COVID-19, a pandemic, is an expanding global threat that has nearly affected all the countries in the world. As the pandemic advances without any medical intervention in place, a global lockdown has been issued along with quarantine orders and social distancing restrictions to prevent further transmission. We discussed the transmission and control effort of COVID-19 based on available information since the disease outbreak. COVID-19 can be symptomatic or asymptomatic, spreading from person-to-person either by respiratory droplets or touching contaminated surfaces. People with underlying medical conditions such as hypertension, diabetes mellitus, and respiratory illnesses are more prone to having a critical disease. Federal, state and local governments have taken effective measures in preventing further transmission by imposing social distancing and isolation, to stop the spread via travel-related cases, which can also influence local spread. To date, there is no vaccine licensed for use and the only therapeutic strategy is supportive care. Chloroquine and hydroxychloroquine, two antimalarial agents, are currently being tested and used as therapeutic agents in the management of COVID-19. This study described the transmission and control effort of COVID-19 hoping that this study will inform the global community of the virus transmission and different public health measurements implemented to prevent further spread.
Coronavirus, COVID-19, SARS-CoV-2, Global Outbreak, Transmission and Control
Coronavirus is classified as a positive-sense, single-stranded RNA virus [1]. This virus circulates among humans, other mammals, and birds. It causes a wide variety of respiratory, enteric, hepatic, and neurological illnesses [2]. It was reported that in December of 2019, a cluster of patients with pneumonia of unknown cause was linked to the seafood and wet animal wholesale market in Wuhan, Hubei province, China [2]. Chinese scientists later identified this novel-coronavirus as the main causative agent [3]. The disease is now referred to as coronavirus disease 2019 (COVID-19) and severe acute respiratory syndrome-associated coronavirus (SARS-CoV-2) is the causative agent.
The spread of COVID-19 can be characterized by 3 distinct phases: An initial phase of slow accumulation of new infections that are often undetectable, the second phase of the rapid growth of infection that could lead to death, and eventually a slowdown of transmission due to the depletion of susceptible individuals [4]. This third phase leads to the termination of the first epidemic wave of transmissibility [4] and therefore, implementation of control measures such as travel bans, and social distancing can elicit protection from the disease spread [4].
The first case of COVID-19 was reported in Wuhan, China in December 2019 and subsequently, this virus has affected about 332,930 people worldwide with 14,510 deaths, as of March 23, 2020 [5]. The current number of cases in China is 81,704 with 3,285 deaths. This virus has been declared a pandemic by the World Health Organization (WHO) and it continues to spread. The total number of infected people in the United States of America (USA) has reached 47,927 with 603 deaths, as of March 23, 2020 [5]. A global effort is in action to prevent the further spread of this infection and many researchers have been working to find the cure for this threat. The distribution of COVID-19 cases in China and the USA is further illustrated in Figure 1 with data as recent as of March 23, 2020 [6].
