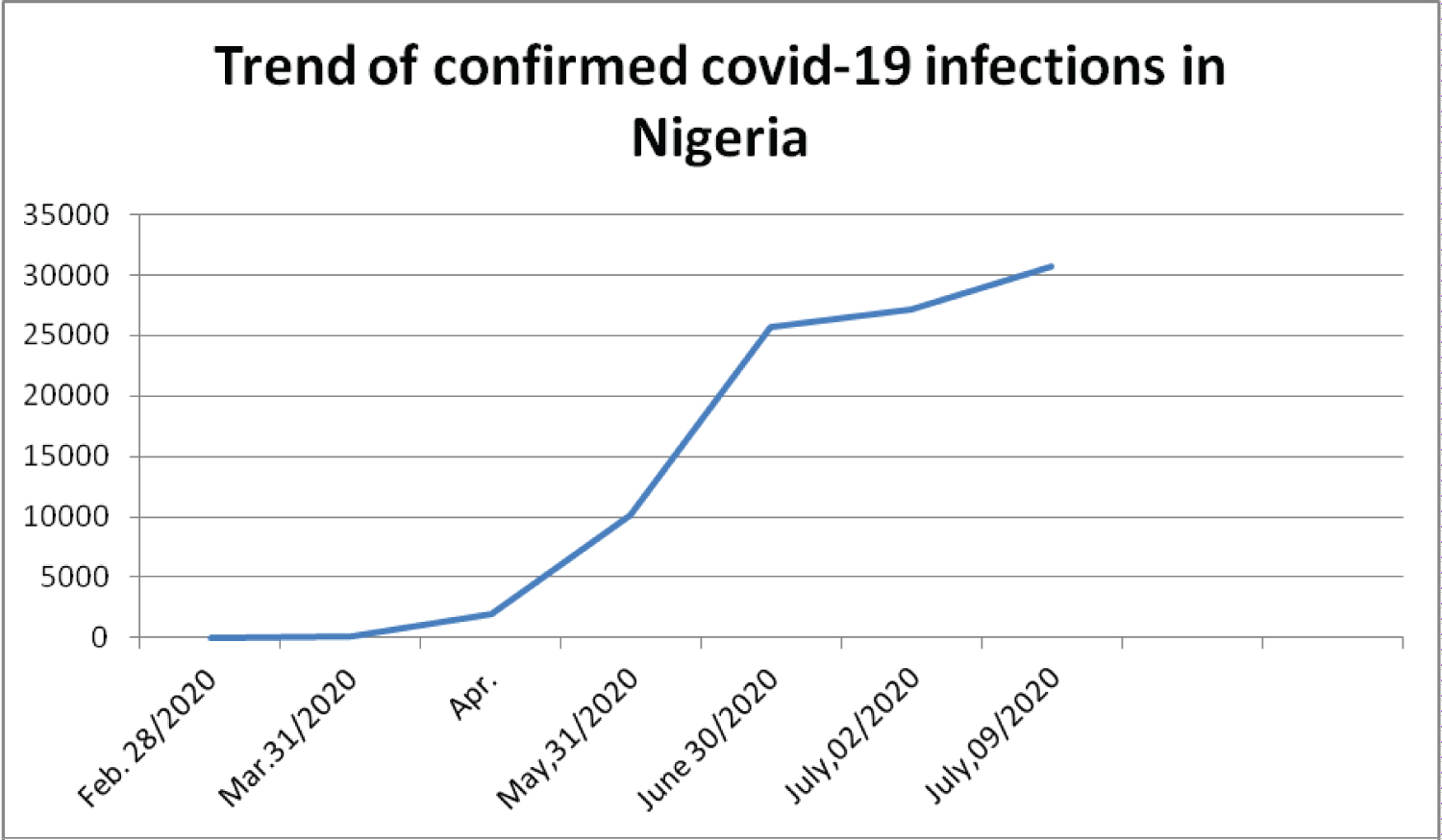 Figure 1: Trend of confirmed Covid-19 infections in Nigeria.
