The purpose of this study was to verify the risk factors present in patients on the kidney transplant waiting list that may interfere with the incidence of CV events and death during the first 12 months after transplantation.
Based on data collected prospectively during pre-transplant workup, a retrospective study was conducted including 665 patients followed up until death or completing 12 months post-transplantation. Endpoints were the composite incidence of CV events and death.
The prevalence of diabetes, LV hypertrophy and CV disease at baseline was high; 14% of patients had angina, 26% an abnormal myocardial scan, and 47% coronary artery disease (CAD). CV events occurred in 53 patients (8.4%) and in 29 (55%) caused death. The independent predictors of events were age ≥ 50 years (HR: 2.292; CI%: 1.093-4.806), angina (HR: 1.969; CI%: 1.039-3.732), and altered myocardial scan (HR: 1.905, CI% 1.059-3.428). Altered myocardial scan (HR: 2.601; CI%: 1.129-5.988) was the sole predictor of CV death.
The incidence of CV events and death were predicted by variables associated with myocardial ischemia. Patients with pre-transplantation myocardial ischemia should be considered at a higher risk of developing early CV complications and managed accordingly before, during, and after the operation.
Transplantation, Chronic kidney disease, Risk factors, Cardiovascular disease
CAD: Coronary Artery Disease; CKD: Chronic Kidney Disease; CVD: Cardiovascular disease; LV: Left ventricular; MI: Myocardial Infarction; MACE: Major Adverse Cardiovascular Event; SPECT: Single Photon Emission Computed Tomography
Cardiovascular disease (CVD), mostly caused by atherosclerosis, is a leading cause of death in patients with chronic kidney disease (CKD). Renal transplantation is related to reduced incidence of CV events and mortality, but they are still higher than that observed in the general population [1,2]. For that reason, patients who undergo renal transplantation are usually assessed for risk factors and actual CVD with the objective of reducing the incidence of CV complications during the post-transplant period. It was demonstrated that the classical risk factors for CV events are prevalent in renal transplant recipients added to others associated with allograft dysfunction or related to the use of immunosuppressive medication [3,4]. However, such studies were mostly concerned with the long-term prognosis of stable patients who had survived the early post-transplant period [3-6].
Clinicians in charge of patients on the waiting list face a different problem. They want to know the risk factors present before transplantation associated with major complications during the pre-transplant and early post-transplant period. With that objective, at our center, we perform a comprehensive clinical CV evaluation and then select patients for noninvasive and invasive coronary testing using a modification of the American Society of Transplantation index, [7] as reported [8].
In the present investigation, we aimed to verify the most significant risk factors present in patients on the waiting list that may interfere with the incidence of cardiovascular events and cardiovascular death during the first 12 months after transplantation. We did not take into consideration risk factors that could appear after transplant, like delayed graft function, post-transplant diabetes, or other transplant-related risk factors, because that information could not be available during the pre-transplant workup. We used data collected prospectively in patients belonging to the KiHeart cohort that was established at our center with the objective of creating a systematic cardiovascular evaluation to define the best approach for diagnosing and treating cardiovascular disease in renal transplant candidates [9].
This was a single-center, observational study in a population of hemodialysis patients included on the waiting list for renal transplantation studied prospectively and analyzed retrospectively. This study was approved by the institutional ethics committee and conducted according to the Declaration of Helsinki.
We used detailed information on more than 2000 renal transplant candidates sent to our service for cardiovascular screening before being formally included on the list. Baseline data were collected at cardiac evaluation using a pre-specified protocol and entered into a computerized database.
Patients were part of a cohort (The Ki-Heart cohort) designed to assess the optimal method of screening for and managing CVD and coronary artery disease (CAD) before and after kidney transplantation. We included adult (> 18 years of age) hemodialysis patients being considered for kidney transplantation. We used a protocol that is uniformly applied to all participants, as follows. We obtain from all patients a medical history based on a standard questionnaire, with special interest in CV risk factors and previous and/or current cardiovascular disease. We also perform routine laboratory tests, resting 12-lead electrocardiography and transthoracic echocardiography. Patients considered at high risk for CAD (age ≥ 50 years or with diabetes, or having angina or CVD, such as previous myocardial infarction or stroke, left ventricular systolic dysfunction, previous coronary intervention, or extracardiac atherosclerosis, or having noninvasive testing suggestive of CAD as defined by myocardial perfusion scanning after pharmacological stress with dipyridamole or adenosine) were referred for coronary angiography.