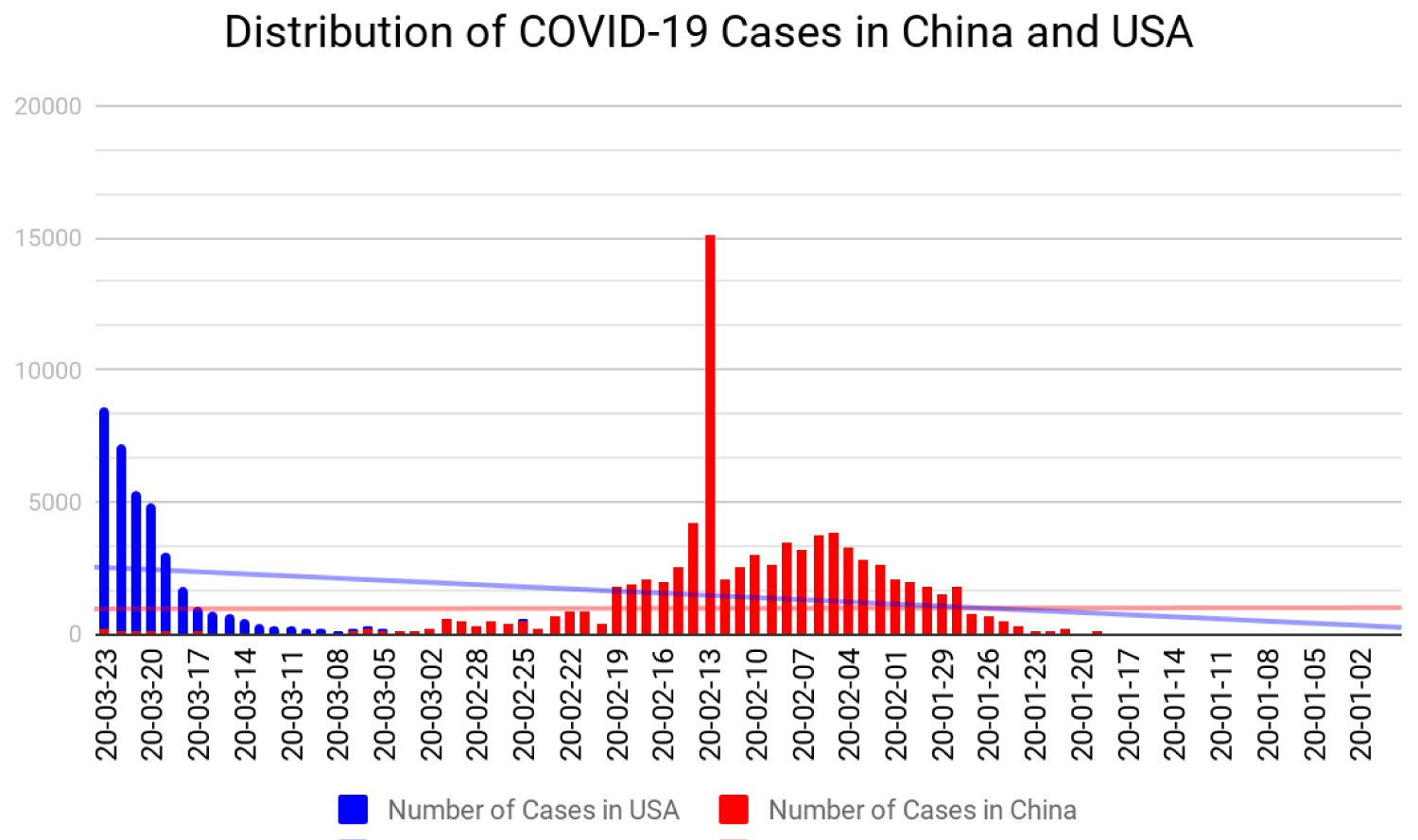 Figure 1: Distribution of COVID-19 cases in China and USA.
View Figure 1
Figure 1: Distribution of COVID-19 cases in China and USA.
View Figure 1
It is estimated that outside mainland China, the USA, Australia, and the United Kingdom (UK) have had an import of higher case counts [7]. Reported case counts are estimated based on the volume of passengers from Wuhan who has imported the disease to these places [7], suggesting travel transmission initially and thereafter local community transmission. The first wave of inter-country spread has targeted Asia (Iran), not including mainland China, the Pacific (Australia) region, North America (USA) and Europe (Italy) [7]. Furthermore, there are many countries where these imported cases have not been detected, perhaps because the cases could not be isolated, or the transmission has been truncated [7].
We aim to describe the transmission pattern and control efforts of the ongoing COVID-19 outbreak, hoping that this study will inform the global community of the response measures undertaken by different countries to contain the spread of the virus.
The coronavirus is categorized as a medium-sized, enveloped, positive-stranded RNA virus [8]. The coronavirus’ large viral RNA genome encodes for necessary structural proteins that aid in its growth. The spike (S) protein projects through the viral envelope and forms the characteristic spikes that surround the coronavirus [8]. These (S) spikes promote receptor binding and fusion with the host cell membrane. The membrane (M) protein on the outer surface of the envelope performs an essential role in viral assembly [8]. The nucleocapsid (N) protein binds with the RNA genome to form the nucleocapsid, which helps regulate viral RNA synthesis [8]. The coronavirus undergoes viral RNA replication in the cytoplasm of its host cell using an RNA polymerase to start gene transcription [8]. The coronavirus is subclassified further into 4 genera (alpha, beta, delta, and gamma) with the alpha and beta genera types identified to cause disease in humans [9].
