Background: To determine link between sarcopenic obesity and osteoporosis and fall risk.
Methods: Systematic review and meta-analysis based on PRISMA Statement was made on studies acquired from PubMed, Science Direct, EBSCOHost, and ClinicalKey using certain keywords and criteria. Included studies were further assessed for quality and risk of bias and included for qualitative and quantitative analysis.
Results: There was no significant relationship between sarcopenic obese patient and risk of osteoporosis. However, there was an increased number of risk of fall in sarcopenic obese patient (RR 2.61; 95% CI 1.76-3.85). Same pattern was observed in risk of fracture (RR 1.38; 95% CI 1.02-1.88). We found out that osteoporosis and sarcopenia altogether bring their respective risk and protective factors towards bone mineral density, thus relation towards osteoporosis yet to be determined. However, they are prone to gait instability and give bigger impact when they fall, thus increasing risk of fall and fracture.
Conclusions: Sarcopenic obese patients should be accounted into comprehensive healthcare to improve quality of life by reducing its morbidity.
Fall, Fracture, Obesity, Osteoporosis, Sarcopenia
Sarcopenia is a clinical condition where skeletal muscle deteriorate within mass and function. The International Working Group on Sarcopenia (IWGS) defined sarcopenia as presence of low skeletal muscle mass and low muscle function which related towards walking speed. It was initially linked with elderly, though recently it is known not exclusive towards elderly. Sarcopenia is highly related with morbidity due to less quality of life, and mortality. Sarcopenia is seen in 14% of elderly aged between 65 and 70 years old, and 53% of elderly aged above 80 years. These statistics have contributed to increased cost and burden of health care, contributing to approximately 18,500,000,000 GBP of direct health care cost in The United States [1].
Besides sarcopenia, obesity is a condition which is emerging on elderly. Study on The United States and Malaysia found that approximately 30% of elderly aged 60 years and above were obese. In addition, one third of them were having hypertension and/or diabetes. Moreover, obesity was highly linked with improved risk of mortality in elderly. Therefore, obesity should be taken into account when assessing an elderly patient which seems overly sized in stature in-order to tackle future morbidity and mortality [2-3].
Sarcopenia is occasionally presented alongside with obesity, known as sarcopenic obesity which provide double burden for the patient, especially for elderly aged over 65 years old which contributes 13% to our demographic chart. Sarcopenic obesity is best explained with biological measure. Aging is related with change of body composition which could be seen in improvement of body fat until seventh decade of life and reduction of it afterwards, vertebral compression, and reduction of muscle mass after fourth decade of life. In addition, basal metabolism is also reduced, thus related towards reduced mitochondrial volume and oxidative capacity. Reduced basal metabolism rate is correlated with muscle mass loss, but not with reduction of appetite. Therefore, sarcopenic obesity could occur. Another biological mechanism discuss oestrogen and testosterone as contributing factors. Reduction of testosterone and oestrogen in elderly contribute negatively to muscle mass and fat distribution. In addition, menopause in women increase body weight and fat mass, but decrease fat-free mass. Elderly also associated with elevated cytokine levels which leads to insulin resistance by muscle catabolism. Such mechanism would promote improvement of fat mass and reduction of muscle mass. In addition, elderly are prone to developing anabolic resistance due to less availability of post-prandial amino acid, low muscle perfusion, and less capacity of digestive tract as result of splanchnic sequestration of amino acid [4].
Sarcopenic obesity is largely associated with disability. It was known that people with sarcopenic obesity had 2.5 folds of eight-year disability risk compared to people who do not. In addition, it was known that sarcopenic obesity increase risk of hospitalization. Sarcopenic obesity was also linked with improved risk of insulin resistance, metabolic syndrome, dyslipidemia, and vitamin D deficiency. In terms of longer prognosis, sarcopenic obesity was at 1.72 folds risk of mortality more than control. Same study shown that lower performance status and ability contributed towards improved risk of mortality. Mortality on sarcopenic obesity was also correlated with other confounding diseases, such as cardiovascular disease, Cerebrovascular disease, and other non-communicable disease that could resulted by disabilities caused by sarcopenic obesity [5]. Another study suggest that sarcopenic obesity was found in 4% of women and 11% of men in study population, with 3.25 folds risk of dying more than they who did not have it [6]. Therefore, sarcopenic obesity has provide a lot of burden towards society, especially elderly and their caregivers in terms of spending, time, and health.
