Unnecessary antibiotic use in nursing home patients leads to negative outcomes including the emergence of multi-drug-resistant bacteria, adverse drug events, polypharmacy and higher health care costs. The purpose of this study was to develop and assess the effects of a pilot clinical staff educational intervention on best practices for the management of asymptomatic bacteriuria (ASB) in nursing home residents.
A multi-faceted educational intervention program on ASB was provided to Emergency Department clinical staff at Butler Memorial Hospital-a non-profit organization and independent community hospital in rural Pennsylvania. The effectiveness of the program was assessed by evaluating the pre- and post-intervention rates of unnecessary antibiotic prescribing among nursing home residents presenting to the Emergency Department with ASB.
A total of 105 participants with ASB were included in the study over a 10-month period. Seventy-three patients were encountered before the educational intervention, and 32 post-intervention. Among these, the rate of unnecessary antibiotic prescribing was reduced from 16.4% pre-intervention to 12.5% after the intervention.
This study provides important educational materials on ASB management and adds to a growing line of evidence suggesting that education on good practices for ASB may be effective in reducing the rate of unnecessary antibiotic prescribing among nursing home residents.
Current guidelines of the Infectious Diseases Society of America define asymptomatic bacteriuria (ASB) according to a specified number of bacteria in urine in the absence of typical urinary tract infection (UTI) symptoms [1]. These guidelines recommend no antimicrobial treatment for ASB except in specified populations, such as pregnant patients or those anticipating a urologic interventional procedure. Despite these guidelines, antibiotic overuse for ASB appears to be widely prevalent in clinical practice, as indicated by several studies reporting that 20-80% of ASB cases are inappropriately treated [2].
Nursing home residents frequently experience ASB, and the symptoms are often mistreated as UTIs. Even in the absence of specific (e.g., dysuria) or non-specific (e.g., fever) signs or symptoms of UTI, nursing home residents frequently receive an antibiotic for a suspected infection [3]. Up to 70% of nursing home residents receive at least one antibiotic agent per year [4], and this practice may be associated with unnecessary negative patient outcomes. Treatment of ASB has been shown to have no clinical benefit in reducing the frequency of symptomatic UTI or ASB, whereas it predisposes patients to the emergence of multi-drug-resistant bacteria, adverse drug events, polypharmacy and increased health care costs [5]. These considerations are especially important in the frail elderly population with frequent comorbidities. National guidelines indicate that men and women over the age of 65 should not receive antibiotic treatment for ASB [6], and the American Geriatrics Society has emphasized the importance of not prescribing antibiotics to elderly people with ASB [7]. Reducing antibiotic overuse for ASB in nursing home residents is therefore an important issue for responsible antimicrobial stewardship [2,4].
A knowledge gap exists among emergency department providers and healthcare staff regarding treatment of ASB, and education on this topic is crucial for positive patient outcomes. Previous studies have suggested that providing education on published guidelines for ASB management to healthcare providers may help reduce mistreatment of ASB cases [2]. A study conducted by Walker, et al. [8] aimed to explore the perceptions, attitudes and opinions of physicians and nurses involved in prescribing antibiotics for ASB in institutionalized elderly people. Focus groups were conducted among physicians and nurses who cared for residents of long-term care facilities [8]. The ordering of urine cultures and the prescribing of antibiotics for residents with ASB were found to be influenced by a wide range of nonspecific symptoms or signs. The physicians believed that the presence of these signs justified the decision to order antibiotics. Nurses played a central role in both the ordering of urine cultures and the decision to prescribe antibiotics through their awareness of changes in the residents' status, and communication of this information to physicians. The presence of non-urinary symptoms and signs was an important factor in the prescribing of antibiotics for ASB in the institutionalized elderly population, and the study concluded that education on ASB is an important priority for both physicians and nurses [8].
