Human infections with zoonotic coronaviruses became an emerging worldwide health concern [1]. Previously Coronaviruses caused mild infections in immunocompromised people and were not considered to be highly pathogenic in humans until they circulated in the Guangdong province of China in 2002 and 2003 during the Severe Acute Respiratory Syndrome (SARS) outbreak [2]. A decade following the aforementioned SARS outbreak, we witnessed the emergence of the Middle East respiratory syndrome coronavirus (MERS-CoV) in Middle Eastern countries and, subsequently, Korea [3]. Recently, at the end of December 2019, Chinese authorities reported on cases of the acute respiratory syndrome that were linked to a novel Coronavirus that was named SARS-CoV-2 [4]. This new strain of coronavirus had not been previously identified in humans and the disease associated with it has been dubbed Corona virus diseases 2019 (COVID-19) by the World Health Organization (WHO). Since its emergence in Wuhan, China, the virus has spread to over 155 countries, causing severe morbidity and mortality [5]. Thus far, most of the infections and deaths have occurred in China. Due to its pathogenic characteristics and high rates of human infection, COVID-19 has become a significant public health concern and has been declared a public health emergency at a global level [1].
There is little knowledge about the characteristics of the newly emerging virus and its epidemiological traits. Understanding the severity and how best to treat the virus is present a challenge.
The purpose of this communication is to describe the epidemiological global trends, characteristics, and distribution of COVID-19 independently and in comparison, to SARS and MERS-CoV. The information gleaned from this analysis will help both to prepare countermeasures for the current COVID-19 outbreak and establish protocols to confront future outbreaks with novel coronaviruses.
COVID-19 is a positive single-stranded RNA virus genomically similar to SARS-CoV and MERS-CoV [6]. All three viruses are zoonotic and can be transmitted from animal to animal, animal to human, and human to human [7]. SARS-CoV, and MERS-CoV are known to have originated in bats and are directly transmitted to humans from live animal markets and dromedary camels [7]. Although there are no confirmed animal reservoirs for COVID-19, patients who initially contracted the disease had been to live animal markets in Wuhan, China [7]. The most supported mode of transmission for COVID-19 is via inhalation of infectious aerosols and large respiratory droplets [8]. The incubation period for COVID-19 is 2 to 14 days with an average of 5.2 days before the onset of symptoms. In comparison, the incubation period for SARS-CoV and MERS-CoV ranges between 2 and 10 days [9]. COVID-19 shares clinical characteristics with SARS-CoV and MERS-CoV. These include fever, cough, dyspnea, shortness of breath, myalgia, and possibly diarrhea [9]. Symptoms may progress to pneumonia, acute respiratory distress, and fatal hypoxemia [9].
The infectivity of COVID-19 has surpassed that SARS-CoV and MERs-CoV. The disease has spread globally at a rapid pace and continues to escalate.
The present analysis of COVID-19 situation is based on open source data from European Centre for Disease Prevention and Control [5]. Since 31 December 2019 and as of 3 May 2020, 3,388,665 cases of COVID-19 have been reported, including 243,312 deaths with a case fatality rate of 7.2%. About 2.5% of the total cases, and 1.9% of all deaths reported were from China where the pandemic originated. In contrast, the SARS epidemic of 2003 affected approximately 8000 cases with a fatality rate of approximately 10% worldwide [10]. Similarly, MERS-CoV epidemic in 2012, another corona class viral epidemic, affected 2519 cases globally and killed 866 cases, but with a case fatality rate of 34.4% [11]. Although the fatality of COVID-19 appears to be lower than prior corona virus-related epidemics, the overall burden and rapid global spread are cause for alarm.
Important information can be ascertained by studying distribution, seasonal, virulence, and transmission patterns of previous corona-virus epidemics. So far, COVID-19 has affected over 209 nations in the course of 125 days. Contrastingly, the SARS and MERS epidemics affected 26 and 27 respectively during their entire epidemic periods [1,12]. This clearly indicates aggressive transmission facilitated by enhanced infectivity and/or easy person-to-person transmission of COVID-19.
