Initial reports of COVID-19 infection suggested certain populations were at high risk if infected, yet it was unclear how best to identify, triage and treat those patients.
COVID-19 is a novel virus initially reported from Wuhan, Hubei province in December 2019 that has spread globally. As the virus spread, clinicians were trying to assess the populations at risk, how to treat and follow best practice guidelines as they were evolving. We sought to examine our community hospital experience, identify predictors of mortality and establish guidelines that would help the system in the future including EVALUATION of service line effectiveness for those high-risk populations, and how COVID-19 impacted our Family Practice training program.
Patients admitted from March 2020 through June 2020 who were COVID-19 (+) were identified and their charts retrospectively reviewed for demographics, symptoms, past medical history, pre-treatment medications, EKG, laboratory values including cardiac and inflammatory biomarkers, in-hospital treatment, length of stay, cardiac events, use of ventilator, or clotting disturbance. Data were analyzed in 2 groups, those who survived hospitalization vs. those who died. Frequency analysis was reported for categorical variables and means ± standard deviations (SD) reported for continuous variables.The Fisher's exact test was performed for categorical values, t-test for continuous variables (significance p < 0.05). Variables with p < 0.05 were entered into univariate analysis but all variables were then analyzed via multivariate logistic regression in the python stats model for generalized linear models for predictors of mortality.
A total of 538 patients were admitted, 49.8% were female, most 52.6% were Caucasian with 30% Hispanic. The average age was 65.5 ± 19.6 years, and those who died were older 79 ± 13 years (p < 0.00001). Mortality for the entire cohort was 17.1%. When analyzed by age, mortality was 3.5% for age < 60, if over 60, it was 24.7% and if over age 80, mortality was 30.7%. Patients admitted from a long-term care facility had a mortality rate of 31.6%, and if over aged 80 the mortality rate was 35.1%, making long-term care residents over 80 the most vulnerable population affected.
Univariate analysis revealed Caucasian, age > 80, admission from a long-term care facility, symptom of altered mental status, history of arrythmia, peripheral vascular disease, hypertension, hyperlipidemia, smoker, known COPD, prior CVA or history of dementia, pre-treatment with antivirals before admission, abnormal EKG, NT-ProBNP, hs-troponin I or any complications, especially use of vasopressors were associated with increased mortality. Multivariate logistic regression found age, non-independent living, abnormal glomerular filtration rate (GFR), abnormal LDH, ventilator use, clotting disorder, history of hyperlipidemia, or treatment with remdesivir were predictors of mortality.
The most vulnerable population affected by COVID-19 infection are those from long term care facilities, over the age of 80 with significant co-morbidities, and who have baseline laboratory abnormalities. These factors should be considered to triage and care for these patients more effectively. Palliative care services need to be involved to help with difficult decisions early in the hospitalization. Working with long-term care facilities to decrease the spread is an important public health initiative for Lee County.
Covid-19, Elderly, Mortality, Risk factors, Palliative care
COPD: Chronic Obstructive Lung Disease; ARDS: Acute Respiratory Distress Syndrome; ICU: Intensive Care Unit; ACE/ARB: Angiotensin Converting Enzyme, Angiotensin Receptor Blockade; SWF: South West Florida; BMI: Body Mass Index; EKG: Electrocardiogram; CDC: Centers for Disease Prevention and Control; HFpEF/ HFrEF: Heart Failure with Preserved of Reduced Ejection Fraction; CVA: Cerebrovascular Accident; MACE: Major Cardiac Adverse Event; LOS: Length of Stay; MRI: Magnetic Resonance Imaging; OR: Odds Ratio; RNA: Ribonucleic Acid; FDA: Food and Drug Administration; DNA: Do Not Resuscitate; ER: Emergency Room; CRP: C Reactive Protein; ESR: Erythrocyte Sedimentation Rate; LD: Lactate Dehydrogenase; PT/PTT: Prothrombin Time/Partial Thromboplastin Time; PPE: Personal Protective Equipment; PGY: Post Graduate Year
COVID-19 is a novel coronavirus initially reported from Wuhan, Hubei province in December 2019 that has rapidly spread globally [1]. As of January 1, 2021, 84 million people world-wide have been affected with 1.8 million deaths and the spread continues [2].