Another study conducted by Irfan and colleagues [9] aimed to reduce risk factors and assess the effects of educational interventions on over-prescribing for ASB. Evaluated variables included the appropriateness of ASB management, as well as physician knowledge and practices regarding ASB. The participants were consecutive patients with positive urine cultures, and the study was conducted in two tertiary teaching adult care hospitals. Educational sessions were implemented that provided a) An overview of the evidence for best practices of ASB management, b) Feedback on baseline assessment findings, c) Clarification of misconceptions regarding ASB management (i.e., risk factors associated with inappropriate treatment of ASB identified during the baseline data collection period), d) Feedback about the initiative, e) Discussions of recent cases and f) Information on appropriate indications for urine culture, specifically for patients with symptoms of UTI [9]. The educational interventions were effective in reducing the rate of inappropriate antibiotic use in ASB cases to less than 10%, and the results were sustained in a follow-up over 2 years [9]. Similarly, Zabarsky, et al. [10] found that an educational intervention directed at nursing staff and primary care providers resulted in significant reductions in both the inappropriate submission of urine cultures and the overall rate of treatment of ASB. These studies demonstrate the importance of combatting prevalent inappropriate ASB treatment in the institutionalized elderly population. Furthermore, responsible antibiotic stewardship is crucial for reducing bacterial drug resistance in the general population.
Butler Memorial Hospital is an independent, non-profit community hospital in rural Pennsylvania that serves a large population of nursing home residents in the surrounding area. The staff of Butler's Emergency Department, as well as local nursing home providers, have voiced a need for improved antibiotic stewardship in the care of nursing home residents presenting with signs and symptoms of ASB. The present study sought to develop an educational intervention on ASB management and generate preliminary data to evaluate whether the intervention could reduce the prevalence of unnecessary antibiotic prescribing to nursing home residents with ASB who present to Butler Health System's Emergency Department. This research aimed to increase the quality of care delivered by Butler Memorial Hospital's Emergency Department and thus improve patient outcomes. Furthermore, this study may add to the increasing evidence demonstrating the need for and utility of educational interventions on ASB management.
Butler Memorial Hospital is an independent community hospital with 296 beds that opened in 1898. It is a non-profit organization located in the rural community of Butler, Pennsylvania. Butler Memorial Hospital's Emergency Department treats many nursing home residents from the surrounding community. The Emergency Department of Butler Memorial Hospital served as the setting for the research project.
A multifaceted educational intervention was provided to the Emergency Department staff at Butler Memorial Hospital in order to emphasize the importance of not treating institutionalized elderly patients with ASB as well as other patients meeting the Infectious Disease Society of America's criteria for no treatment. The educational material provided in this study included an overview of the evidence regarding ASB management, clarification of misconceptions related to ASB management; and discussion of cases that residents had recently encountered, and appropriate indications for urine culture, specifically for patients with symptoms of UTI. The intervention was implemented in several ways. First, a self-serve educational module (in Microsoft PowerPoint) on ASB management was set up in the ED breakroom for staff to review at their convenience. The module is presented here as a Supplementary File 1. In addition, pocket cards highlighting the Infectious Diseases Society of America guidelines for ASB treatment were provided to emergency department staff as a reference and placed as posters on walls throughout the ED (Figure 1). The pocket cards included an algorithm, created by the primary investigator, detailing when to screen and treat ASB patients, along with the Infectious Diseases Society of America guidelines and criteria for the diagnosis of bacteriuria. Third, the clinical staff leader reviewed the above materials with staff in their monthly staff meeting. These interventions were implemented beginning Aug 1, 2018 and continued throughout the remainder of the study.