Although the current data on COVID-19 remains fluid [5], the pattern observed (Figure 1) predicts the following course: An epidemic peaking within a month, a pandemic, and a decline that will be observed by the end of the following month. The pattern of deaths from COVID-19 has followed a two-month pattern similar to incident cases (Figure 2). The pattern of a two-month epidemic cycle and mortality observed in China has been reflected in other countries (Figure 3 and Figure 4). Given this scenario, we could expect an epidemic decline within 3 months if rest of the world could enhance their response to COVID-19 based on Chinese experience by strictly adhering to virus containment and disease prevention protocols. Interestingly, the epidemic pattern appears to be a time-shortened version of the MERS-CoV outbreak in which a peak was observed within two months of a four-month epidemic cycle (Figure 5) [13]. This information forecasts a much quicker epidemic resolution for COVID-19 than for the MERS. Furthermore, the epidemic curve of COVID-19 followed a pattern similar to SARS epidemic in China that started in March 2003 and ended in 3 months rendering further support to emulate Chinese response in containing the disease globally [14,15].
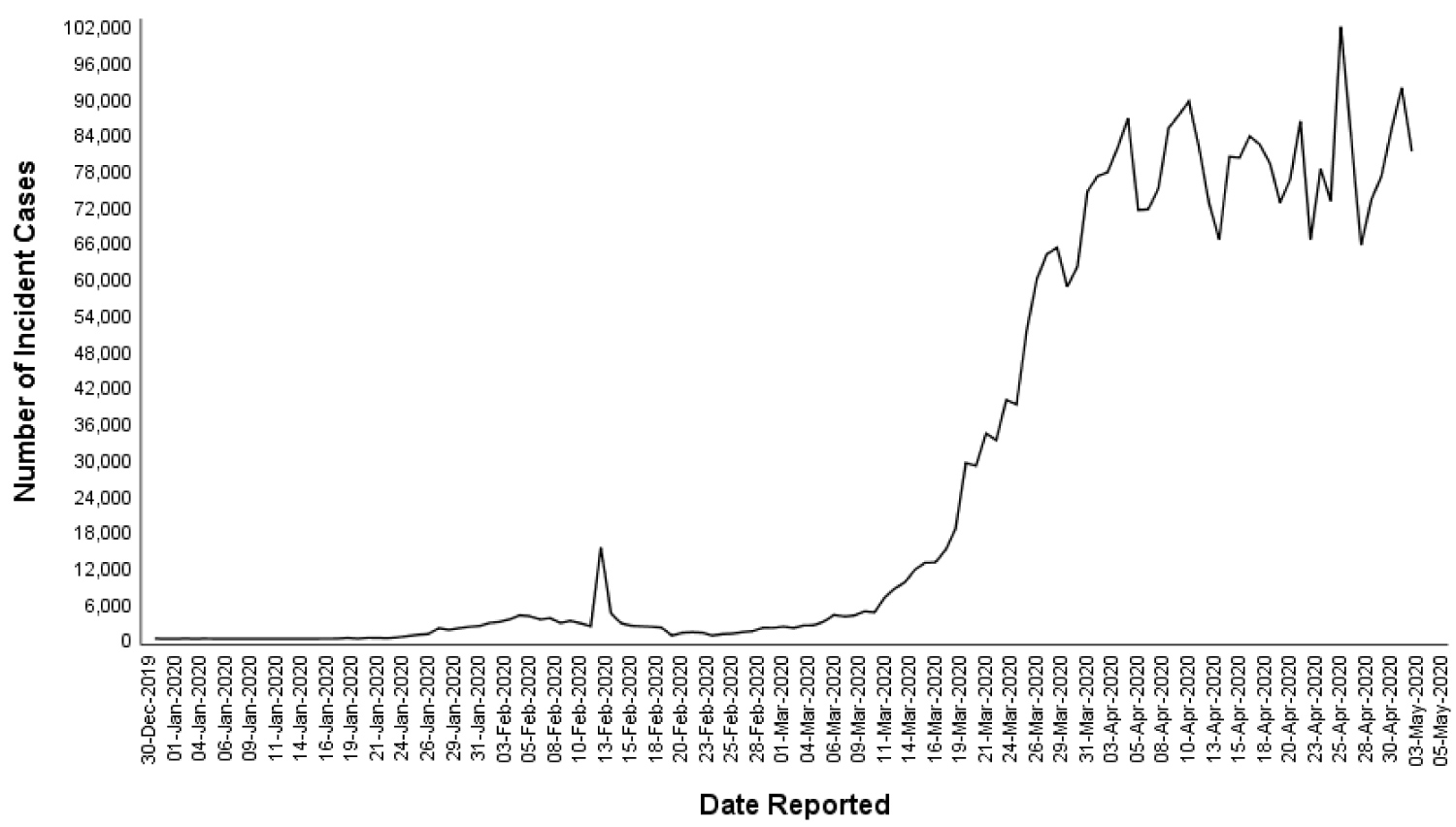 Figure 1: Global distribution of incident COVID-19 cases overtime, between 31st December 2019 and 3rd May 2020.