The World Health Organization (WHO) has designated this a pandemic [3] and health care providers, epidemiologists and government officials are continually assessing public health issues and strategies for treatment and containment. There have been a number of reports from other countries with early cases detailing many of the clinical scenarios the virus causes. Most of the reports suggest respiratory symptoms with fever, cough, dyspnea, and headache predominating that has, in many cases progressed to severe alveolar damage requiring mechanical ventilation [4]. The elderly and those with significant co-morbidities, especially cardiac disease seem most at risk. In particular, Chinese patients over the age of 80 infected with COVID-19 had a 14.8% mortality rate compared to 2.3% under age 80. The co-morbidities that present the highest risk to the patients with COVID-19 include cancer (fatality 5.6%), hypertension (6%), COPD (6.3%), diabetes (7.3%) and cardiovascular disease (10.5%) [5]. As the COVID-19 pandemic began, little data was available for review, and a multitude of papers were published in real time to guide responses to the disease as the virus spread [6].
Evolving evidence for treatment was published without the usual rigorous peer review process thus requiring providers on the front lines to rapidly assess available data and adjust treatment as appropriate [7]. Located in Southwest Florida, Lee County is the eighth largest county (population 770,577) with 29.2% of the population greater than age 65 [8]. This study sought to identify the variables that would put the hospitalized elderly of Lee County at greater risk for adverse events due to COVID-19 infection. The demographics of all patients hospitalized were compared to identify contributing variables to predict mortality and suggest possible improvements and a coherent strategy for future care of these patients. This study also sought to examine how the pandemic affected the Florida State University Family Practice residency program and service lines specifically designed to address elderly care, especially palliative and Q-life services.
This was a retrospective review of all patients over age 18 found to be COVID-19 (+) who were admitted to any of the four Lee Health acute care hospitals from March through June of 2020. The study was approved by the Lee Health Institutional Review Board. Data collected included demographics, age, race, body mass index (BMI), symptoms, past medical history, prior cardiac disease, medications, therapeutics, laboratory data, EKG and other cardiac testing, radiology, length of stay, and adverse events. Data was retrieved from the electronic medical records EPIC system (Verona, WI). As part of a quality initiative, the data was to be used to develop an algorithm based on results to triage those at higher risk of adverse events or death for better outcomes in the future. Additionally, data were collected relating to home conditions prior to admission (independent living, assisted living, nursing home or hospice) to ascertain if different services were needed for these patients.
Patients admitted for presumed COVID-19 without a subsequent (+) test were not included in the analysis. Although individual data by hospital was available to the health system for internal review, results are presented in aggregate. This paper describes a large community hospital system's experience with COVID-19 with particular attention to the demographics and contributors for adverse events compared to the rest of the hospitalized cohort. Because of the demographics of Lee County and concern for the elderly in the pandemic, we analyzed our data in terms of mortality after a COVID (+) patient was admitted
Statistical analysis was performed by the Heart and Vascular Institute, and Lee Health's statistical advisors. Categorical variables were reported as frequency analysis (percentages) with mean ± standard deviation (SD) for continuous variables. Continuous variables (laboratory values) were expressed as normal or abnormal based on our laboratories standard. We did not seek degrees of abnormality but used absolute cutoffs for these variables for ease of interpretation. The cohort was analyzed with two group comparison (deceased versus survivors).
Comparisons were determined by Fisher's Exact test for categorical variables and Student's t-test for continuous variables with a significance level of 0.05 (two-tailed). The variables with statistical significance were selected for univariate logistic regression, which was performed to explore the association of variables and risk for death. Additionally, multivariate logistic regression was performed to examine a series of predictor variables to determine those that best predicted mortality. Multicollinearity was assessed using a correlation matrix and variance inflation factor (VIF), and then the identified multicollinear variables were removed from the multivariate logistic regression model. All analyses utilized the Python Scipy-Stats and StatsModels generalized linear model packages.
From March 7, 2020 when the first COVID-19 patient was identified within the Lee Health system through June 2020, a total of 538 COVID-19 (+) cases were admitted. Figure 1 displays the monthly case admissions and mortality.
