Background: The global impact of COVID-19 continues to affect all sectors, especially the healthcare sector.
Settings: This retrospective study was conducted using data generated from routine program implementation in low and middle income setting across 2 north eastern states of Nigeria in sub- Saharan Africa.
Methods: A retrospective analysis was conducted to assess the impact of COVID-19 on access to HIV services in Northeast Nigeria. We assessed data from four periods: pre-COVID (November 2019-March 2020), COVID lockdown (April-May 2020), COVID restrictions (June-July 2020), and COVID relaxed restrictions (August -September 2020).
Results: Analysis revealed a reduction in HIV service outcome during the COVID lockdown. Of the 602 new HIV cases identified in that period, only 413 were linked to care, signifying a 68.8% ART uptake rate compared to 93% in the pre-COVID period.
Conclusions: Strategic measures are needed to ensure continued HIV service delivery care for key populations to counter subsequent effects of the pandemic.
HIV, COVID-19, Antiretroviral therapy, Continuum, Pandemic, Key populations
The first case of the Corona virus infection (COVID-19) was reported in December 2019 in Wuhan, China [1]. The causative agent, the SARS-COV-2 virus [2], rapidly spread across the world, leading to the World Health Organization (WHO) declaring it a pandemic in March 2020 [1]. The global impact of the pandemic resulted in disrupted healthcare and socioeconomic systems and its rapid spread necessitated the introduction of non-pharmaceutical interventions (NPI) such as restricted gatherings, public spaces closure, and country lockdowns [3]. Nigeria recorded her first COVID-19 case in March 2020 [4] and instituted mitigation strategies including a lockdown which went into effect between April and July 2020, strict restriction on movements and travels, and establishment of COVID-19 isolation centers to contain the spread of the virus [5]. Likewise, significant focus, efforts and human resources were being deployed to respond to the COVID-19 pandemic [6]. These strategies, although crucial for COVID-19 containment, had several implications for healthcare delivery systems including HIV treatment services. Given that the healthcare sector in Nigeria is already contending with a stretched workforce, the deployment of human resources from HIV services to the COVID-19 response meant disruptions to HIV services with expected increases in new infections, fewer tests, and lesser access to care and treatment [7]. The pandemic created challenges for the already fragile health system and threatened a reversal in the gains being achieved in the control of HIV/AIDS in the country [8].
Nigeria has the third highest HIV burden worldwide [9]. In 2020, the national prevalence was 1.4% of its adult population aged 15-49 years with an estimated 1.9 million people living with HIV (PLHIV) [10]. The HIV epidemic in the country is not evenly distributed with certain regions and groups such as key populations bearing the brunt. Key populations (KP) groups including female sex workers (FSW), men who have sex with men (MSM), people who inject drugs (PWID), and transgender persons (TG) consist of about 3.4% of the population, yet account for almost 32% of new HIV infections [11]. Socio-cultural barriers, stigma and Nigeria's unfavorable political and legislative environment exacerbate KP groups' vulnerability to infection and access to care. To overcome these challenges, HIV programmes in Nigeria with support from the United States President's Emergency Plan for AIDS Relief (PEPFAR) have long developed and implemented One Stop Shops (OSS) for KPs. These OSS are KP friendly health facilities where healthcare providers are trained to understand the peculiar needs of KP groups and effectively provide HIV treatment and care options in conducive settings that protect their privacy [12]. The COVID-19 pandemic posed a threat to these services due to the implementation of lockdowns and restricted movement. In response to that, a PEPFAR KP program developed and implemented a mitigation strategy to reduce the impact of the COVID-19 pandemic lockdown on HIV/AIDS program services, including testing, treatment, and viral load. The program consisted of the implementation of a differentiated service delivery (DSD) model such as the establishment of community clinical service assistant points (CSSAP) for decentralized drug refill services at the community and the scale up of mobile testing, treatment, and viral load services. The DSD model is a client-centered approach that simplifies and adapts HIV services to reflect the preferences of various groups of PLHIV while reducing burden on the healthcare systems [13]. Through the DSD model, KPs living with HIV (KPLHIV) were able to access antiretroviral therapy (ART) in the community based on their own preferred arrangements.