View Figure 1
Figure 1: Global distribution of incident COVID-19 cases overtime, between 31st December 2019 and 3rd May 2020.
View Figure 1
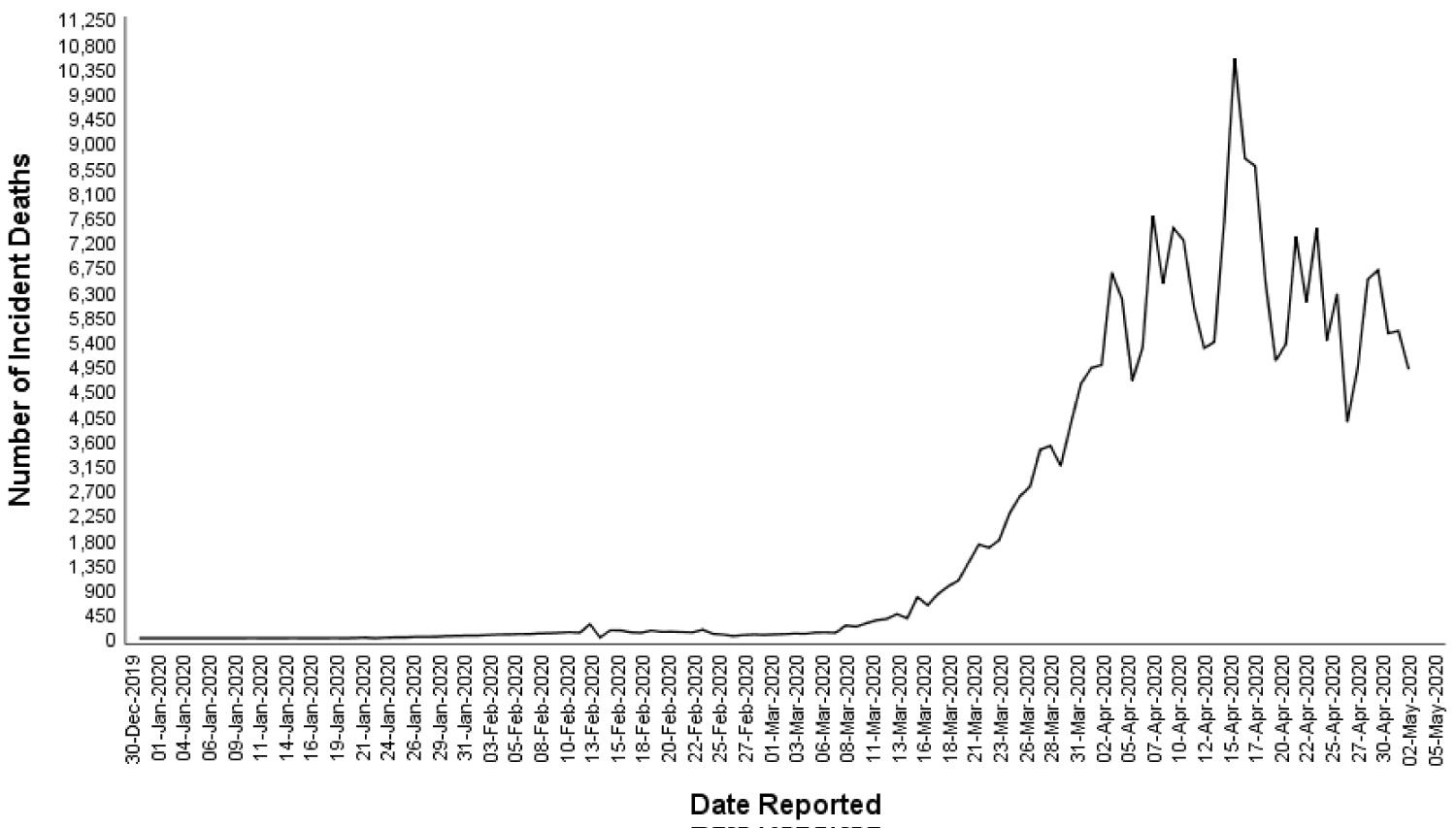 Figure 2: Global distribution of new deaths due to COVID-19 overtime, between 31st December 2019 and 3rd May 2020.
