Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) has first emerged in the province of Hubei, China, in late December 2019, and the contagious form of disease covered the whole world by the rapid spread. As of July 12, 2020, there are 12,879,107 confirmed cases of Coronavirus disease (COVID-19), and 5,68,422 deaths were reported globally [1]. However, after its first appearance in China, the United States of America (USA) and Europe were worst hit by COVID-19 and emerged as the epic centre of disease. Contact transmission, the severity of the disease, and unavailability of specific therapeutics make COVID-19 more deadly than previous other viral outbreaks and it seems to be the disease of the century [2]. SARS-CoV-2 transmission occurs via the respiratory droplets produced during coughing, sneezing, and talking [3]. The nuclei of the droplets contain viral particles that can remain viable in aerosols for up to 3 hrs and can infect the individual if inhaled or indirectly via the touch of contaminated objects [4,5]. Although, health-care authorities and vaccine industries are searching for specific and effective therapies to prevent community transmission of SARS-CoV-2, to date any specific measures are unavailable. Apart from western medicine policymakers and the scientific world are also looking for alternative medicine and some-how they have shown some level of protection in China and India. In such a health emergency when the entire world is suffering from SARS-CoV-2, a vaccine is the only hope, and according to world health organization (WHO), 110 vaccine candidates are under development and approx. 10 vaccine candidates are part of the human trials.
The scientific community is also discussing the possibility of herd immunity, the term coined almost a century ago [6], this term was rarely used until recent decades and its usage is encouraged by the increasing use of vaccines. Although, the term "herd immunity" has spread almost as wild as the virus from the start of the coronavirus pandemic, trying to reach herd immunity without a vaccine would be a disastrous pandemic response strategy. To achieve the herd immunity, acquired immunity is reputable at the level of the individual and it can be possible either by natural infection with a virus or with a specific vaccine. However, at present vaccine is not available and lockdown is the only way to contain the disease. Though the concept of herd immunity looks disastrous in the absence of a vaccine, natural herd effect cannot be overlooked and theoretically herd effect through natural infection is possible. At present various nations are going to lift lockdowns and that poses some serious risk of a potential second peak in cases of COVID-19, and now it is one of the hottest topics of scientific debate at present. The major question is can exposure to the coronaviruses that cause the common cold help to protect against COVID-19 and is herd immunity plausibility and hope in modern-day or terrible thought to save a life in modern-day. Therefore, in this communication, we attempted to throw some light on the concept of herd Immunity amid COVID-19 crisis.
The term `herd immunity' is a very old term and it is a benchmark that is achieved when the majority of the population develops resistance to a highly contagious disease, which, in turn, limits the spread of the disease further. It is frequently seen in recent literature on the epidemiology of infectious diseases and their prevention and control by immunization [7]. Herd immunity imparts resistance to a group against the infectious disease because of the immunity of a large proportion of the members in the group and leads to consequent lessening of the likelihood of an affected individual coming into contact with a susceptible individual although it is not necessary to immunize every person to stop transmission of an infectious agent through a population [8]. Simply, the herd immunity threshold depends on a single parameter recognized as R0, or the basic reproduction number, where R0 denotes to the average number of secondary infections caused by a single infectious individual introduced into a completely susceptible population [9]. Theoretically, if an infectious pathogen with an R0 of 4, means that the infected individual can infect 4 others during the infectious period if the population is not immune against the pathogen. Statistically, the herd immunity threshold is defined by 1 - 1/R0 e.g. if R0 = 4, the corresponding herd immunity threshold is 0.75 [9]. In a particular population, R0 is defined by the host and pathogen interaction and it might be different for various pathogens. R0 may depend on the characteristics and transmission dynamics of the people facing the disease outbreak [10]. Herd immunity works in a way like, if the approx. 70% of the population has become immune to the virus, then four out of every five people who encounter someone with the disease, won't contract it. Hence, they will not be able to spread it, and this will help in controlling the transmission of that particular disease (Figure 1). This is an indirect way of protecting those who are not immune to the disease. Depending on how infectious a disease is, about 70 to 90% of the population needs to develop resistance against disease to achieve herd immunity [11].