Body mass index (weight in kilograms divided by height in square meters) was calculated from data collected on a day between 2 consecutive dialysis sessions. Smokers comprised current and past tobacco users. Hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg. Dyslipidemia was defined as total cholesterol and/or triglycerides ≥ 5.16 mmol/dL and 2.28 mmol/dL, respectively. Diabetes was defined according to American Diabetes Association guidelines. CV disease was defined by at least one of the following: Heart failure, previous myocardial infarction (MI) or stroke, coronary artery disease, and arterial vascular disease. Heart failure was defined as New York Heart Association functional Class III or IV. MI was defined by characteristic electrocardiographic and enzyme alterations and stroke by clinical/radiological evidence. Left ventricular hypertrophy was defined by LV mass index > 115 g/m2 (men) and > 95 g/m2 (women). The diagnosis of arterial vascular disease was based on clinical grounds (absence of pulse in 1 or more peripheral arteries), a history of amputation or vascular intervention, or both. We used arterial angiography in those cases suspected by not confirmed by physical evaluation. Sudden death was defined as death from natural causes occurring within 1 h after initiation of symptoms with no definitive assessment of its cause. The diagnosis of acute pulmonary edema was based on acute episode of respiratory distress with typical clinical and radiological evidence of lung congestion requiring emergency intervention. Unstable angina was defined as an acute episode of myocardial ischemia without detectable myocardial necrosis. Significant CAD was arbitrarily defined as luminal stenosis ≥ 70% in 1 or more epicardial arteries or at least 50% narrowing of the main left coronary artery by visual estimation from 2 independent experts who did not participate in this study.
Patients with significant CAD were evaluated by the study team, according to the American Heart Association/American College of Cardiology criteria for coronary intervention [10] and selected either to continue on medical treatment or to undergo myocardial revascularization (surgical or percutaneous) plus medical treatment. Percutaneous intervention (bare metal stent) was preferred whenever the two invasive procedures were considered adequate by current guidelines. The study team did not participate in the selection of patients for transplantation; we only defined risk.
Patients in this study had received hemodialysis, performed in 4-hour sessions, 3 times/week. Patients were maintained on statins, aspirin, angiotensin-converting enzyme inhibitors (or angiotensin-receptor blockers), and beta-blockers, according to current guidelines for secondary prevention of CV events, independently of clinical evaluation, and were seen at least two times per year in our service when medication was checked and enforced. They had free access to medication, dialysis, and transplantation. Cardioprotective medication was reintroduced as early as possible after the operation. Routine immunosuppression consisted of prednisone, mycophenolate and tacrolimus, or cyclosporine. Censored events were verified during clinical visits, by telephone, or electronic mail. When events took place in other hospitals, we resorted to chart reviews and contact with attending physicians.