The entry of the coronavirus into a cell depends on the (S) protein binding to a cellular receptor, which facilitates viral attachment to the surface of target cells [10]. While there is still much currently unknown about COVID-19, a closer study of SARS-CoV could indicate viral transmission patterns and inclinations. As with other coronaviruses, the outward projecting spike (S) protein facilitates viral entry into target host cells and mediates the initial binding to a receptor on the surface of susceptible cells [11]. This SARS-CoV receptor was identified by mass spectrometry as ACE2 (angiotensin-converting enzyme 2), a zinc metallopeptidase that has been identified as a homolog of ACE (angiotensin-converting enzyme); an important regulator of blood pressure [11]. ACE2 has been associated with heart function, hypertension, and diabetes and is mediated through its ability to convert angiotensin 2 [12]. ACE2 functions in both the cardiovascular and immune systems in healthy persons and plays a role in the development of hypertension and diabetes mellitus. The coronavirus enters the host cell through the (S) protein binding to the ACE2 that is found in the lungs and heart, with a high affinity to invade alveolar epithelial cells [12].
Unlike the complications arising from influenza cases, where respiratory failure is usually caused by pneumonia from a secondary bacterial infection, studies based on the past SARS-CoV outbreak may indicate that COVID-19 is directly causing a primary viral pneumonia [13]. SARS-CoV primarily targets epithelial cells of the alveoli and the conducting airways in the human lungs, as these cells are found to express ACE2, an enzyme that also acts as the SARS receptor [13]. With alveolar type 2 cells being one of the major cell types to be susceptible to infection, the diffuse nature of the alveolar damage would lead to an increased inflammatory cytokine response by the immune system, which would further damage the epithelium, causing disruptions in the areas involved in gas exchange and in the conducting airways [13]. However, despite notable elevations in serum concentrations of proinflammatory cytokines, such as IL-10 and IL-8, it is still unclear whether the cytokines were produced by the epithelial cells of the alveoli and conducting airways, where the virus was replicating; or by inflammatory cells at the site of infection [13]. Although the possibility of a secondary superinfection exacerbated by a primary viral infection by SARS-CoV-2 hasn’t been indicated, due to the limited information available, it should not be ruled out. Furthermore, the immune response to SARS-CoV-2 is not yet fully understood, but based on based on the Middle East respiratory syndrome coronavirus (MERS-CoV) cases, patients with SARS-CoV-2 are unlikely to be re-infected shortly after their initial recovery [14].
While generally associated with mild-to-moderate illness in previously healthy individuals, COVID-19 has been associated with more complicated and debilitating illnesses. On December 29, 2019, the first 4 reported cases were identified by local hospitals in Southern China that relied on using the surveillance mechanism for "pneumonia of unknown etiology" developed during the 2002-2003 SARS (severe acute respiratory syndrome) outbreak [15]. Recent reports indicate that COVID-19 has been recognized in other Chinese cities and in over a dozen countries worldwide due to international travel [15].
Asymptomatic individuals, as well as those with symptoms, express high viral load within the first few days despite the patient symptomatology [16,17]. In addition, infection transmission by those without symptoms can make control effort of the disease rather challenging [16]. Current data indicate that coronavirus transmission can spread from both asymptomatic and symptomatic persons to other persons through respiratory droplets that remain in the air, deposits on surfaces, and possible fecal-oral route of transmission [12]. The vertical method of transmission should also be considered as another possible method of spread, based on a recent cohort study conducted by Lingkong and colleagues. The study examined 33 neonates born to mothers with confirmed COVID-19 pneumonia from the Wuhan Children's Hospital, in Wuhan, China [18]. Among those examined, 3 of the neonates were identified as having COVID-19, with shortness of breath being the most common symptom [18].