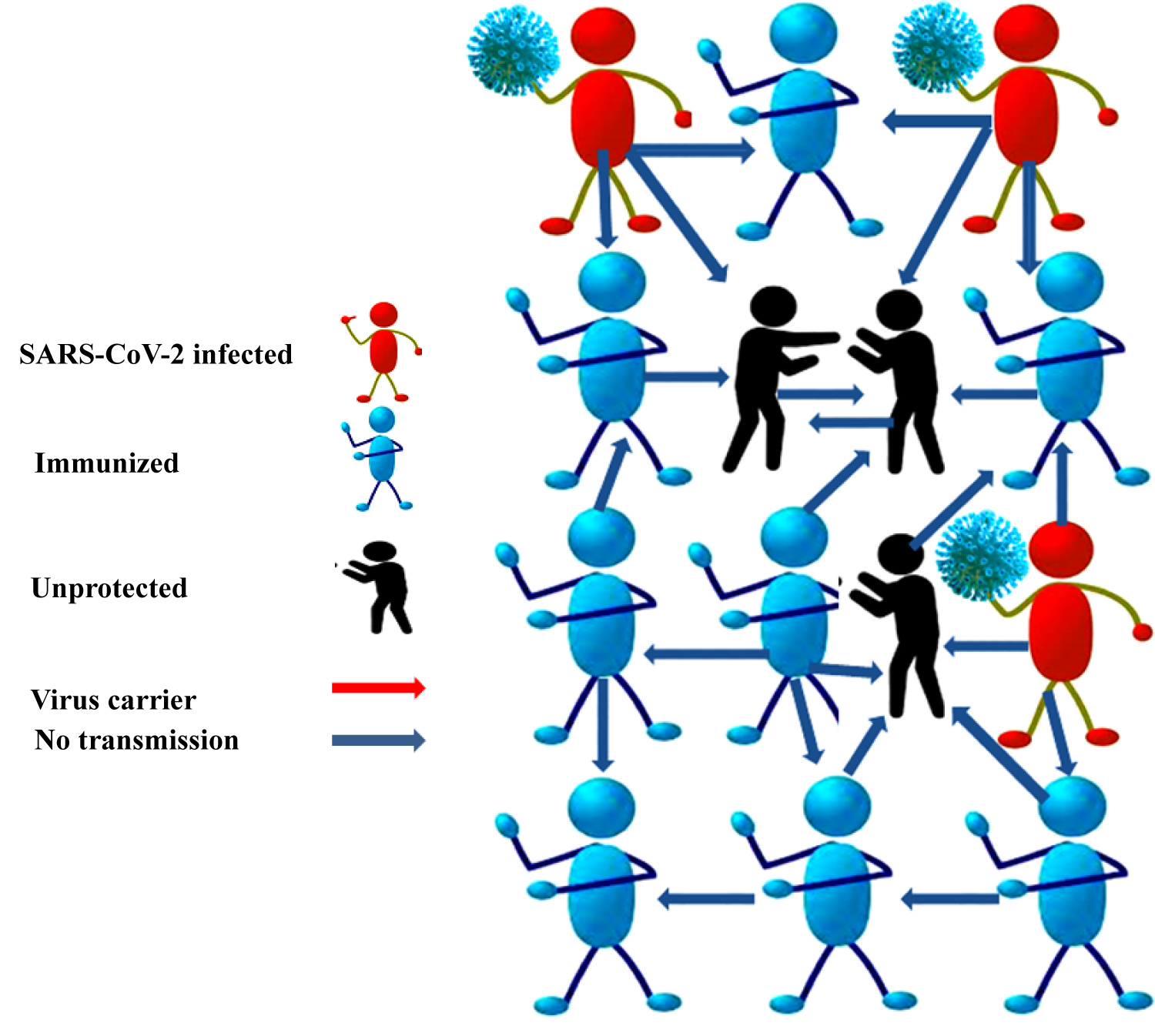 Figure 1: Plausibility of Herd immunity for the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to contain the pandemic.
View Figure 1
Figure 1: Plausibility of Herd immunity for the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to contain the pandemic.
View Figure 1
Herd immunity is a naturally occurring body phenomenon recognized in the 1930s and it was observed when a significant number of children had become immune to measles [12]. There are various examples of herd immunity available so far explaining the importance of indirect protection for predicting the short- and long-term impact of vaccination programs. Such as measles, mumps, rubella, pertussis, chickenpox, and polio [13,14]. Apart from these, herd immunity has been shown in the past against Pneumococcal and Haemophilus infections after the introduction of conjugate vaccines [15]. The examples and historical findings available support herd immunity and again herd immunity emerged as the hottest topic of scientific discussion in the 21st century amidst SARS-CoV-2 outbreak. The challenge in the case of COVID-19 in terms of the herd immunity is how it will be effective in reducing infection among those who remain susceptible to the population. Because at present no vaccine is available that can show the direct effect on the transmission that is the key for the indirect effect or herd immunity.
