This commentary provides a detailed examination of the interplay between climate change, vector-borne diseases (VBDs), and conflict within fragile and conflict-affected states (FCS). It identifies how climate change intensifies existing vulnerabilities by altering the conditions favorable to disease vectors, which exacerbates public health crises in regions already destabilized by conflict. This analysis highlights the profound multiplier effect of climate change on VBD transmission through ecological changes that expand vector habitats and alter their breeding patterns, leading to increased disease outbreaks in environments with compromised healthcare infrastructures. Further explored are the socioeconomic impacts of these health crises, which perpetuate cycles of poverty and impede sustainable development, thereby challenging the efficacy of international aid and governance in these regions. The commentary argues that the compounded challenges of climate change, health vulnerabilities, and conflict necessitate integrated policy responses. It recommends the development of resilient health systems, robust disease surveillance, and control mechanisms, and the inclusion of health imperatives in climate adaptation strategies to effectively address the interconnected threats. Additionally, the paper calls for improved governance structures to ensure the successful implementation of public health interventions and to facilitate international cooperation. By providing a comprehensive overview and actionable recommendations, this commentary aims to inform policymakers and international agencies about the critical need for coordinated efforts to mitigate the impacts of these interlinked challenges and to enhance the resilience of vulnerable communities in FCS.
Climate change is one of the most significant challenges of the 21 st century with major implication for public health [1]. Numerous studies have shown how climate change impacts human health through a variety of environmental transformations [1-4]. These include deforestation, which alters natural habitats and increases interactions between humans and disease vectors; emissions of greenhouse gases that intensify global warming; industrial activities and changes in land use that impair natural ecosystems; the combustion of fossil fuels, resulting in air pollution; and the depletion of the ozone layer, which enhances exposure to damaging ultraviolet radiation. Collectively, these factors create a complex web of health vulnerabilities [1].
According to the World Health Organization (WHO), vector-borne diseases (VBDs) account for more than one-sixth of all illnesses and disabilities globally [1]. A growing portion of the world's population is at risk due to these diseases, exacerbated by climate change and its impact on the environment [2]. Vectors, primarily arthropods like mosquitoes and ticks, are important in the transmission of these diseases [1]. They act as carriers, transmitting pathogens from an infected host (human or animal) to an uninfected individual [1]. The mode of transmission of VBDs varies and can be vertical, horizontal, or mechanical [2]. Vertical transmission (VT) occurs when a pathogen is passed from parent to offspring (transgenerational transmission) or persists between different stages of an arthropod’s development (transstadial transmission). In VT, the pathogen typically enters the ovarian germinal tissue and then spreads transcardially to subsequent reproductive or blood-feeding stages, with transgenerational transmission occurring through the ovaries [1]. Horizontal transmission involves the transfer of diseases from vectors to vertebrate hosts through bites or direct contact with infected vector excrement. For instance, Aedes mosquitoes carry the dengue virus, black-legged ticks transmit Lyme disease, and female Anopheles mosquitoes transmit Plasmodium parasites, causing malaria [2]. Furthermore, mechanical transmission occurs when vectors physically transfer pathogens from infected to uninfected hosts. Unlike other modes of transmission, this process does not involve pathogen growth or reproduction within the vector. Houseflies ( Musca domestica ) are significant mechanical vectors responsible for transmitting bacterial and viral pathogens, including diseases like diarrhea and conjunctivitis [1,2].
Fragile and conflict-affected states (FCS) are countries or territories plagued by institutional and social instability and often violent conflict. The World Bank's Fragile, Conflict, and Violence group categorizes these states based on their financial and security situations, publishing an annual list since 2006 [3]. The latest version includes twenty countries marked by high levels of institutional and social fragility and nineteen countries experiencing violent conflict, as illustrated in Figure 1 [4,5]. Globally, one-fifth of countries fall into the FCS category, encompassing nearly 1 billion people and 43 percent of the global poor [3,4]. Conflict not only escalates climate vulnerability and vector-borne diseases (VBDs) but also amplifies their detrimental effects on populations and economies [1-4].