The coronavirus can remain viable and infectious in aerosols for hours and on surfaces for some days; and has been detected on plastic and stainless-steel surfaces more than 72-hours later [12,19]. The incubation period, based on 158 confirmed cases outside Wuhan, is estimated to be 5.1 to 5.2-days, with a range of 2 to 14-days, and is consistent with the incubation period estimates from confirmed cases in China [20]. The current recommendation after any potential exposure is a 14-day period of monitoring and self-quarantine, with current predictions citing that 101 out of every 10,000 cases (99th percentile) will develop symptoms after the initial 14-days [20].
People with comorbidities are more likely to be infected, especially those with hypertension, coronary heart disease or diabetes. Patients with existing cardiovascular disease are seemingly more likely to develop severe respiratory symptoms if infected [21], with data suggesting that patients with cardiovascular disease also account for a large proportion of deaths from COVID-19. Among the patients with severe symptoms of COVID-19, the data from a recent study indicates approximately 58% had hypertension, 25% had heart disease and 44% had arrhythmia [21]. The mortality data released by the National Health Commission of China (NHC) indicates that 35% of patients with infection had a history of hypertension and 17% had a history of coronary heart disease. The data also showed that patients greater than 60 years of age who were infected had severe pneumonia, possibly indicating a link to cardiovascular disease; further aggravating pneumonia and the severity of symptoms [21]. At the time of this entry, on March 29, 2020, the number of confirmed cases globally was 634,813, of which 103,321 cases in the USA alone were as a result of local transmission, indicating that the source of infection is within the reporting location [22].
Past studies have proposed that bats could serve as the main reservoir for the coronavirus [9], similar to how the severe acute respiratory syndrome coronavirus (SARS-CoV) and the MERS-CoV rapidly spread from animals to humans and cause severe respiratory illness [13]. It is speculated that other peridomestic mammals, such as pangolins [16] may serve as intermediate hosts [9,16], and also possibly assist in the process of gene exchange such as recombination and mutations promoting an increase in viral genetic diversity [9]. When SARS emerged in China in 2002-2003, it also had an element of human transmission that was thought to be promoted by intermediate hosts like civet cats and raccoon dogs, which are commonly sold as a source of food in Chinese wet markets, with the Chinese horseshoe bat serving as a natural reservoir [13]. This trend can be seen again in the early days of the COVID-19 outbreak, as the initial groups of infections that arose in Wuhan were also linked to the Huanan seafood markets [13]. Besides, SARS-CoV-2 affects many families who have not visited the wet market, suggesting a person-to-person pattern of disease spread [23,24].
The COVID-19 disease that started in Wuhan, China has been exported globally [25]. The USA and other countries have taken measures to restrict travel within and outside their borders to slow the spread of the disease [25]. In addition, Figure 2 illustrates the mitigation measures that can ensure a break in the chain of infection [14]. Despite these measures, the Centers for Disease Control and Prevention (CDC) estimates that in the USA the total cumulative number of reported cases between January 12 and April 12, 2020, has passed 500,000 cases [26] and over 20,000 patients have died [26]. Of the confirmed cases, 6,515 were travel-related, 13,341 were contracted from close contacts and 534,993 cases are being investigated [26]. The majority of these cases were seen in densely populated areas, and as of April 01, 2020, the USA had more coronavirus cases than any other country in the world [26]. In the USA, these cases emerge in hotspots such as New York, which has the highest number of cases with an estimated 188,694 confirmed cases and 7,349 deaths as of April 13, 2020 [26]. In addition to New York, Washington State, California and New Jersey have also seen an increase in the number of confirmed cases [26]. Other hotspots are emerging nationwide and according to the CDC, Louisiana has experienced a surge in cases of COVID-19 with 21,016 confirmed cases and 884 deaths, as of April 13, 2020 [26].
 Figure 2: Preventing the spread of COVID-19.
View Figure 2
Figure 2: Preventing the spread of COVID-19.