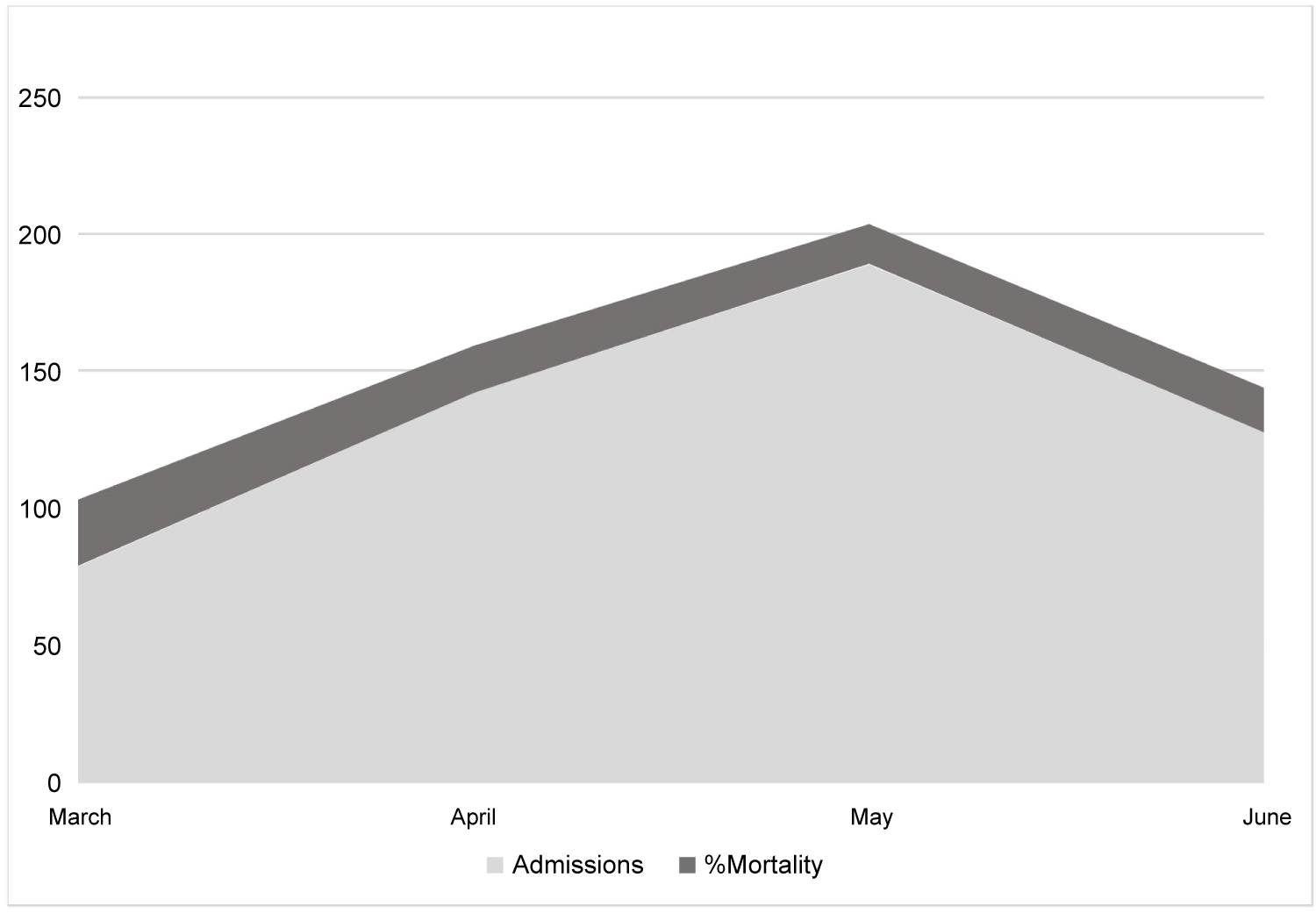 Figure 1: Monthly COVID-19 admissions with % mortality depicted in dark gray.
View Figure 1
Figure 1: Monthly COVID-19 admissions with % mortality depicted in dark gray.