Sarcopenic obesity was also suspected as contributors towards osteoporosis and fall in elderly. A study shown that even though obesity could be a protective factor of osteoporosis in elderly, sarcopenia contributed 2.81 and 2.75 fold risk more towards osteoporosis in spine and femur, respectively [7]. In another study, sarcopenia was linked to improved risk of osteoporosis by 1.87 times and 3.89 times in women and men, respectively [8]. Other study also mentioned that patient with both sarcopenia and obesity experienced lower-leg muscle density and lower balance path leg, both on men and women. Same study also mentioned lower bone mineral density in patient with sarcopenic obesity [9]. Another study found that people with sarcopenia and obesity experienced 1.35 folds and 1.21 folds increased risk of falling in age group 50 to 64 years old and 65 to 79 years old respectively [10]. In-order to determine clear relationship between sarcopenic obesity and risk of osteoporosis and fall, authors conducted a systematic review and meta-analysis on population with sarcopenic obesity.
Authors conducted a systematic review with meta-analysis adhering to Preferred Items for Systematic Reviews and Meta-analysis (PRISMA) statement [11]. This study has been registered in PROSPERO with registration number of CRD42021248063. Authors conducted searching using specific keywords on four databases: PubMed, Science Direct, EBSCOHost, and Clinical Key. Authors used keyword of "Sarcopenia"[Mesh] AND "Obesity"[Mesh] AND ("Osteoporosis"[Mesh] OR "fall") on PubMed, ("sarcopenia" OR "sarcopenic" OR "sarcopenias") AND ("obesity" OR "obese") AND {("osteoporosis" OR "osteoporoses" OR "bone loss") OR ("fall")} on Science Direct due to limitation of Boolean operator, and ("sarcopenia" OR "sarcopenic" OR "sarcopenias") AND ("obesity" OR "obese" OR "obesed") AND {("osteoporosis" OR "osteoporoses" OR "bone loss") OR ("fall")}on the rest of databases. Searching was done at 5 April 2021 on PubMed and 8 April 2021 on other databases.
Authors set inclusion criteria as follows: 1) Clinical trial; 2) Studying population with sarcopenic obesity as independent variable; 3) Studying osteoporosis and/or fall risk as dependent variable; 4) Involving normal (not sarcopenic nor obese) populations as control; 5) Done in community and/or clinical settings. In addition, authors set exclusion criteria as follows: 1) Studies written in language other than English/Bahasa; 2) Review. Searching and assessment were done by seven authors (LIO, ADS, MP, BPPS, RH, AA, TK) with any discrepancies within authors discussed further for solution and coherency.
Studies which passed eligibility criteria further assessed for their quality. All studies were appraised with critical appraisal tools by Oxford Center for Evidence-based Medicine for study quality [12]. In addition, risk of bias of each study was assessed using Cochrane Tool for Risk of Bias if there are randomized study in our study [13]. Assessment with both tools were done by seven authors (LIO, ADS, MP, BPPS, RH, AA, TK). Any discrepancies met were discussed for clearer and unified outcome.
Studies were extracted for further review. Characteristics extracted such as: 1) Author and year of publication; 2) Study location; 3) Study design; 4) Number of samples involved; 5) Study period; 6) Gender; 7) Age; 8) Osteoporosis profile; 9) Fall risk profile. These data were taken for qualitative and quantitative analysis. Quantitative analysis was done using OpenMeta from Brown University Evidence-based Practice Center [14]. Authors conducted single-arm meta-analysis to determine impact of sarcopenic obesity towards two variables: 1) Osteoporosis; 2) Fall risk. Both calculations were done using dichotomous data.