View Figure 2
Figure 2: Global distribution of new deaths due to COVID-19 overtime, between 31st December 2019 and 3rd May 2020.
View Figure 2
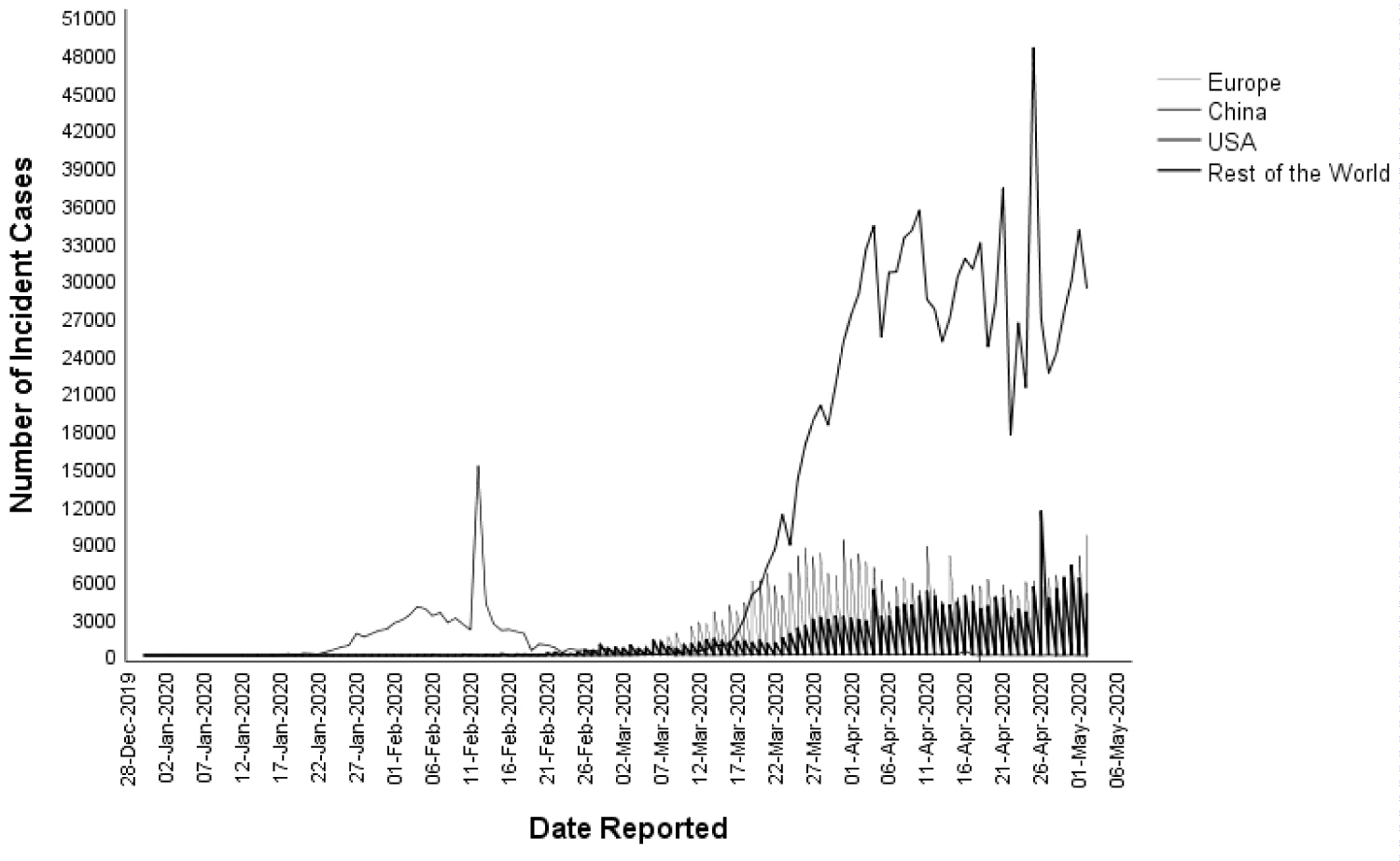 Figure 3: Distribution of incident COVID-19 cases overtime, between 31st December 2019 and 3rd May 2020, in China, USA, Europe, and Rest of the World.
