Dermatofitosis are cutaneous infections caused by fungus. They affect the keratinized surface layers epidermis, hair and nails.
We report a case of a 42-year-old female patient who presented with erythematous annular lesions with a raised edge on the chest, back, neck, hands and arms. These lesions were compatible with erythema multiforme, subacute lupus and/or ringworm infection. The biopsy of lesions was done and the study showed the structures suggestive of fungi in hematoxylin-eosin staining. They were confirmed by PAS staining, starting antifungal treatment for 4 weeks with complete resolution of lesions.
Superficial mycoses, Dermatophytes
Corporalis ringworm includes all dermatophyte infections affecting hairless skin of the trunk and extremities, except of those located in specific areas, such as palms or soles. The infection is generally limited to the stratum corneum and is seen most often in exposed areas but may occur in any location.
In the classic form of ringworm, after a period of incubation from 1 to 3 weeks, an erythematous lesion is observed, extending progressively centrifugally and results in polycyclic annular plates of various sizes with an erythematous elevated edge in which it is possible to observe vesicular or pustular lesions, and a paler center that represents the resolved infection.
Most lesions show a fine desquamation although this may be minimal or absent, especially after initial treatment with topical steroids (tinea incognito). The lesions can be single or multiple and may coalesce to form large plates [1,2].
42-year-old woman without personal history who presented to the Dermatology outpatients' clinic with erythematous lesions on the trunk and upper limb including the palms (Figure 1). The lesions were erythematous plaques with a raised edge and subtly flaking center, without signs of superinfection on the back of the upper limbs or trunk and erythematous macules on the palms (Figure 2).
 Figure 1: Erythematous Lesions on the Trunk and Upper Limb Including the Palms. View Figure 1
Figure 1: Erythematous Lesions on the Trunk and Upper Limb Including the Palms. View Figure 1
 Figure 2: The lesions were erythematous plaques with a raised edge and subtly flaking center, without signs of Super infection on the back of the upper limbs or trunk and erythematous macules on the palms. View Figure 2
Figure 2: The lesions were erythematous plaques with a raised edge and subtly flaking center, without signs of Super infection on the back of the upper limbs or trunk and erythematous macules on the palms. View Figure 2
Two days before, she had attended the emergency center for the same reason, where she was prescribed corticosteroids and antihistamines.
We performed a supraclavicular injured skin biopsy and with blood count analysis, biochemistry, ANA, IgE, PCR and HIV, mycoplasma, herpes simplex, cytomegalovirus, liver and syphilis serologies.
We included in the differential diagnosis: dermatofitosis (erythematous scaly papules with active edges), erythema multiforme (dianiformes edematous lesions) and subacute cutaneous lupus (annular papulosquamous lesions located in photoexposed areas) [3].
The analytical results were within normal limits and the histopathology study with hematoxylin-eosin showed foci of papillary edema and lymphoid infiltrate in dermis. In the stratum corneum, structures suggestive of fungi were evident, confirmed by the presence of fungal spores in PAS technique (Figure 3).
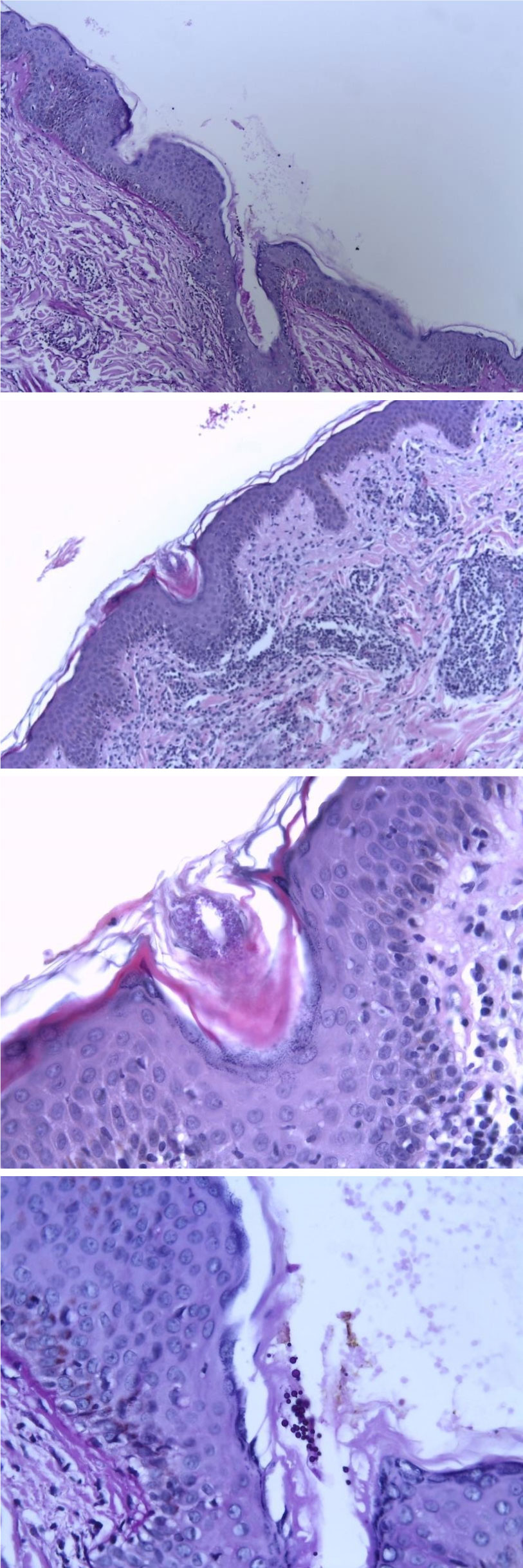 Figure 3: In the stratum corneum, structures suggestive of fungi were evident, confirmed by the presence of fungal spores in PAS technique. View Figure 3
Figure 3: In the stratum corneum, structures suggestive of fungi were evident, confirmed by the presence of fungal spores in PAS technique. View Figure 3
We prescribed Itraconazole orally for 4 weeks, and reviewed within 45 days. In the follow-up, the lesions had completely disappeared.
Dermatofitosis is a skin infection that is caused by fungi. The most frequent etiologic agent in children is M. canis and in adults, T. rubrum and T. mentagrophytes interdigitale variety.
The rash begins as a small area of red, raised spots and pimples and slowly becomes an erythematous annular lesion, single or multiple, with an edge with vesicles or crusts and centrifugal growth and healthy skin in the middle.
The most common predisposing factor in our environment for tinea corporis is excessive perspiration. Other important factors are the use of occlusive clothing, contact sports such as rugby, football or wrestling, and of course the patient's immune response. Described chronic or dermatophyte infections very extensive in HIV patients with chronic mucocutaneous candidiasis, in steroid treatment, or undergoing bone marrow transplantation [1-3].
If only one or two lesions exist, topical antifungal therapy is sufficient. Antifungal medication may be given as a pill for extensive infections or infections in people with weakened immune systems. Examples of oral medications for ringworm include itraconazole, terbinafine, fluconazole and griseofulvin.
In our case the patient had extensive infections and we considered an oral treatment. The lesions disappeared in about 3 weeks [4,5].
Sometimes, different skin lesions manifest similarly, requiring histological study to establish a definitive diagnosis.