Heterogeneity was first assessed using Cochrane's Q-statistic with chi-square test and Higgins' I2 statistic test. Based on Cochrane Handbook, P-value of < 0.1 considered as statistical heterogeneity and I2 > 50% considered as statistical heterogeneity. In advance, heterogeneous data were pooled using random-effect model, otherwise homogenous data were pooled using fixed-effect model [15].
Searching was conducted alongside with the searching strategy, deriving nine studies to be appraised and synthesized (Figure 1) [7,10,16-22]. Included studies were done between 2008 and 2018 on various countries in Asia, Australia, Europe, and America. All studies were either cross-sectional or prospective cohort, except one randomized controlled trial (RCT) study. Our study involved 16,575 subjects with variety of age (Table 1). Qualitative assessment of studies shown good results on all studies, expect unclear completion follow-up of several studies as the result of case-control design (Table 2) [7-10,16,21]. Risk of bias assessment on RCT by Waters, et al. shown that the study was free of bias risk (Table 3) [13,22].
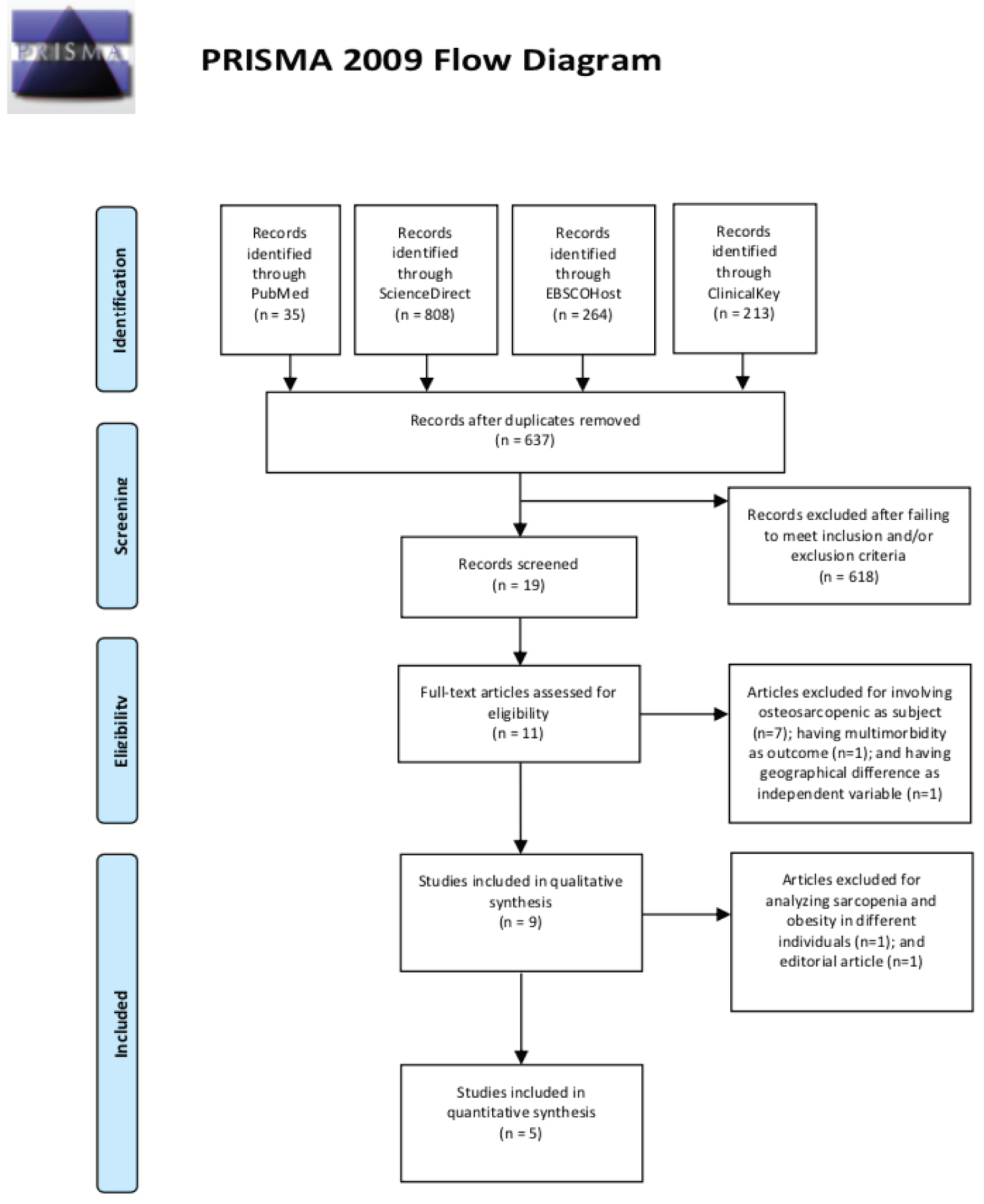 Figure 1: Searching strategy conducted by authors [11].