View Figure 3
Figure 3: Distribution of incident COVID-19 cases overtime, between 31st December 2019 and 3rd May 2020, in China, USA, Europe, and Rest of the World.
View Figure 3
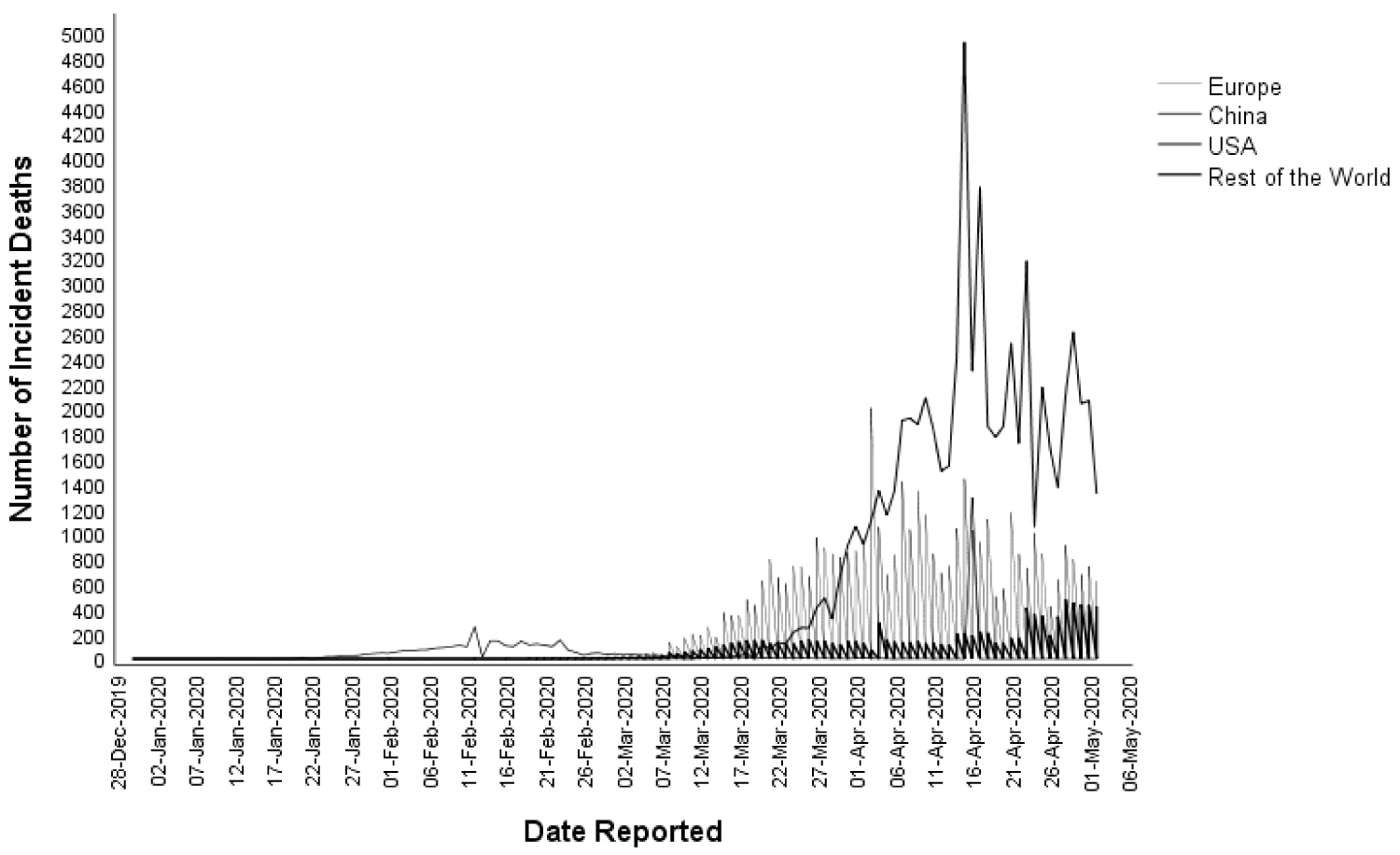 Figure 4: Distribution of new deaths due to COVID-19 overtime, between 31st December 2019 and 3rd May 2020, in China, USA, Europe, and Rest of the World.