View Figure 1
Table 1 displays the demographics and clinical presentation of the entire cohort. The majority of patients were Caucasian (52.6%), with the next most common ethnic group being Hispanics (30%). Most of patients were over age 60 (63.7%), and while only 7% of Lee County residents were older than 80 years of age, they represented 29% of admissions. Admissions by gender were similar with 49.8% being female, the average age was 65.6 ± 19.6 years, and 29% were over age 80. The most common co-morbidities overall were hypertension, hyperlipidemia and diabetes mellitus (58.4%, 38.8% and 32.2% respectively), with 39.8% of the group obese (BMI ≥ 30 as defined by the CDC) [9]. There was a history of cardiac disease in 26.8%, defined as prior arrhythmia requiring treatment (atrial fibrillation, supraventricular tachycardia (SVT), pacemaker or defibrillator), structural heart disease (patent foramen ovale (PFO) or atrial septal defect (ASD) requiring closure, or more than moderate valve disease in the aortic, mitral or tricuspid positions), a history of heart failure with preserved or reduced ejection fraction (HFpEF or HFrEF), peripheral vascular disease (carotid, abdominal aortic aneurysm or peripheral arterial disease) or any history of revascularization, MitraClip™, or transcatheter aortic valve replacement (TAVR). Overall, symptoms were primarily fever, chills, dyspnea or cough. Patients over the age of 80 had a higher rate of altered mental status or prior CVA compared to younger patients (29.8% less than 80, 70.2% greater than 80).
Table 1: Demographic and clinical presentation with COVID-19 patients. View Table 1
The average length of stay (LOS) for the overall group was 12.8 ± 12.26 days with 19.9% hospitalized greater than 30 days. There was no statistically significant difference between LOS in the groups that died versus those discharged (13.5 ± 11.5 Vs. 12.7 ± 12.8, p = 0.56 NS), but was significant in multivariate analysis. This could be due to the presence of interaction with other covariables affecting the multivariate regression model.
A full panel of laboratory values was not drawn on every patient due to constraints presented by the pandemic. For the total cohort, a NT-Pro BNP was collected in 49% of patients, troponin I in 23.9%, d-dimer in 84% and serum ferritin in 50.7%. Cardiac testing was not utilized as frequently as in pre-pandemic admissions due to potential exposure to personnel and the constraints of personal protective equipment. An abnormal EKG was defined as QtcF on admission > 500 ms, advanced AV block, atrial fibrillation or flutter, new ischemia, left bundle branch block, or evidence of prior myocardial infarction. Overall, 86.6% of patients had an EKG upon admission, very few had echocardiography, and none had cardiac MRI. In patients with a chest x-ray or CT scan on admission, more than 78.4% were abnormal, with no statistical significance between the 2 groups. When mortality was evaluated by age, overall mortality was 7.6% for age < 60 and 24.7% over the age of 60 with the majority of deaths being in those over aged 80 (30.7%) The living conditions played a significant role in mortality as shown in Table 2. Of those patients over the age of 80, if admitted from home, mortality was 19% but if admitted from a non-independent living situation (rehabilitation, skilled nursing, assisted living, hospice) the mortality rate was 35.1%.This also held true for patients less than aged 80.
Table 2: The effects of living conditions on mortality. View Table 2
The in-hospital complication rate was 28.3% which included major adverse cardiac events (MACE) of myocardial infarction (elevated troponins with EKG and clinical scenario), arrhythmia requiring treatment, hypotension requiring pressors, heart failure or cardiac arrest, ventilator support for respiratory failure or a documented bleeding or clotting disorder. Overall mortality for our cohort was 17.1% (92/538) but for those patients over the age of 80 the mortality was higher at 30.8% (48/156).