View Figure 1
Figure 1: Searching strategy conducted by authors [11].
View Figure 1
Table 1: Characteristics of included studies [7,10,16-22]. View Table 1
Table 2: Quality assessment of included studies [7,10,16-22]. View Table 2
Table 3: Risk of bias assessment of selected study [13,22]. View Table 3
There are six studies reporting impact of sarcopenic obesity towards osteoporosis (Table 4) [7,10,16-22]. Out of six studies, one stated significancy of sarcopenic obesity towards osteoporosis risk, whilst another one stated its insignificancy [7,18]. In terms of bone mineral density (BMD), there were two studies stated higher BMD in control group, but deemed insignificant [7,17]. Another study suggest lower spine and total body BMD in sarcopenic obesity group [23]. In terms of fracture risk, there were two significant studies suggesting higher fracture risk in sarcopenic obesity compare to the control group [20,21]. Another study found greater femur neck fracture incidence compared to control or obese, but less to sarcopenic group [22].
Table 4: Results of included studies [7,10,16-22]. View Table 4
Quantitative analyses using meta-analysis were done in two aspects: osteoporosis risk and fracture risk. In terms of osteoporosis risk, authors involved two studies with heterogeneously distributed data (I2 > 50%). Based on random effect model, it was known that osteoporosis risk was insignificantly higher in sarcopenic group compared to control group (RR 3.89; 95% CI 0.907-16.729) [7,14,18]. However, significant relationship was found between sarcopenic obesity and fracture risk. Based on homogenous data and fixed effect model (I2 < 50%), there was higher risk of fracture compared to the control group (RR 2.61; 95% CI 1.762-3.854) [14,20,21]. Therefore, it could be summed up that sarcopenic obesity was not significantly related towards risk of osteoporosis, but significantly related towards fracture risk (Table 5, Figure 2).
There are six studies discussing impact of sarcopenic obesity towards fall risk (Table 4)[10,16,19-22] Fall risk was assessed through variety of tools and units. A study reported insignificant difference on The Activities-specific Balance Confidence Score (ABC) and Fall Efficacy Score International (FES-I) [16]. Another one reported insignificant difference of Tinneti score and Time Up and Go Test (TUGT) score between both groups [19]. Another studies suggested insignificant difference of fall risk and fall incidence per year between groups [20,22]. Out of all studies, there were two studies eligible for meta-analysis. Authors found out that the data were spread heterogeneously, thus random effect model was used. It was known that fall risk was significantly higher in sarcopenic obesity group compared to control group (RR 1.38; 95% CI 1.018-1.878) [10,14,20]. Therefore, it could be concluded that sarcopenic obesity was significantly related towards fall risk (Table 5, Figure 2).