View Figure 1
Figure 1: Trend of confirmed Covid-19 infections in Nigeria.
View Figure 1
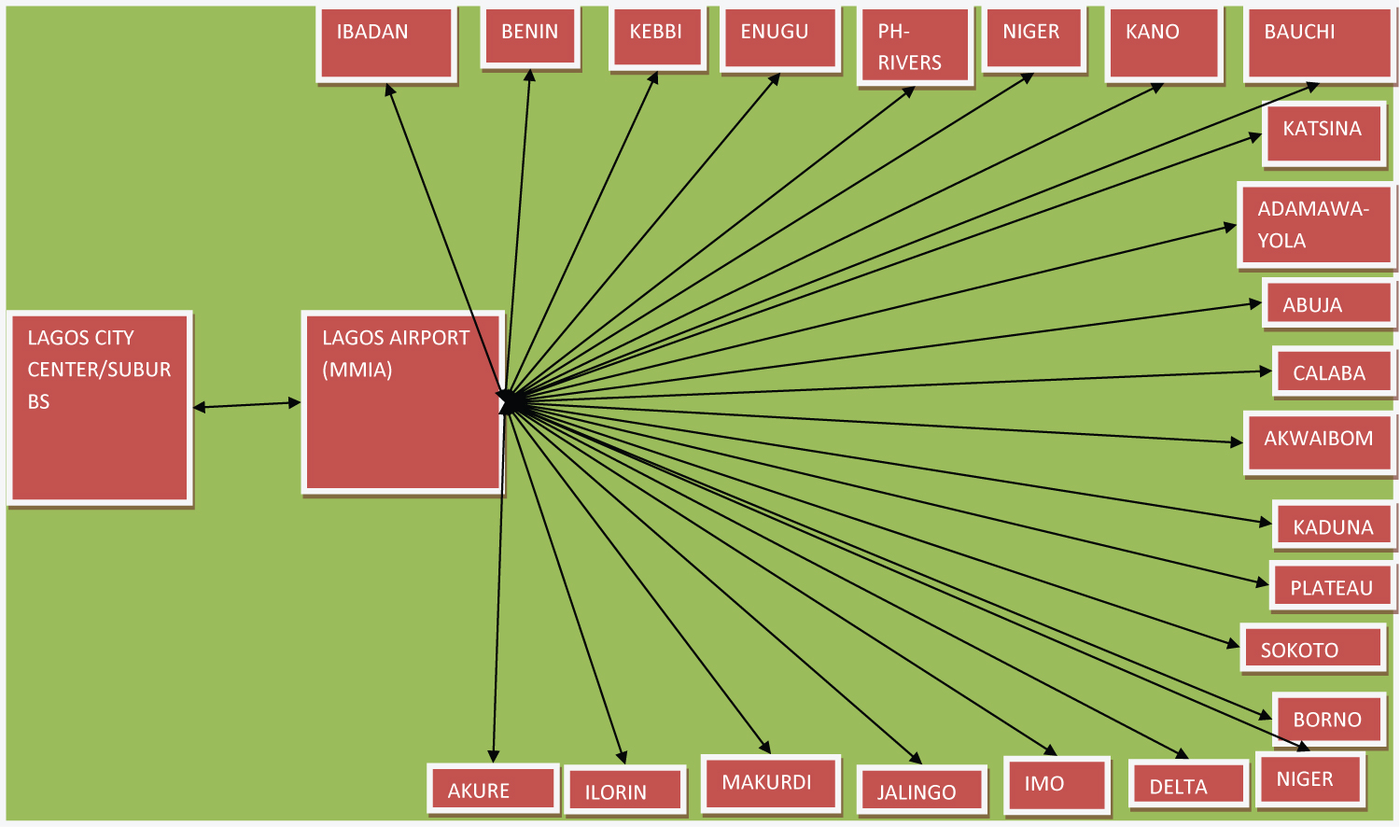 Figure 2: Air travelers exposure to Covid-19 based on inter-state spatial interactions between Lagos and Major airport Cities in Nigeria.