View Figure 4
Figure 4: Distribution of new deaths due to COVID-19 overtime, between 31st December 2019 and 3rd May 2020, in China, USA, Europe, and Rest of the World.
View Figure 4
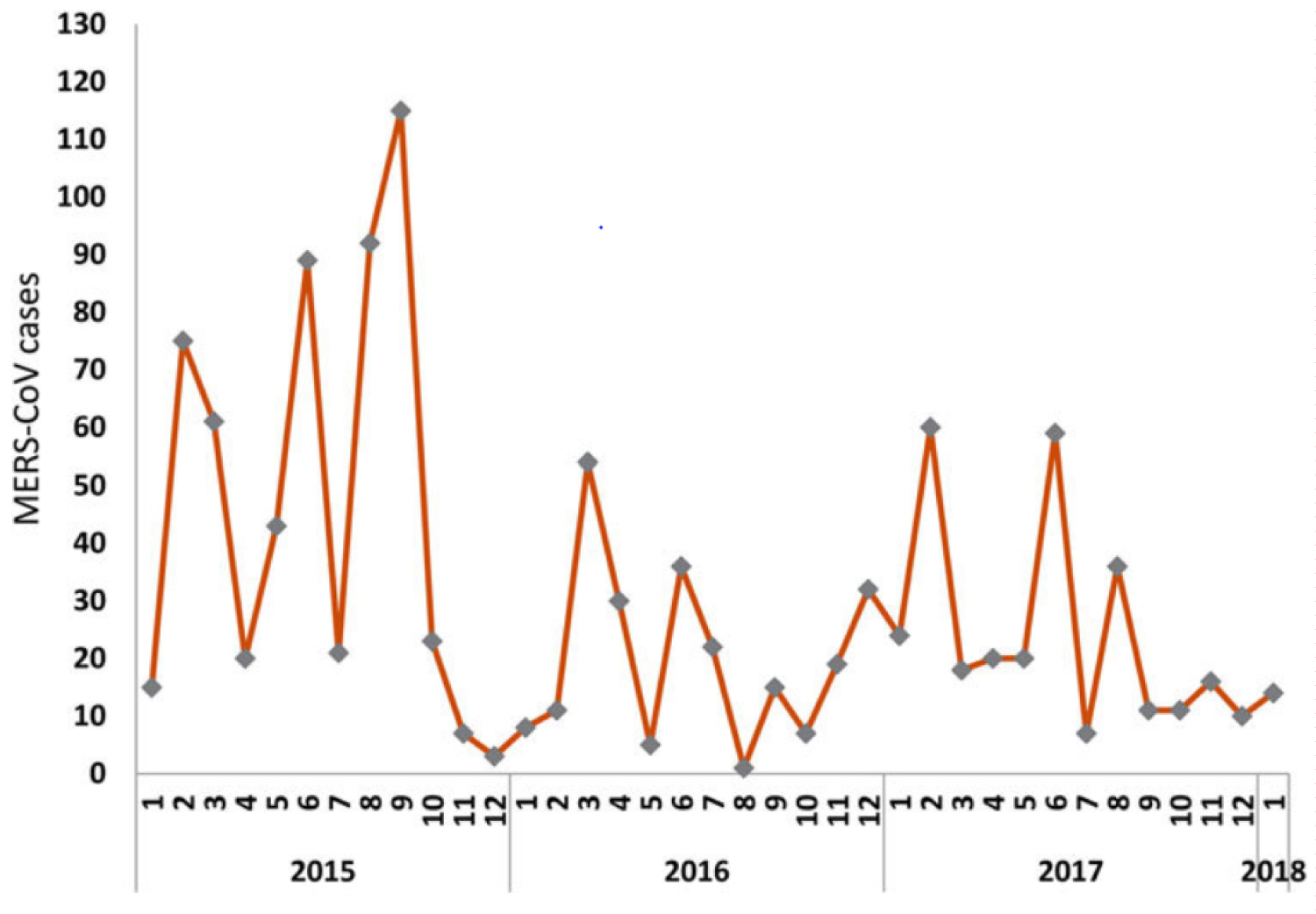 Figure 5: Time series of MERs-COV cases reported worldwide.