View Figure 2
Due to the severity of the disease and the lack of specific therapeutics and vaccines, the federal, state and local governments have taken measures to prevent local transmission [25] given that the virus can be transmitted by aerosols which could remain suspended in the air for minutes-to-hours after a cough or sneeze [27]. Moreover, these expelled viral particles can remain viable on various surfaces for some days [27]. Reduced transmissibility relies on public health tools such as isolation, social-distancing, quarantine, and community-wide containment to bring about reducing interaction between people, in order to slow the spread of the disease [25]. Isolating an infected person will interrupt the transmission to an uninfected person [25], while an exposed individual should be quarantined to avoid transmission even before symptoms develop [25]. COVID-19 transmission appears to thrive in drier and cooler environments, despite global efforts to quarantine, increase hand hygiene, social distancing, and other public health measures [28]. The outbreaks in Western Europe, the USA, and Iran have grown exponentially and perhaps may be due to temperature, humidity and health infrastructure [28]. Therefore, it is assumed that temperature, humidity and health infrastructure dependence have the ability to assist in curbing the spread of the disease [28]. Human behavior and hygiene are major determinants of spread, but the relationship between higher temperature and absolute humidity has been shown to lower a number of cases, hence, affecting viral transmissibility [28]. Lower temperatures alone can result in systematically worsening the immune system, which can hypothetically cause a greater effect in COVID-19 transmission [28].
Although the current approach to the management of COVID-19 consists mainly of prevention and control measures, as well as supportive care when needed, a variety of therapeutic approaches are being explored [26]. As researchers worldwide are currently developing vaccines and other mitigation strategies against COVID-19, antiviral medications such as lopinavir-ritonavir and remdesivir [26,29] are being investigated. A randomized clinical trial that compared lopinavir-ritonavir to standard care showed that lopinavir-ritonavir has no treatment benefit when compared to standard care [30]. Similarly, chloroquine and hydroxychloroquine that are used to treat malaria and other inflammatory conditions are also being investigated as therapeutic agents against COVID-19. These drugs have been shown to have in-vitro activity against other coronaviruses, including SARS-CoV-2 [29]. One study conducted in China showed that chloroquine improved patients' clinical outcomes when compared to a control group, and it is currently being used as a therapeutic measure [26,31]. Although data on the use of chloroquine and hydroxychloroquine is still limited and anecdotal, these drugs are currently recommended for the treatment of hospitalized COVID-19 patients in several countries, including in the USA.
There is no predictability as to how COVID-19 will behave given that the entire world population lacks immunity [28]. The best response is continual isolation; prompt identification of cases and contacts, strict quarantines, travel restrictions [32], social distancing, personal hygiene, and other intensive efforts, rather than just relying on a change in the season [28] and the development of a more appropriate therapeutic approach. Managing COVID-19 is a global struggle, as a true shutdown would be too difficult given the monumental financial and social consequences associated with supply chain disruptions and supply shortages, as seen particularly among the healthcare professionals worldwide who are taking care of COVID-19 patients without easy access to proper personal protective equipment (PPE) [28,33].
SARS-CoV-2 is a widespread infectious virus that has impacted enough individuals to be classified as a large-scale pandemic. It has infected over a million individuals within a few months since the start of the outbreak. Due to its alarming rate of spread, countries have been struggling to implement their domestic solutions, and these methods have thus far been inadequate, even amongst the most developed nations. Closing borders, social distancing, and enforcing mask requirements are some ways that individual governments can attempt to prevent transmission and mitigate the disease. Amongst countries that have been relatively successful in managing the pandemic, it is clear that they are only as safe as the weakest link in their delicately balancing system. Further research is needed to understand any additional method(s) of transmission and avoid further spread of the disease. Alongside understanding the virus, efforts to combat COVID-19 must be accelerated to find treatment for those that are infected and also a preventive vaccine for those who are not yet infected; the combination of these solutions could lead to the quelling of the outbreak.
None.
A.S: Conceptualization, and design, approval of the final version, responsibility for accuracy, and integrity of all aspects of research. C.O: Supervision and revising the article for intellectual content; editing. S.Y: Writing-review and editing. H.C: Writing-review and editing. N.H: Writing-review and editing. A.F.A: Writing-review and editing. O.A: Writing-review and editing. S.P: Writing-review and editing. A.M: Writing-review and editing; project administration.