The magnitude to which COVID-19 restrictions and measures have affected global HIV programmes is still unclear. A recent modeling study by Jewell B, et al., predicted that disruptions to HIV services for PLHIV and high risk individuals caused by the COVID-19 pandemic in sub-Saharan Africa would have severe consequences on the HIV/AIDS epidemic control gains in the region. The authors estimate that a 6-month disruption of ART across 50% of PLHIV on treatment would be expected to cause an increase in HIV-related mortality with over 500,000 extra deaths from AIDS-related illnesses over a 1-year period compared to a period with no disruption [14]. Another study observed a 59% decrease in the number of men who have sex with men undergoing facility-based HIV testing and a 34% reduction in ART uptake rates during the implementation of COVID-19 measures in Jiangsu, China [15]. Similarly, a South African article reported survey results by the healthcare organization Right to Care and the Africa Health Research Institute (AHRI), which showed declines of about 50% in HIV and TB medication collection during lockdown [16]. This study analysis explores the impact of COVID-19 lockdown and restrictions on HIV services outcome i.e., testing, new diagnosis, linkage to care and total treatment figures among key populations in two Northeastern states of Adamawa and Bauchi in Nigeria. The study hypothesizes that COVID 19 measures may negatively impact HIV services and compares actual HIV data to expected numbers captured during the analysis period.
A multicenter retrospective study was conducted between November 2019 to September 2020 among KP groups receiving HIV care and services in two Northeastern states in Nigeria.
Inclusion criteria include all KPs tested, identified KP-PLHIV, and KPS linked to treatment during the pre-COVID, COVID and immediate post COVID period. Exclusion criteria are KPs tested outside the study period as well as non KPs.
We reviewed HIV data collected over 10 months from validated source documents. We classified this data into four periods: Pre-COVID (September 2019 March 2020), COVID lockdown (April-May 2020), COVID restrictions (June-July 2020), and COVID relaxed restrictions (August-September 2020). A trend analysis covering the four periods was conducted using a simple combo chart indicating the relationship between the various periods and HIV services outcome (testing, positives, linkage and new on treatment). Exponential smoothing was used in forecasting the figures and subgroup differences were assessed using linear regressions. The independent variable was periods in months and the dependent variable was HIV services outcome. Model for linear regression curve compares observed values with predicted (linear). All curves were forecasted using SPSS Statistics (version 28.0.1) in a time series model for November 2019 to September 2020. Comparative analysis was based on the monthly number of reported data vs. expected numbers. P-value of a = 0.05 was deemed statistically significant.
Data for analysis was stored in an encrypted drive to ensure confidentiality and secure access only to authors. Clients were given unique codes that identified them while ensuring confidentiality of data. The PEPFAR DATIM platform was the primary data storage tool for this study.
While service was provided, informed consent, confidentiality of data and results, communication on progress of care was strictly adhered to. All other ethical standards for data protection. Clients were properly counseled to make informed decisions about testing and commencement of treatment.
We present our findings following the HIV care continuum cascade from testing to ART initiation.
Participants include MSM, FSW, PWIDS, and Transgender persons in the Northeastern states of Adamawa and Bauchi in Nigeria. These groups are highly mobile and are often discriminated against, as such services are often provided to them in a safe space called the OSS.
A total number of 29,635 HIV tests was conducted over the 11 months period with 3460 positive patients identified (Figure 1).
 Figure 1: Trend of HIV services from November 2019 to September 2020.
View Figure 1
Figure 1: Trend of HIV services from November 2019 to September 2020.
View Figure 1
The number of KPLHIV linked to ART care was 3357 (97%) over the 11 months period. The lowest linkage to care rates was recorded during the COVID-19 lockdown. Only 68% of PLHIV were linked to care. About 32% of all newly diagnosed KPLHIV during the lockdown period were considered to experience interruption in treatment (IIT). Subsequent tracing strategies were employed to return the majority of those KPLHIV back to care. This is evidenced in the data from June to July 2020, where a 120% ART uptake rate is recorded (Figure 1).
The plots in Figure 2 shows a clear dip in HIV service outcome for testing (HTS_TST), positive (HTS_POS), and new on treatment (TX_NEW) with a linear relationship seen between the independent and dependent variables. This dip commenced from March and gradually worsened with the biggest drop in service outcome noticed in May, which corresponds to the national COVID-lockdown period. Service outcomes gradually began to improve towards the end of May despite the lockdown and subsequent restriction. This improvement was steady with services returning to pre-COVID figures in September when COVID restrictions were relaxed by the government. The gradual improvement in service outcome was due to the development and implementation of a COVID-19 mitigation strategy to improve HIV testing linkage, and treatment services.