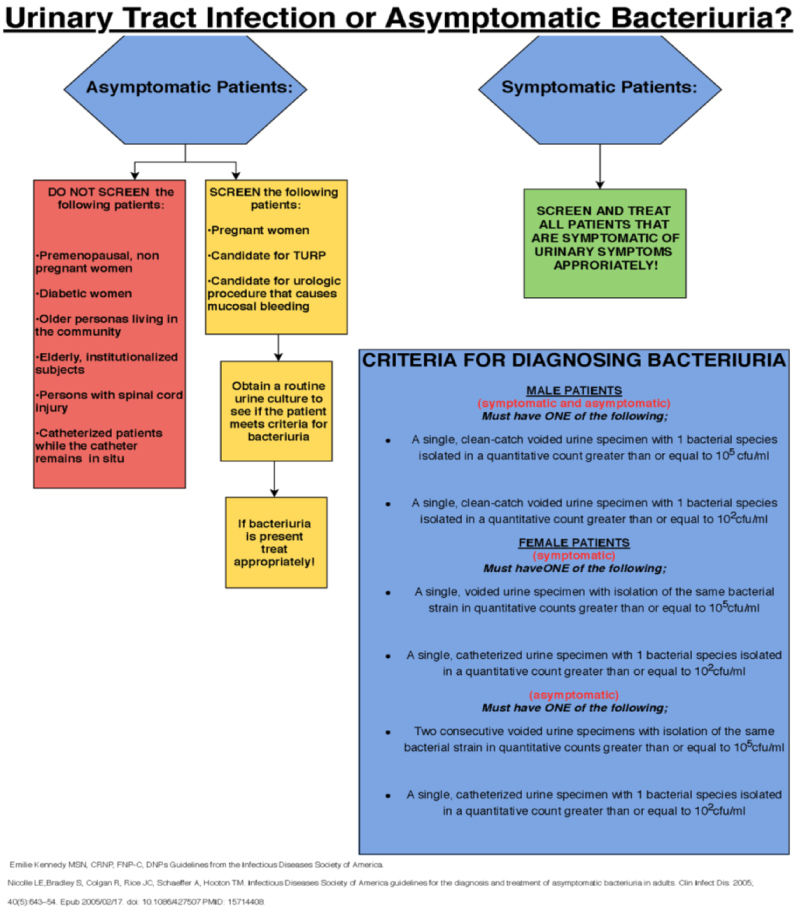 Figure 1: ASB educational pock card and poster. As a component of the educational intervention, pocket cards on ASB management were distributed to ED staff, and posters were placed throughout the ED. View Figure 1
Figure 1: ASB educational pock card and poster. As a component of the educational intervention, pocket cards on ASB management were distributed to ED staff, and posters were placed throughout the ED. View Figure 1
The participants in this study comprised patients residing in institutional facilities for the elderly who presented to the Emergency Department of Butler Memorial Hospital from Feb 1, 2018 to Nov 10, 2018. By retrospective chart review, the patients were included in the study if they met the following standard criteria for ASB: no urinary symptoms; discharge back to the nursing home; and a first positive urine culture, defined as bacterial growth of at least 105 CFU/mL. Patients were excluded from the study if they showed a first positive urine culture of mixed growth, defined as more than three organisms [11]. Participant data were collected including age, gender, presence of indwelling catheters, and whether the patients were discharged on antibiotics for urinary symptoms. Data were collected before and after the educational intervention for comparison.
Data were collected for 6 months before the educational intervention (Feb 1 - July 31, 2018) and 3 months after implementation of the intervention (Aug 10 - Nov 10, 2018). This research project utilized a quasi-experimental design. Emergency Department staffs were provided with the educational intervention, and the primary outcome of the study compared the percentage of ASB patients given antibiotics before and after the educational intervention. Data were analyzed using Microsoft Excel.
The Institutional Review Boards at Edinboro University of Pennsylvania and the Butler Health System both approved the on-site data collection procedures for this study. Both boards provided the research team with a waiver of written consent. There were no physical, psychological, financial, socioeconomic or legal risks, or harm due to confidentiality to participants in this study.
Butler Health System's Emergency Department receives numerous nursing home patients from the surrounding area. Over the study period, a total of 105 residents met the criteria for ASB and were included in the study. Among these, 73 were seen in the 6 months before the educational intervention, and 32 in the 3 months post-intervention.
Demographics of the participants are presented in Table 1. The full cohort included 32 males and 73 females, with a mean age of 81.8 years (range: 53-97). For the 73 pre-intervention patients, there were 20 males and 53 females, with an average age of 82.6 years (range: 53-97). Among the 32 patients encountered after the intervention, there were 12 males and 20 females, with an average age of 80.0 years (range: 61-97). Nine participants had indwelling Foley catheters, including 7 in the pre-intervention cohort and 2 in the post-intervention cohort.