View Figure 2
Figure 2: Air travelers exposure to Covid-19 based on inter-state spatial interactions between Lagos and Major airport Cities in Nigeria.
View Figure 2
The identified travel infective pathways between Lagos and other states in various regions is best used to explained the aggregation of exposure risks as individual travelers interact between spatial locations by physically transiting through them. For example, by a physical travel interaction from Lagos to Abuja, a traveler accumulates an aggregate exposure to the spread of covid-19 pandemic equivalent to the sum of the exposure risk faced in each of his travel from Lagos urban center and/or suburbs to Lagos airport and travels from Abuja urban center and/or suburbs to Abuja airport as indicated in the Figure 2. See Table 2 for individual travelers' exposure to the spread of covid-19 as a result of travels interactions in both Lagos and other regional airport locations as well as travels interactions in Abuja and other regional airport locations.
Table 2: Travelers' exposure to spread of covid-19 following travel interactions on travel Pathways in Lagos and Abuja to-and-fro other airport Cities in Nigeria. View Table 2
The travel interactions in both Lagos and Kano, Lagos and Yola, and Lagos and Benin infective travel pathways holds extremely high exposure to the spread of the covid-19 pandemic above 100 infective hosts per square kilometer traveled into WRBE of the cities/states. This is flowed respectively by very high exposure to spread of covid-19 by travel interaction in Lagos and Asaba (Delta) and Lagos and Ibadan of 45.48 and 44.45 infective hosts per square kilometer of journey into the city centers. Travel interaction in Lagos and other states/cities show exposure rates below 30 individual hosts per square kilometer. Similarly, travels between Abuja and Kano, Abuja and Yola and Benin and Abuja infective pathways show highest exposure of travels to the spread of the covid-19 pandemic than other regions. However, individual air travelers and airport users faces lesser risk of exposure to spread of covid-19 and the infection when the travel is among Abuja and the associated air travel infective pathways in other airport regions; Appendix 1 than Lagos and the associated infective-air-travel pathways to other regional airport locations. The policy implication is that limiting the exposures to extremely high exposure infective pathways will limit travelers' vulnerability to covid-19 infection while unguarded increase to travels through such high exposure travel pathways will increase vulnerability to covid-19 infection and further increase the spread of the disease. Thus awareness of travelers' levels of exposure to the spread of the covid-19 pandemic is a prerequisite to flattening the curve of transmission of the disease thereby stopping further spread. When it becomes obvious that travelers must travel through high and extremely high exposure pathways, they must adopt safe practices and serious measures to limit their vulnerability. This may be by strictly adhering the general standards and procedures and preventive guidelines issued by the World Health Organization (WHO) and Nigeria Centers for Disease Control (NCDC). Airport authorities and airlines operating in extremely and very high exposure pathways as well as health workers should be aware of their exposure levels so as to be able to develop effective personal and organizational mechanisms to prevent further spread.
Travelers in the different air travel pathways in the different states and regions show disproportionate exposure to the spread of the covid-19 pandemic. Increasing travel interaction of individuals in multiple states and pathways following the lifting of the ban on interstate travel and the commencement of interstate domestic flight operations has equally increased the exposures faced by travelers to the spread of the covid-19 disease. The exposure to spread of covid-19 travels pathways from Lagos to-and-from the associated airport cities imposes the highest of exposure risks than those associated with to-and-fro Abuja and other airport locations. The disproportionate exposure matrix in the states and regions is shown in the Figure 3.