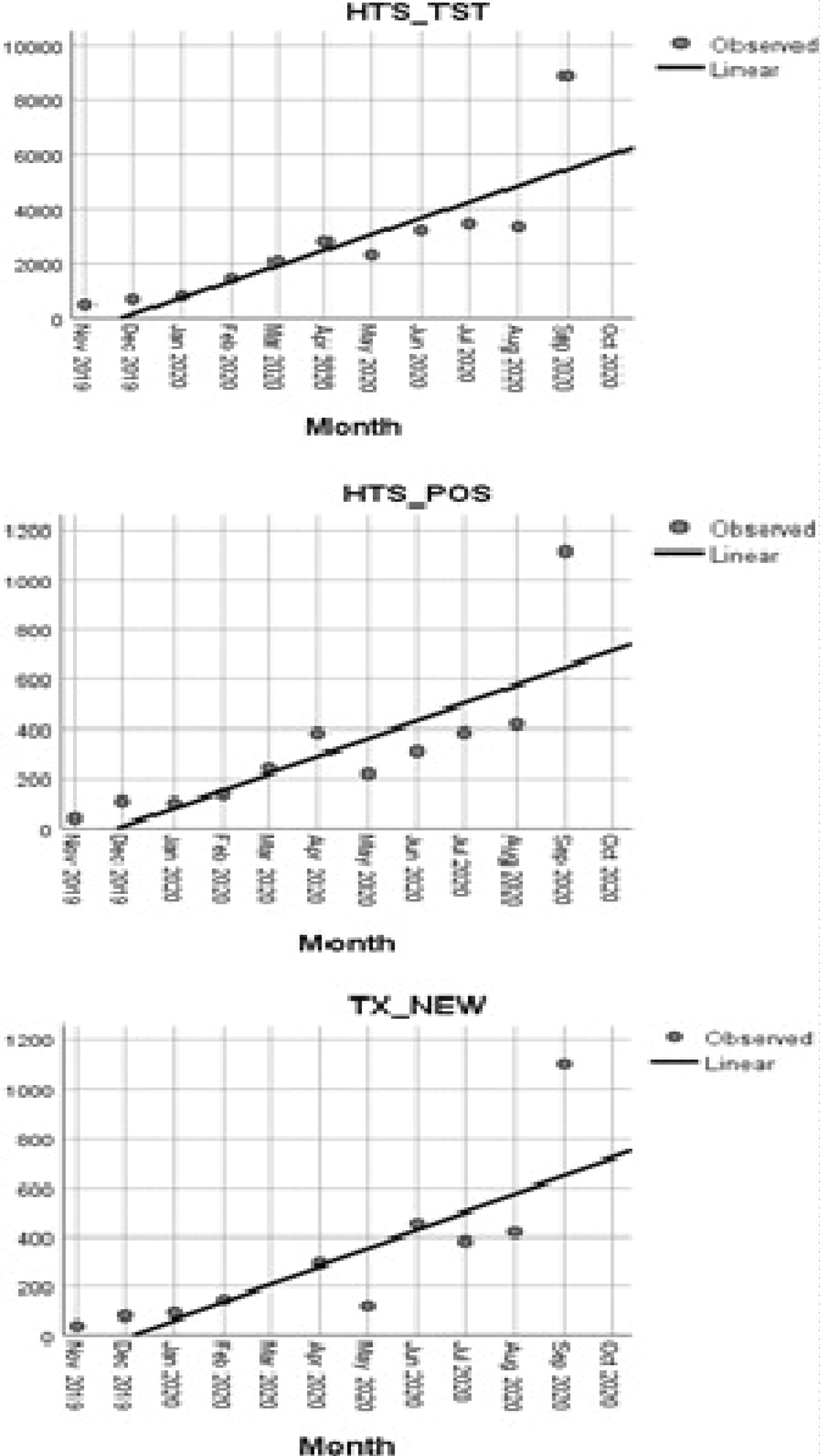 Figure 2: Trends in expected vs. real number of HIV services from Nov 2019 to Sep 2020.
View Figure 2
Figure 2: Trends in expected vs. real number of HIV services from Nov 2019 to Sep 2020.
View Figure 2
The COVID-19 pandemic has had wide-ranging impacts on HIV epidemic control efforts and delivery systems worldwide, including Nigeria. Globally, the number of reported HIV services in the continuum of care decreased [17,18]. According to a WHO report, over 70 countries were confronted with the risk of ART interruption impacting 17.7 million PLHIV receiving treatment between April and June 2020 due to limited or diverted HIV services [19]. In Northeast Nigeria, the number of reported KPLHIV linked to ART and initiated on treatment in our study context decreased during the COVID-19 lockdown period compared to the expected estimated data. While the figures for HIV testing were lower than expected during the lockdown period, perhaps the most significant outcome was that among KPs who tested positive during HIV screening tests within that period, only about two-thirds received timely health care services. Of the 602 new HIV cases identified during the lockdown period, only 413 were linked to care signifying a 68.8% ART uptake rate compared to 93% in the pre-COVID period. These results demonstrate how unexpected disruptions such as the COVID-19 pandemic can affect all parts of the HIV delivery system especially given the rapidness and swiftness within which the virus spread, thus putting several healthcare systems in Nigeria in jeopardy because they were not equipped to deal with the situation. Interruptions in treatment will reverse the gains from several years of treatment program [7].