Table 3 summarizes the univariate analysis of factors associated with the death of COVID-19 admitted patients. They were more likely to be Caucasian (odds ratio OR: 2.52; 95% confidence interval CI: 1.55 - 4.09, p = 0.0002), above the age of 80 (OR: 3.41; 95% CI: 2.15 - 5.42, p < 0.0001), living prior to admission in a long-term care facility (OR: 4.18; 95% CI: 2.62 – 6.67,p < 0.0001), presenting with altered mental status (OR: 2.36; 95% CI: 1.23 - 4.54, p = 0.01), have a history of prior arrhythmia (OR: 2.27; 95% CI: 1.32 - 3.89, p = 0.0029), peripheral vascular disease (OR: 3.17; 95% CI: 1.28 - 7.89, p = 0.013, hypertension (OR: 2.03; 95% CI: 1.24 - 3.31, p = 0.0048), hyperlipidemia (OR: 2.04, 95% CI: 1.29 - 3.2, p = 0.001), current or prior smoker (OR: 3.18; 95% CI:1.95 – 5.17, p < 0.0001), CVA or dementia (OR: 2.24; 95% CI: 1.39 - 3.61, p < 0.0001), or pretreatment prior to hospitalization with antivirals (OR: 4.21; 95% CI: 1.26 - 14.12, p = 0.0197). Death was more likely if the EKG (OR: 2.03; 95% CI :1.23 - 3.37, p = 0.006), NT-Pro BNP (OR:3.04; 95% CI: 1.90 - 4.88, p < 0.0001), or troponin I(OR: 4.87; 95% CI: 2.93 - 8.1, p < 0.0001) were abnormal or if there was MACE: MI (OR: 6.71; 95% CI: 1.48 - 30.52, p = 0.00137), arrhythmia (OR: 3.5; 95% CI: 1.52 – 8.07, p = 0.0032), or hypotension requiring pressors (OR: 13.46; 95% CI: 7.05 - 25.71, p < 0.0001). Overall, there was no difference in mortality with the use of statin or ACE/ARB prior to admission, in-hospital treatment with azithromycin, hydroxychloroquine, convalescent plasma, remdesivir or tocilizumab. Mortality was associated with the use of antibiotics (OR: 1.91; 95% CI: 1.2 – 3.05 p = 0.0067) or steroids (OR: 2.03; 95% CI: 1.08 – 3.79, p = 0.0271) while hospitalized, but in the multivariate analysis only remdesivir was significantly associated with mortality as seen in Table 4.
Table 3: Univariate analysis of mortality risk factors with COVID-19 admitted patients. View Table 3
Table 4: Multivariate logistic regression analysis of mortality risk factors in COVID-19 patients. View Table 4
To further identify predictors of mortality, we performed a multivariate analysis of our COVID-19 admitted patients. We used all the variables after removing those with a high correlation to other variables (multicollinearity identified statistically with variable inflation factors). With the new set of variables, we fitted a multivariate logistic regression model, which selected variables predictive of mortality (Table 4). Factors associated with mortality included age, long term care, abnormal glomerular filtration rate (GFR), abnormal LDH, respiratory distress requiring a ventilator, clotting disorder, history of hyperlipidemia, or COVID-19 treatment with Remdesivir (noted as positive coefficients). Negatively associated with mortality (i.e. associated with survival) are shown with negative coefficients and included; living at home prior to admission, prehospital antiviral treatment, or treatment with tocilzumab or no COVID treatment at all during hospitalization. The predictive accuracy of this model is 91.6%.
Early in the pandemic, multiple treatment strategies were developed based on theoretical considerations [10,11]. Worldwide, clinicians were attempting to assess the possible benefits, and in critically ill patients, the public was clamoring for a "try anything" approach [12] and subsequently, medical publications were expedited to try to meet this need. Our data show that similar to others, treatment patterns evolved over time [Table 5].
Table 5: In-hospital treatment by case (may have received > 1). View Table 5
Emerging data suggested that anticoagulation was associated with lower mortality among hospitalized COVID-19 patients [13]. This prompted an increased use of therapeutic enoxaparin in our healthcare system, with 59.1% of patients presenting with an abnormal d-dimer. Subsequently, clinical trials and meta-analyses were published evaluating the various regimens shedding light on best practices [14] with extensive discussion about the prothrombotic effects of COVID-19 infection [15].
Published reports have suggested that older patients with co-morbidities are at higher risk of succumbing to COVID-19 infection. The co-morbidities that present the highest risk to the patient with COVID-19 include cancer (fatality 5.6%), hypertension (6%), COPD (6.3%), diabetes (7.3%) and cardiovascular disease (10.5%) [5]. Since then, Adult Respiratory Distress Syndrome (ARDS) complications with rapid inflammation and CT scan evidence of infection described as a ground-glass appearance have been reported [16]. Similar to the MERS-Co-V (Middle East Respiratory Syndrome related coronavirus) that caused acute myocarditis and heart failure [17] in the 2016 outbreak, cases of cardiac damage with COVID-19 have been reported. In 5 of the first 41 patients diagnosed with COVID-19 in Wuhan, there was an increase in hs-troponin I levels, and 4 of the 5 required ICU hospitalization. The higher the level of biomarker, the more severe were the symptoms. These patients appeared to have initially sought medical attention with cardiac symptoms of arrhythmia and chest pain rather than respiratory concerns suggesting cardiac injury before their death [18]. An additional report from China found that in a series of 187 patients with COVID-19, 52 (27.8%) had elevated troponins on admission with a mortality rate of almost 60%. Patients with underlying cardiac disease and elevated troponins fared worse than those with known cardiac disease and normal troponin levels [19]. A report from Germany showed an astounding 78% of COVID-19 patients evaluated with cardiac MRI revealed cardiac involvement in 78 patients (78%) and ongoing myocardial inflammation in 60 patients (60%), independent of preexisting conditions, severity and overall course of the acute illness, and time from the original diagnosis [20].