 Figure 1: List of Fragile and Conflict Affected States (FCAS), 2024 [4,5].
View Figure 1
Figure 1: List of Fragile and Conflict Affected States (FCAS), 2024 [4,5].
View Figure 1
In conflict-affected states, VBDs pose a significant health risk and cause widespread socioeconomic disruption [3,4]. The impact of VBDs is intensified by limited funding for critical infrastructure like secure housing and sufficient drainage systems, essential for mitigating climate-related challenges [3,4]. Additionally, poor governance in these regions reduces resilience to climate shocks and complicates efforts to secure international aid, thereby increasing disease incidence [3,4]. This governance deficiency exacerbates health risks, as public health systems are often underfunded and ill-equipped to manage or control outbreaks of diseases such as malaria, dengue, and Zika [3,4]. The interplay of political instability, inadequate infrastructure, and climatic adversity creates a complex environment conducive to the rampant spread of VBDs [3,4]. Consequently, residents of these states face increased vulnerability to diseases that could otherwise be controlled with adequate resources and effective governance [3,4]. This paper explores the interconnectedness of climate change, VBDs, and conflict, offering policy recommendations to combat climate vulnerabilities and VBDs in FCS.
Climate vulnerability and VBDs exacerbates each other in FCS [1-4]. Figure 2 shows a simplified framework to illustrate this nexus. Climate change and VBDs are intricately linked, with climate change invoking various indirect effects on ecosystems [1-3]. For example, reduced rainfall can lead to water scarcity, biodiversity loss, habitat destruction, and altered reproductive patterns [1]. These changes impact vector ecologies by affecting their life cycles, breeding rates, and activity levels, which in turn increase human vulnerability to diseases [1]. Besides affecting disease vectors, climate change also influences pathogens and their hosts [1,2]. Specific humidity conditions may favor the growth of certain microbes, while temperature changes can enhance the survival and transmissibility of pathogens, with higher temperatures supporting faster pathogen replication and development [1,1]. Combination of political instability and environmental factors can lead to increased drug resistance and pose threats to individual well-being [2,3,4]. These complex interactions suggest that meteorological factors will significantly alter disease patterns, influencing the geographical distribution of most, if not all, vector-borne diseases [1,2].