Table 1: ASB participant demographics. View Table 1
The rates of antibiotic prescribing were assessed among the participants before and after the intervention (Figure 2). Among the 73 patients with ASB encountered before the intervention, 12 (16.4%) were unnecessarily given antibiotics and discharged back to the nursing facility following an inaccurate diagnosis of UTI. Within this latter group, 8 were females and 4 were males, and 3 of the patients had indwelling Foley catheters. Of the 32 patients with ASB seen after the educational intervention, 4 (12.5%) were given antibiotics for an inaccurate UTI diagnosis and discharged to their facility. All four of patients were female, and one had an indwelling Foley catheter.
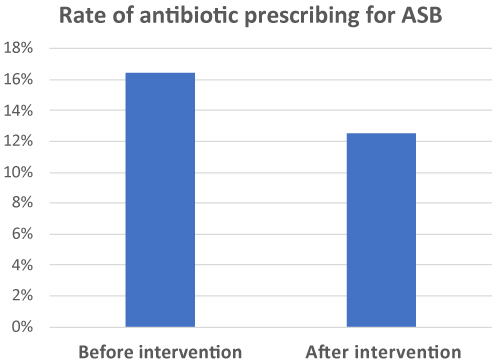 Figure 2: Rate of antibiotic prescribing for ASB. Retrospective chart review was used to determine the rates of antibiotic prescribing for nursing home residents with ASB before and after the educational intervention. View Figure 2
Figure 2: Rate of antibiotic prescribing for ASB. Retrospective chart review was used to determine the rates of antibiotic prescribing for nursing home residents with ASB before and after the educational intervention. View Figure 2
Thus, the rate of unnecessary antibiotic prescribing was reduced by 3.9% following implementation of the educational intervention. These data may indicate the utility of the educational interventions implemented in Butler Health System's Emergency Department for decreasing unnecessary antibiotic prescribing for nursing home residents with ASB, which may have benefit for reducing potentially harmful patient outcomes.
UTIs are the most common bacterial infection in elderly people, causing more than 50% of all infection episodes requiring treatment in the institutionalized elderly population [12]. However, ASB is also quite prevalent in this community and is commonly misdiagnosed as UTI and inappropriately treated with antibiotics. Given the prevalence of ASB in institutionalized elderly individuals, appropriate treatment is essential for delivering quality patient care. Differential diagnoses other than a UTI should be considered before antibiotic treatment is administered [12].
The data presented in the present study show that nursing home residents who come to the Butler Health System's Emergency Department frequently present with symptoms meeting the Infectious Diseases Society of America's guidelines for ASB. Patients with ASB were found to be discharged with UTIs at a relatively high rate. According to Lee, et. al., "Physicians' lack of knowledge and misperceptions contribute to the misuse of antibiotics" [2]. This suggests that increased awareness of appropriate treatment methods may improve patient outcomes and avoid the harmful consequences of unnecessary antibiotic use.
This pilot educational intervention included information on ASB management disseminated by posters, pocket cards, and a PowerPoint presentation to the Emergency Department staff at Butler Memorial Hospital. Provision of the educational intervention was associated with a 3.9% overall reduction in the rate of antibiotic prescribing among nursing home residents with ASB. These data may suggest the utility of educational interventions on ASB management for enhanced antibiotic stewardship, and this report provides important materials to enhance awareness of ASB best practices among clinical staff.
One limitation of this study is it that it was conducted in only one hospital; a multi-center design would increase the validity and generalizability of the intervention. Another limitation is the small sample size of participants. Furthermore, a randomized control trial format should be used to more robustly evaluate the efficacy of the intervention. Further research must be conducted to more accurately assess the rate of inappropriate ASB treatment in the inpatient hospital setting. The research findings were shared with Butler Health System's Infectious Disease Group and Emergency Department, and the Pennsylvania Safety Advisory Committee. These research data may be beneficial for ongoing and future antibiotic stewardship initiatives.
None.
E.K. conceived of and designed the study, performed the analysis, and wrote and revised the manuscript.
I wish to thank the Butler Health System staff for their support and contribution, including Dr. Marc Oster and Dr. John Love for their useful and constructive recommendations on this project. Special thanks should be given to Dr. Meg Larson, my research project chair for her professional guidance and valuable support and the faculty of Clarion and Edinboro Universities.