One proposed mechanism for cardiac involvement may involve ACE-2 signaling pathways that damage myocardial cells, and a massive cytokine release syndrome that can result in cardiovascular collapse [21]. The myocarditis seen with COVID-19 bears a striking similarity to the fulminant myocarditis seen with immune check point inhibitors used in the treatment of oncologic diseases. This amplification of the T-cell mediated immune response can cause a cytokine storm with high mortality [22]. Other etiologies of myocardial damage could likely include demand ischemia related to elevated heart rates, the effects of sepsis, and possibly stress induced plaque rupture [23]. The documented pro-thrombotic effects of COVID-19 are also implicated and can play a significant role [24].
Early on in the pandemic it became clear that older patients fared worse than younger patients. Based on current epidemiological data, COVID-19 infected patients aged ≥ 80 shows a greater risk of death in comparison with younger patients [25] and that advanced age is the most important predictor for mortality [26].
While our data agrees with other reports, our mortality rate appeared much higher than reported previously; 3.5% for the younger cohort (< 60) and 24.7% for those over 60, but 30.7% over the age of 80. A 40% mortality rate has been reported from Mt. Sinai in New York in COVID-19 patients with a history of heart failure reinforcing that those with pre-existing heart disease were at higher risk, not just age alone [27]. Part of the increased mortality is presumably related to co-morbidities in the elderly, and a higher incidence of pre-existing cardiac disease. The MACE rate was highly associated with poor outcomes in this study.
Review of the elderly patients that succumbed during hospitalization reveals that most had come from other than a private home setting, had more co-morbidities, and despite supportive care, had multisystem organ failure. The majority of those who died were made do not resuscitate (DNR) status and palliative care was consulted late in the hospitalization for comfort care only. The local policy of most long-term care facilities mandating patients could not be discharged to those facilities until they had 2 negative COVID tests would imply the elderly had longer LOS, but there was no difference in LOS among the groups that survived and those that did not, regardless of age.
There was no statistical difference in pre-hospital medication use with respect to ACE-1, ARB or statins on outcomes, although others have reported that patients who were on statins for 30 days prior to infection had better outcomes, less severe disease, and shorter recovery times [28]. Other analyses of patients from China reported no adverse events in those on statin or ARB with COVID-19 infection [29-31]. A difference was found in our study in those treated with antivirals prior to hospitalization, but the numbers were very small, with only 11 patients pre-treated before admission, and 5 out of 11 died while hospitalized.
Remdesivir is an inhibitor of the viral RNA-dependent, RNA polymerase with in vitro inhibitory activity against SARS-CoV-1. It had been shown to shorten the time to recovery in hospitalized patients with Covid-19 [32] but a subsequent large-scale review of over 11,000 patients showed no decrease in mortality and treatment did not shorten the course of the disease [33]. This same study showed no benefit from the antiviral drug lopinavir or interferon regimens in hospitalized COVID-19 patients. This is an ongoing controversy as the drug is the only FDA approved treatment as of this writing [34] although there have been several drugs released under an emergency use authorization. Our data showed treatment with Remdesivir was a predictor of mortality in multivariate analysis, which may have been reserved for the most seriously affected patients.
Chloroquine, and its analogue hydroxychloroquine are widely used as antimalarials, but also used to treat lupus, certain cancers, hepatic amoebiasis and rheumatoid arthritis. It has shown promise in bacterial, fungal, protozoal, amoebic, parasitic and viral infections [35] which led to a great deal of enthusiasm as a possible treatment for COVID-19 infections. This was subsequently shown in the same large trial of 11,000 patients to have no mortality benefit [36].