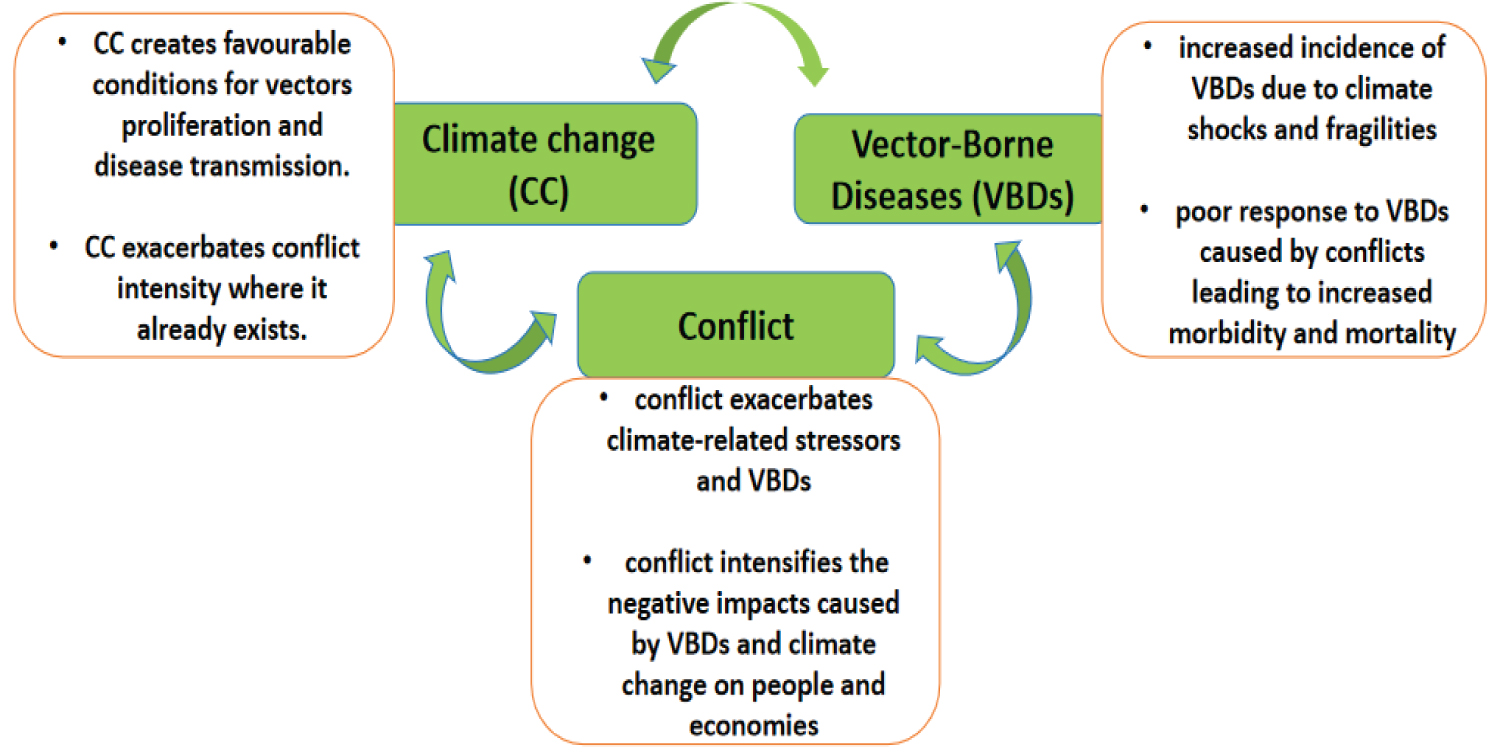 Figure 2: Climate change- Vector-Borne Diseases- Conflict Nexus.
View Figure 2
Figure 2: Climate change- Vector-Borne Diseases- Conflict Nexus.
View Figure 2
Armed conflicts have many devastating consequences and one of the most immediate is the weakening of health systems [6,7]. Healthcare facilities are damaged, healthcare workers (HCWs) are displaced, and public health services like supply chains for essential medicines are disrupted [6,7]. This often results in a drastic reduction in healthcare access for the affected population [6,7]. Conflict increases exposure to health risks like new infections and vectors as people may go untreated or seek care from unregulated sources thereby increasing the risk of untreated vector-borne diseases [6,7]. Additionally, the affected population often lives in crowded areas with poor sanitation further exacerbating the spread of vector-borne diseases [6,7]. Access to clean water, adequate sanitation facilities, and accommodation end up limited thereby creating ideal conditions for disease transmission [6,7]. Disease surveillance and control programs are essential for monitoring disease outbreaks and carrying out preventive measures [6]. However, in conflict-affected states, control programs for diseases like guinea worm, river blindness, and polio are often disrupted resulting decline in vaccination coverage which leaves populations vulnerable to vaccine-preventable diseases [8,9]. Disruption in vector control measures like insecticide spraying and mosquito net distribution leads to unchecked proliferation of vector populations [6]. Additionally, resources and personnel are often redirected to address immediate humanitarian needs, which often results in a breakdown in surveillance efforts [6]. Owing to this, disease transmission can go undetected thereby leading to larger outbreaks and increased morbidity and mortality. This was seen in the earthquake in Haiti in 2010 where the identification of the emergence of cholera took several days [10].