Figure 5: Time series of MERs-COV cases reported worldwide.
Source: Da'ar & Ahmed, 2018 [13]. Reproduced with the permission of authors.
View Figure 5
Despite the significant span of time between the first case of MERS-CoV in Saudi Arabia (Sept 2012) and the reported global outbreak of COVID-19, there have been no new large scale epidemic clusters of MERS-CoV reported in the last three years [11,16]. Moreover, it is interesting to note that the kinds of measures being taken in the current outbreak of COVID-19, including mass quarantines in various nations and extensive travel restrictions, were not implemented during the MERS-CoV outbreak. This is regardless of the fact that the reported case-fatality rate for the MERS-CoV outbreak was five times higher than that of the current COVID-19 outbreak as of May 3rd, 2020 (34.4% vs. 7.2%) [5,11].
Many questions have arisen regarding the consequences and outcomes of the current outbreak. Why was similar travel restrictions not implemented for the MERS-CoV outbreak despite its fatality? According to data reported since 2012, there have been less than 25 imported cases of MERS-CoV outside the Middle East [17]. Cases were reported in the United States, Asia (China, Malaysia, the Philippines, the Republic of Korea, and Thailand) and Europe (Austria, France, Germany, Greece, Italy, the Netherlands, Turkey and the United Kingdom [17]. For the current COVID-19 outbreak, symptomatic infected patients are mostly being diagnosed and treated in their countries of origin. However, there are many infected but asymptomatic individuals that are being permitted travel abroad and facilitate the spread of the virus.
Interestingly, published data on the current COVID-19 outbreak has shown that that the fatality rate from the virus in some regions of China in which the population exceeds that of whole nations is notable low [18]. For example, Hunan province of China with a population of 68.99 million experienced a low case fatality of 0.4% compared to Italy (13.7%), UK (15.4%), France (18.9%) and Spain (11.6%) [5,18]. Also notable are the differences in case fatality rate distributions from one Chinese city to the next. For example, the case fatality rate in Hubei is 6.6%, while that in Hunan is 0.4%. Moreover, the incidence of confirmed cases is also highly variable from one city to the next. In Hunan, for example, the incidence of the confirmed cases was 1.5 per 100,000 population, compared to 115.1 per 100,000 population in Hubei, and 5.9 per 100,000 nationwide [18]. These figures also varied from one country to other or from one region to another indicating a diverse geographic effect. Based on confirmed cases from Italy, Spain, Iran and India the incidence of COVID-19 varied between 3.0 per 100,000 in India to 463.5 per 100,000 in Spain [5].
Comparing COVID-19 statistics to MERS-CoV statistics can provide some perspective. The World Health Organization (WHO) has reported a total of 2,519 globally confirmed MERS-CoV cases with 866 associated deaths from 2012 until 31 January 2020 [11]. This translates to a case fatality rate of 34.4% globally. In Saudi Arabia, the country of origin of MERS-CoV, a total of 2,102 cases, including 780 related deaths and a case fatality rate of 37.1% at the end of 2019 was reported [16]. This means that the cumulative incidence of the disease was 6.4 per 100,000 populations in Saudi Arabia. These incidence and fatality rates are 1.1 and 6.7 times higher respectively than the incidence and case fatality reported for COVID-19 in China. The statistical comparisons shed light upon an important question: why are extreme worldwide restrictions and protective measures being taken for COVID-19 when they weren't for MERS-CoV? Although Mecca in Saudi Arabia hosts 3 million pilgrims annually, there were no cases reported of MERS-CoV during the peak of the outbreak in Saudi Arabia [19].
It would appear that China has managed to gain control of the COVID-19 pandemic within their country. As evidenced by the rapidly falling infection rates within China, the global epicenter of the COVID-19 outbreak appears to have successfully implemented policies to combat the disease. Although it takes significant healthcare system resources and leadership, China has demonstrated that control of the COVID-19 pandemic is possible even with a massive population. As the infection rates in other countries rise (Figure 4), there are important public health and leadership lessons that can be gleaned from the success of China in controlling this outbreak.