Tocilizumab is a recombinant humanized monoclonal antibody against the interleukin-6 receptor and has been studied in Europe and the United States with variable responses in patients requiring ventilator support [37]. Our study found a negative correlation with its use and mortality, that it was of benefit and correlated with better outcomes. Studies of steroid use suggest benefit in hospitalized patients in both increasing the number of days alive and free of mechanical ventilation over the 28-day study period along with decreased mortality [38,39]. Steroid use in our study did not correlate with mortality in multivariate analysis but did in univariate assessment and may have been affected by patient selection and timing of treatment.
Plasma from donors who have recovered from COVID-19 contains antibodies to the virus that may help suppress viral replication and modify the inflammatory response [40]. In India, the results of a trial with 464 adults showed that convalescent plasma was not associated with a reduction in progression to severe COVID-19 or all-cause mortality [41]. In the United States, results of the Mayo Clinic data suggest that convalescent plasma with high antibody titers may be more beneficial in non-intubated patients when administered within 72 hours of COVID-19 diagnosis [42].
There was a theoretical concern that the ACE-2 receptor on the X- chromosome would suggest that males of any age may be more at risk with infection, however, for our cohort, it did not appear that gender was a risk factor for mortality in the univariate analysis [43]. A significant finding in our study is that those who succumbed to the COVID-19 infection often presented with atypical symptoms. They were more likely to have had prior CVA, or dementia and presented with alterations in mental status, which was seen more frequently in the very elderly, those over age 80. This is important to note, as many elderly brought to the ER during the height of the pandemic were without advocates to assist with history and specific complaints, making triage challenging.
Our data showed that while most of the patients had elevated CRP and d-dimer, neither was associated with excess mortality in multivariate analysis. Mortality was predicted by univariate analysis in those with abnormal cardiac biomarkers including NT-pro BNP (OR 3.04) and troponin I (OR 4.87) but did not predict mortality when entered into multivariate regression analysis. Abnormal LDH and GFR were however, significant predictors in multivariate analysis.
Other studies have shown laboratory biomarkers have been used to prognosticate COVID-19. The virus binds to ACE-2 receptors in bronchial airways resulting in a significant inflammatory reaction, which can be measured via pro-inflammatory markers such as Interleukin-6, and compensatory anti-inflammatory cytokines such as Interleukin-10 along with C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), glucose, lactate dehydrogenase (LDH) and ferritin [44]. Depending on the organ system involved troponin I, NT-pro BNP, d-dimer, PT/PTT, and liver function studies can all be abnormal [45], and limited studies suggest these can be used to prognosticate disease severity [46-49].
The elderly in our cohort had a much higher death rate but most importantly, if the patient came from a long-term facility rather than a private home, they had an even higher mortality (35.1%). Considering that 73% of patients greater than aged 80 were admitted from a long-term care facility, this created a significant need to address early in the hospitalization. The International Association for Hospice and Palliative Care has called for a number of initiatives derived from the pandemic response thus far [50,51]. They advocate for:
a) Optimizing cooperation and coordination to preserve continuity of care
b) Enhanced social support for patients and caregivers by leveraging smart phone technology and telehealth platforms to maintain social connections
c) Assess emerging needs and shifting treatment strategies as needed to deliver care
d) Embed palliative care principles in the core service lines to treat patients with compassion and dignity
This data suggests there needs to be a framework for allocating resources to those with the best possible outcomes, evaluating the needs and stressors of hospital workers and evaluating and incorporating scientific evidence into institutional guidelines [48-50]. Lee Health system has successfully been utilizing Palliative care best practices and embedding certain guidelines into EPIC to facilitate consultation and care of these vulnerable patients, but this remains an ongoing initiative.
The COVID-19 pandemic presented significant challenges for residency programs [51-55] and ours was no different. Due to county-wide shutdowns and clinics without telemedicine early on, many residents were displaced to minimize patient interaction and spread of disease. This resulted in reduced work hours, with at-home "reading" rotations and more inpatient shifts to cover for quarantined colleagues. A Pandemic Response Rotation was developed to work at the COVID-19 Command Center specifically to expose residents to public health responsibilities. For some residents, the pandemic meant the inability to take timely board exams, resulting in delays for licensing and board certification.