Climate change is associated with decreased air quality which can result in a subsequent rise in mosquito reproduction, parasite development, and bite frequencies thereby making vector-borne diseases like malaria, tick-borne illnesses, and dengue fever more widespread [1-4]. This is further exacerbated in zones/regions of conflict [3,6,7,11]. Displacement of populations, destruction of infrastructure, and alteration in ecology can bring about new breeding grounds for vectors and disrupt their natural habitats [11]. Between 1999-2000, a tularemia outbreak was reported during the civil war in Kosovo due to ecological changes, huge population movements, and deterioration of sanitation [12]. Population displacement can facilitate the transmission of vectors and contact with infectious agents both for the migrating population and for the population at the destination [11].
Climate vulnerability worsens temperature change and precipitation patterns, decreasing air quality thereby expanding the geographical range of disease vectors and increasing the frequency and severity of disease outbreaks [1,2]. However, the core manifestations of these diseases and climate change impacts can differ between regions [1,2,13]. Malaria, for example, remains a major health concern in conflict-affected regions of sub-Saharan Africa, however, dengue fever shows more prevalence in Southeast Asia and Latin America [13]. In a study by Stensgaard, et al. it was predicted that a significant decrease of Schistosoma mansoni in west and central Africa will occur by 2080, with increase in eastern and southern Africa [13]. Environmental changes due to conflict such as deforestation and population displacement may have distinct consequences on disease transmission dynamics in different geographical contexts [13]. For example, deforestation tends to create favourable conditions for the growth of heliophilic malaria vectors like Anopheles gambiae in Africa however it reduces Anopheles dirus in southeast Asia which prefers forest cover [13].
Wars destroy health systems and infrastructure, curtail existing disease control programs, and cause population movement leading to an increase in exposure to health risks and favour the emergence of infectious diseases [3,6,7]. According to the World Meteorological Organization (WMO), one-third out of every 100,000 people from 73 countries in their study are not covered by multi-hazard early warning systems [14]. Donor countries in collaboration with international organizations can respond by increasing funding to initiatives to build state-of-the-art early-warning and advisory systems in the most vulnerable countries, especially Small Island Developing States (SIDS) and African countries that have the weakest early warning systems [15]. Integration of climate change considerations into public health policies is essential now more than ever. The WHO called the Paris Agreement “a fundamental public health agreement” and major reports such as the Lancet Countdown: Tracking Progress on Health and Climate Change have made clear the central role of the health field in both identifying and communicating economic health “co-benefits” from reduce greenhouse gases and contributing to the widespread need to target vulnerability and build local resilience. Climate and non-climate actors, development partners, governments, and donors must prioritise climate-friendly policies, commit to preventive measures to save lives, and reduce image footprint globally. It is important for governments to develop and implement education and public awareness programs on climate change and its effects, to ensure that the public has access to information, and to encourage public participation in finding and implementing solutions.
The nexus between climate change and the surge of vector-borne diseases in conflict-affected states underscores the urgent need for comprehensive strategies. Vulnerable communities are at greater risk of acquiring diseases due to the disruption of healthcare infrastructure, exacerbation of environmental degradation, and population displacement during conflict. Through the implementation of targeted interventions, strengthening healthcare infrastructure, and building community resilience, the impact of climate change on disease dynamics in conflict areas can be lessened. Furthermore, encouraging sustainable development and tackling the underlying drivers of conflict can lay the groundwork for long-term resilience. By working together, we can protect public health and increase adaptive capacity, making conflict-affected governments more prepared to handle the twin challenges of vector-borne diseases and climate change.
None.
The authors declared no competing interests.
The authors wish to thank Pharma Incubation Hub for training and mentoring undergraduate pharmacy students in Africa in research and capacity building.
Adeniyi Ayinde Abdulwahab and Yusuff Adebayo Adebisi concveived the idea. Adeniyi Ayinde Abdulwahab, Yusuff Adebayo Adebisi, Ashiru Mustapha Adeniyi, Taiwo Olawehinmi, Omotayo Faith Olanrewaju, Agwuna Favour Obianuju, and Ibrahim Abdulmumin Damilola wrote the initial draft. Adeniyi Ayinde Abdulwahab and Yusuff Adebayo Adebisi reviewed and revised the manuscript. Adeniyi Ayinde Abdulwahab prepared the manuscript for publication.