There are two possible ways to gain immunity against the SARS-CoV-2 infection i.e. either by direct immunization which needs a specific vaccine and second is indirect immunization which is referred to as herd immunity. The direct immunization needs vaccines, which contain disease-causing microorganisms in the form of inactivated or live-attenuated states. These activate the immune system to produce disease-specific antibodies that protect an individual from catching the infection and make them immune against the disease that is the key effect of direct immunity. While indirect immunization is achieved when our body contracts infections and body automatically produces antibodies to fight off that infection. However, the magnitude of the direct effect of vaccine-derived immunity is a function of the transmissibility of the infectious agent, the nature of the immunity induced by the vaccine, the pattern of mixing and infection transmission in populations, and the distribution of the vaccine and, more importantly, of immunity in the population [16]. Some recent studies have estimated the basic reproductive number (R0) of the SARS-CoV-2 to be in the range of 2 to 6. In an initial cohort study, R0 of approximately 2.2 was estimated in 425 confirmed cases in Wuhan, China. That indicates an infected individual gives rise to 2.2 other infections on an average [17]. However, more recently Sanche, et al. reported a R0 higher at 5.7 [18]. Such variation in R0 reflects the difficulty of obtaining accurate R0 estimates in an ongoing pandemic, and the current estimated SARS-CoV-2 R0 values likely do not indicate a complete picture of the transmission dynamics across all countries. Although, the threshold for achieving herd immunity depends on R0 which indicate how infectious a particular disease is. In present circumstances, the possible ways to acquire the immunity against the SARS-CoV-2 immunity are (1) Expansion of safe and effective vaccine and a mass vaccination (2) Mass exposure of community with SARS-CoV-2 globally that may be termed as natural immunization [19]. Epidemiologists have estimated that at least 70% of the population needs to be immune to achieve that threshold. It is well known that for achieving herd immunity, a vaccine or 70% population getting infected with the disease and becoming resistant is a must [20]. However, at present vaccine is not available for COVID-19 yet, thus if a large proportion of the total population gets infected, then maybe herd immunity can be achieved.
The herd immunity might be a terrible idea because at present there are no preventive measures available to contain the spread of COVID-19. Thus, considering that coronavirus is highly contagious; if lockdown restrictions are removed the number might still be achievable. But, COVID-19 seems to be a lethal disease hence a large number of infections will not only overwhelm the hospitals but also may lead to high death rates. Globally many research groups are working on vaccines against COVID-19 and some of them showed good promising results. In Oxford University, a group of researchers led by Sarah Gilbert designed a vaccine that encodes the new coronavirus's spike protein, which it uses to invade host cells. The researchers injected in six rhesus macaques and the vaccinated monkeys developed neutralizing antibodies which can prevent a virus from entering cells against SARS-CoV-2. Vaccinated animals had much lower levels of viral RNA in their lung tissue than non-vaccinated animals, suggesting that the vaccine stopped the virus from multiplying in the monkeys' lungs [21]. The most important concern is whether the people infected by the new coronavirus can make antibodies against the virus or not because this response will be a key for the herd immunity. A recent study showed that persons getting infected with COVID-19 and recovering are making antibodies against the new coronavirus, suggesting they are immune from reinfection for an unknown length of time [22]. Another study finds that individuals who have had COVID-19 produce a robust response in immune cells called T cells. The adaptive immune system contains several main components: such as antibody-creating B cells, helper T cells, and killer T cells. The latter two are important for recognizing and destroying a particular virus, respectively. Alessandro Sette and Shane Crotty, both professors at the La Jolla Institute for Immunology, and their colleagues found that of a group of 20 people who had recovered from COVID-19, 70 percent had killer T cells and 100 percent had helper T cells that were specific to the SARS-CoV-2 virus, which causes COVID-19. Importantly, the researchers observed a strong T cell response to the "spike" protein which the virus uses to bind to and infect cells. This observation, they say, hints that exposure to seasonal common cold coronaviruses may confer some protection against the new pathogen [23]. The above findings show that infection with the novel coronavirus produces protective or neutralizing antibodies and suggests that people who have had COVID-19 infection possess at least some immunity. These results are an encouraging sign for the dozens of vaccines under development and give some plausibility of herd immunity effect also if the required infection threshold is achieved.
Anecdotal data suggest that there is always a risk associated with indirect immune effect especially when the disease is lethal and contagious but simultaneously this property of disease is also associated with herd immunity effect. There are ethical and legal consequences of herd immunity protection. Thus vaccination is the preferred choice to provide immunity to susceptible individuals. Traditionally vaccine has been key to achieve the direct and indirect immunity i.e. herd effect in the marked population. Although in the case of SARS-CoV-2 pandemic when the vaccine is not available, naturally acquired immunity is only the basis of herd immunity but the concept may cause great controversy. Theoretically, herd immunity may be achieved against novel coronavirus if 70% population gets infected. However, there is a perceived risk of millions of deaths also associated with this terrible concept. Earlier research findings showed that infection with the novel coronavirus produces protective or neutralizing antibodies, which are encouraging signs and gives some support to herd immunity concept. Simultaneously the findings raise many interesting and important issues about individual and public values in the current health emergency. At present, various types of vaccines are under development and some of them are under phase three clinical trial worldwide to contain the current pandemic. However, there is an intense need for an effective vaccine to acquire herd immunity and get rid of COVID-19 pandemic. Until a vaccine is available, personal protective equipment, hand hygiene, social distancing and lockdown appear to be the ways to slow down the transmission of the SARS-CoV-2 virus.