Available personal-protective equipment (PPE) was of concern, and some attendings chose not to involve residents in patient management to minimize PPE use and interaction with COVID-19 patients. With reduced hours, PGY-3 residents struggled to meet patient encounter requirements for graduation as telemedicine encounters were initially not counted towards requirements. As the pandemic progressed, the residency program faculty and healthcare system administrators worked to ensure residents were able to utilize telemedicine and provide patient care, and subsequently virtual encounters were included for residency numbers. Due to the added stress on patients' lives, residents were vigilant of their patients' emotional health, and sought referrals to social services or psychiatric services as needed.
1. In the population of Southwest Florida, patients hospitalized for COVID-19 had an overall mortality of 17%. If patients were stratified by age, those < 60 had a mortality of 3.5% while those over aged 60 had a mortality of 24.7%. Elderly patients admitted from a long-term facility and over the age of 80 had the highest mortality of 35.1% with no gender difference noted.
2. Palliative care and Q-life services are necessary early in the hospitalization of elderly patients to assess the appropriate treatment response and avoid futile, prolonged hospitalization when comfort and compassionate care is preferred. Our palliative care service is currently in the process of embedding a tool in our electronic medical record to risk stratify patients on admission and start to engage in appropriate dialogue with respect to patients' wishes as these are very difficult conversations to have in the midst of a pandemic.
3. It is possible to risk stratify disease severity in COVID-19 patients upon arrival to the Emergency Department by assessing living arrangements, co-morbidities, clinical status, and cardiac and other biomarkers. Risk factors associated with increased mortality included age, long term care, abnormal glomerular filtration rate, respiratory distress requiring a ventilator, clotting disorder, history of hyperlipidemia, and can be used to help triage patients for optimal care.
4. Because of the local policy of long-term care facilities to keep patients hospitalized until they had two negative COVID tests, some hospitalizations were unavoidably prolonged. The system should consider convalescent strategies to avoid returning patients to a population of at-risk residents and avoid prolonged hospitalizations.
5. This data should be used to support comprehensive pandemic planning for southwest Florida taking into consideration the large numbers of vulnerable patients at the highest risk for complications and death. Comprehensive assessment with predictive labs may help triage these patients for appropriate use of limited resources, earlier use of palliative care, or special units to quarantine from other vulnerable populations.
The retrospective nature of this study is a significant limitation with inability to collect appropriate data on all patients for extensive analysis. Normal or abnormal labs were treated as discrete variables and were not further analyzed to assess the absolute value of lab values on outcomes. There was limited laboratory evaluation with incomplete cardiac biomarkers and imaging studies, that may have added considerably to the data. As with all retrospective studies, the data collected at the time is subject to availability without verification, and if not documented, could not be captured. Despite that, in a large community setting, the most vulnerable were identified and recommendations have been made to help address that segment of the population with a very high mortality rate. This pandemic and any future surge will have an effect on physicians in training as well as service lines that care for the elderly population in our community.
The authors would like to acknowledge the data collection and editorial assistance of our participating investigators: Mikhailia M Lake MD, William B Cutting, MD, Renee Wong MD, Moises Perez DO, Richard Chazal MD FACC FAHA, Director of the Heart and Vascular Institute for Lee Health, Jeff Lassell data analyst for the Heart and Vascular Institute, as well as the assistance of Alex Daneshmand, DO, Ph.D Chief Safety Officer Lee Health, and Jonathan Von Koenig, DO who reviewed and contributed to the palliative care discussion.
AMA conceived of the study, received IRB approval for the project, obtained, analyzed and interpreted the data and made substantial contribution to the writing of the manuscript.
SC: Obtained, analyzed and interpreted the data and made substantial contribution to the writing of the manuscript.
KQ: Obtained, analyzed and interpreted the data and contributed to the writing of the manuscript.
CO: Substantially contributed to the analysis of the data and contributed to the writing of the manuscript in a significant fashion.
MM: Analyzed the data, contributed to the writing and editing of the manuscript and contributed to design of Figures and Tables.
This study was approved by the Lee Health IRB, HIPAA informed consent was waived for this minimal risk study.
The datasets analyzed are available upon reasonable request.
Authors declare they have no competing interests.
No funding was associated with this work except for contributing statistical analysis provided by Lee Health.
Statistics provided by Lee Health.