Based on quality assessment, all studies met the standard and considered to be in a good quality. Hence, there is no issue on quality. Even though there was an evidence of lower spine and total body bone mineral density (BMD) in patients with sarcopenic obesity, our meta-analysis shown that there was insignificant correlation between sarcopenic obesity and risk of osteoporosis (RR 3.89; 95% CI 0.907-16.729) [7,18-21]. This was suggestibly accounted towards lean body mass. BMD is influenced by lean mass, hence such conditions as aggravation of body weight and sarcopenia are highly related into less BMD. In patient with sarcopenic obesity, BMD is influenced not by sarcopenia, but also obesity. Sarcopenia alters bone metabolism, thus reduce BMD, but obesity also plays an important role in such paradoxical protective mechanism [7]. Lately obesity has been accounted for bone strength, called as "obesity paradox" or "reverse epidemiology". A study found that obesity and overweight were significantly correlated with better BMD and less risk of osteoporosis (RR 0.26; 95% CI 0.11-0.64) [23]. This phenomenon best explained by better weight-bearing effect [24]. However, it was known that obesity and fat deposition in the body cause alteration of bone structure due to disruption of bone-regulating hormones, elevation of oxidative stress, improved inflammation which could disrupt bone metabolism [25]. Those were why other two studies were inconsistent on their finding of sarcopenic obesity towards BMD and osteoporosis [7,17].
In terms of fracture risk, our meta-analysis found out that there was significantly elevated risk of fractures in patient with sarcopenic obesity (RR 2.61; 95% CI 1.762-3.854) [20,21]. This was accounted to controversial role of body mass index towards bone health, as stated by paragraph above. From the meta-analysis, we could consider that body mass could give positive and negative contributions towards bone health, but could not damper adverse event of having big body mass itself. It will be discussed further that sarcopenic obesity patients were prone to fall, which could increase risk of fracture [10,20]. Even though that more body mass means more shock absorption during fall, it still means that there are more instability, leading to falls. It was also known that body mass contributes to force applied to the body when it was coming to fall [20]. However, authors suspected the impact of body mass towards bone health and fracture risk were gender-related. It was figured out that sarcopenic obese women have more compact BMD compared to the control group, whilst sarcopenic obese men have roughly insignificant difference of BMD compared to the control group. This phenomenon was accounted for oestrogen level on fat mass of women, which contributes to activity of osteoblast and osteoclasts in forming the bone, thus maintaining bone health [21].
In terms of fall risk, our quantitative analysis shown that people with sarcopenic obesity have a greater tendency of falling compared to the one who do not (RR 1.38; 95% CI 1.018-1.878) [10,20]. This phenomenon was accounted to double impact of sarcopenia and obesity. It was known that sarcopenia could alter mass structure, thus create environment of instability for its patients. This was added up by obesity which caused gait disturbance [10,20]. A study shown that BMI, waist circumference, and waist-to-height ratio significantly correlated with gait instability in the elderly [26]. On the other hand, sarcopenia contributed towards walking instability and neuromuscular disorders, which altogether increase fall risk, especially in the elderly [27]. These double phenomenon should be taken into account when managing elderly with sarcopenic obesity, especially with elevated risk of fracture and proneness towards osteoporosis.
This study is a pilot-review made to determine relationship of sarcopenic obesity towards frailty of the patients, especially on risk of osteoporosis and fall. This study expected to give us broad information on what to expect and how to manage patients with sarcopenic obesity. However, this study is limited to its general sample. Recent finding shown that outcomes of sarcopenic obesity are gender-related. However, such studies available to be synthesized into a review are doubtfully adequate. Thus, we recommend researchers to done more specific trials to improve outcome of further more specific review.
Sarcopenic obesity could occur in every people, especially on later age. Patients with sarcopenic obesity were subject to improved risk of fall and fracture, yet osteoporosis has not been significantly determined. Therefore, early diagnosis and prompt treatment from physician and caregiver should be conducted in a strict and disciplined fashion to ensure that quality of life of patients living with sarcopenic obesity was reserved, in order to reduce morbidity and mortality of it.
Authors stated there was no conflict of interest on the production of this study.
Authors stated there was no funding on this research.
None.
All authors have contributed equally.