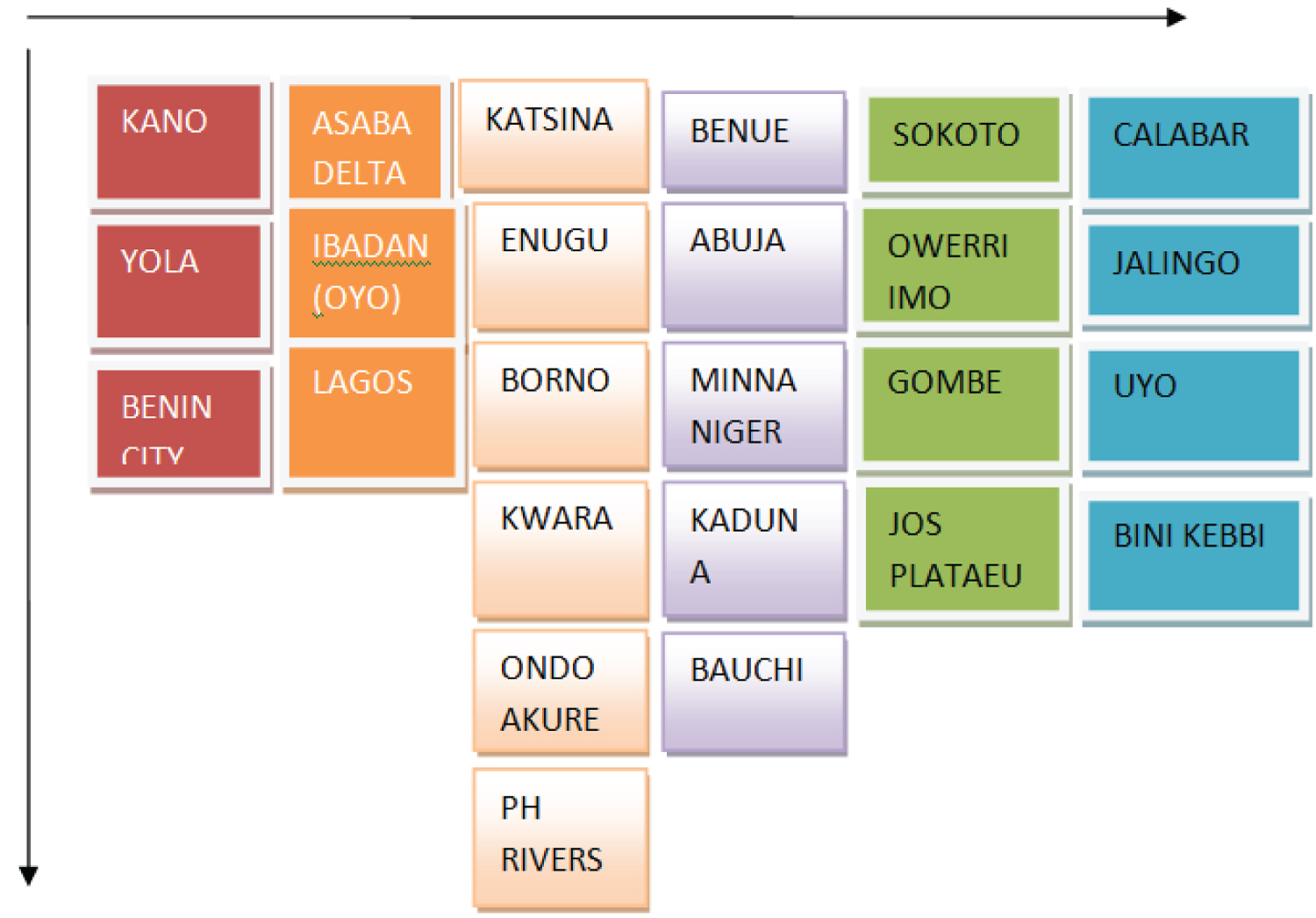 Figure 3: Decreasing order of exposure to spread of covid-19 in states.
View Figure 3
Figure 3: Decreasing order of exposure to spread of covid-19 in states.
View Figure 3