In the era of test and treat where HIV treatment is being optimized for all identified positive patients [20], disruptions to ART services and delayed initiation in care can be crucial because this not only leads to poor treatment outcome among PLHIV but also increased transmission in the population and the risk of developing PLHIV drug resistance to certain HIV regimens [21]. Access to HIV services including testing and linkage to ART has several implications for the UNAIDS 95-95-95 target of 95% of PLHIV knowing their status, 95% of those who know their status being on ART and 95% of those on ART being virally suppressed by 2025 [22]. Currently, two of the past HIV targets set for epidemic control; (i) The goal of fewer than 500,000 annual new infections and 500,000 AIDS-related deaths in 2019 [23] and (ii) The 90-90-90 targets for 2020 were not achieved by several countries [24]. Therefore, temporary disruptions to global HIV programmes need to be avoided at all costs because those gaps can be additive in increasing onward transmission, AIDS-related deaths, and unsuccessful treatment outcomes, especially if the UNAIDS 95-95-95 target is to be achieved.
Nevertheless, once the realization that the COVID-19 pandemic was going nowhere and that this would be one of the added challenges that the HIV epidemic would face, it dawned on HIV programmes to initiate strategies that would protect the gains of epidemic control and ensure continuity of services. The PEPFAR KP program in Northeast Nigeria was one of such strategies initiated. The program developed context specific HIV program mitigation strategies some of which were novel such as the CSSAP and others [25]. The program included a differentiated DSD model in the form the CSSAP for decentralized drug refill services at the community and the scale up of mobile testing, treatment, and viral load services. The flexibility of the strategies, of which when combined not only increased access to HIV services, but also demonstrated how HIV services, including community testing, and linkage to ART, can be not only sustained but expanded during the COVID-19 pandemic. At the end of May 2020, the lockdown policy was lifted, and instead COVID-19 restrictions were put in place. The restrictions enabled more flexibility around providing HIV care and services to KPLHIVs. This approach would prove effective as evidenced by the data because HIV linkage rates within our study context start to increase after the COVID lockdown period with significant linkage to care rates (100% new HIV cases linked to ART) recorded between June to Sept 2020 as expected. The PEPFAR KP program facilitated and expanded KPLHIV centered alternatives for ART dispensation. Comparable adopted strategies within the COVID-19 pandemic context have been described in sub-Saharan African HIV programmes [26,27]. Moreover, several studies have shown that initiating and continuing ART in the community had increased rates of retention and HIV viral suppression for PLHIV when compared to facility-based care [28-30]. Similarly, within the Nigerian context, community-based ART initiation has proven to be effective with community ART initiation being associated with improved linkage and retention in care and significant viral suppression in patients, when compared with referral to facility-based for care [31].
Our analysis has a few limitations. Our study period did not explore past the HIV care continuum. The data was only collected at a single point in time, so we cannot account for changes over the course of the epidemic. Individual level consequences of the pandemic such as depression, mental health was not captured and could have affected treatment interruptions even if the patients had their drugs and thus retention of PLHIV established in care and their viral suppression during that period needs further analysis. Despite these limitations, our analysis showed that the COVID-19 pandemic and the subsequent lockdown policies and restrictions had some negative impact on the HIV delivery system.
The intersection of the COVID-19 pandemic and the HIV epidemic highlights the vulnerability and gaps in HIV services that if not mitigated, could unravel potential epidemic control gains. It also underscores the importance of pandemic readiness towards sustaining critical health services during any pandemic. HIV service adaptations and mitigation plans that ensure continuity of care for PLHIV especially during unexpected disruptions such as the COVID-19 pandemic are thus essential in global HIV health programmes to ensure positive clinical outcomes for PLHIVs.
The KP HIV program which led to these results was funded by the President's Emergency Plan for AIDS Relief (PEPFAR). However, the authors note that no funding was received to assist with the preparation of this manuscript.
This retrospective study does not involve a direct dealing with human subjects but rather a retrospective program-level data review and analysis. There was strict adherence to data confidentiality and protection.
MK designed and conceptualized the study. The analyses were performed by MK, and AA. The first draft of the manuscript was written by MK, AU, MB, OA, HS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.