From August 1997 to February 2017, 2404 hemodialysis patients underwent cardiovascular evaluation in our service before being formally included on the transplant waiting list. Excluded from the study were 112 patients (4.7%) leaving 2292 to be included (Figure 1). During this period, 665 patients (29%) underwent transplantation and were followed up until death or 12 months after transplantation. Patients who returned to dialysis were not censored at that point. The median time on the waiting list was 23.2 months. No transplanted individual was lost to follow-up.
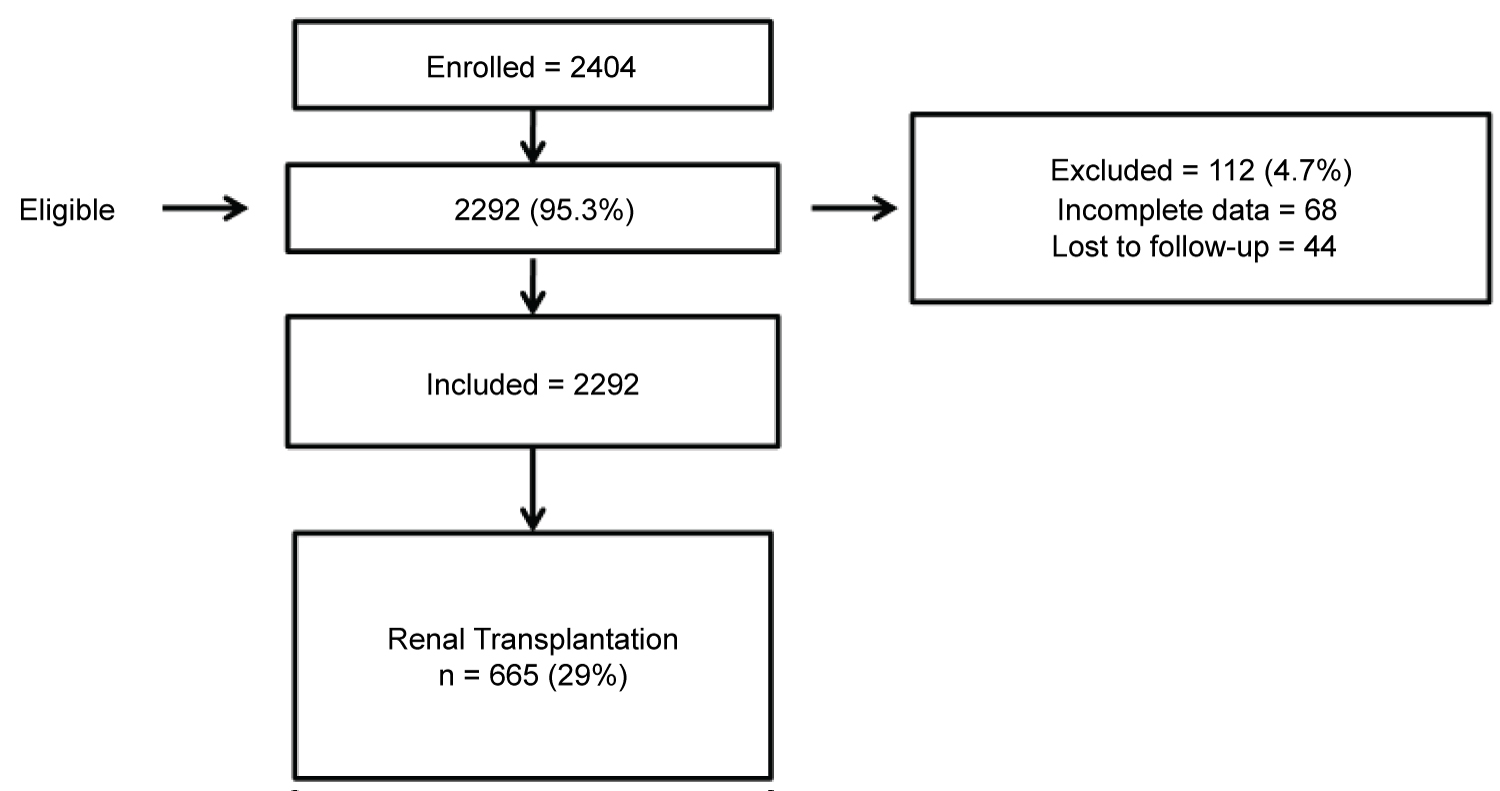 Figure 1: Flow chart showing patients included in the study.
View Figure 1
Figure 1: Flow chart showing patients included in the study.
View Figure 1
Primary endpoint was the composite incidence of CV events (myocardial infarction, unstable angina, stroke, sudden death, heart failure, acute pulmonary edema, or acute peripheral arterial syndrome). Secondary endpoint was the composite incidence of cardiovascular death. When more than 1 event occurred, only the first was considered for analysis because was a decision of the study team.
Values are expressed as means, standard deviation of the means, medians, and percentages. We used a statistical software package (SPSS Statistics, version 20.0, IBM, Armonk, NY, USA) for analysis of the data. Survival curves were constructed using the Kaplan-Meier method and compared by using the log-rank test. Cox proportional hazards model was used to verify the variables associated with outcomes. The variables selected for multivariate Cox model were those showing a significant or near-significant association with outcomes on univariate analysis. A P value of < 0.05 was considered significant.
At baseline, the majority of our patients were older than 50 years, with a predominance of males and whites. There was an increased prevalence of hypertension, diabetes, left ventricular hypertrophy, and associated cardiovascular disease (Table 1). Angina was reported by 14% of our patients, whereas 26% of those assessed by myocardial scan had either fixed or transient perfusion defects. Coronary angiograms were performed in 57%, and in 47%, significant narrowing was observed. Before undergoing renal transplantation, 34/374 patients (9.0%) underwent coronary interventions (surgical or percutaneous).
Table 1: Base-line characteristics n = 665. View Table 1
During 12 months of follow-up, 53 CV events were observed in 665 patients (8.4%), myocardial infarction (2.8%), unstable angina (1.2%), sudden death (1.5%), and stroke (1.2%) being the most frequent. The mean time of CV event occurrences was 9.3 ± 4.4 months. Univariate analysis showed that the variables significantly associated with CV events were age ≥ 50 years, diabetes, angina, previous myocardial infarction, arteriopathy and abnormal myocardial scan (Table 2). Most classical CV risk factors like dyslipidemia, hypertension, smoking, obesity, and left ventricular hypertrophy were not predictors of events. Coronary artery disease, as assessed by angiography, was not associated with adverse events.
Table 2: Pre-transplant variables and cardiovascular events during early (12 months) post-operative period in patients undergone renal transplantation n = 665, univariate analysis. View Table 2
Multivariate analysis, which included the variables associated with outcomes on the univariate analysis, showed that age ≥ 50 years (HR: 2.292; CI%: 1.093-4.806), angina (HR: 1.969; CI%: 1.039-3.732) and fixed or transient perfusion defects on myocardial scan (HR: 1.905; CI%: 1.059-3.428) were the independent predictors of early major CV events (Table 3), (Figure 2, Figure 3 and Figure 4).
Table 3: Pre-transplant variables and cardiovascular events during early (12 months) post-operative period in patients undergone renal transplantation n = 665, multivariate analysis. View Table 3
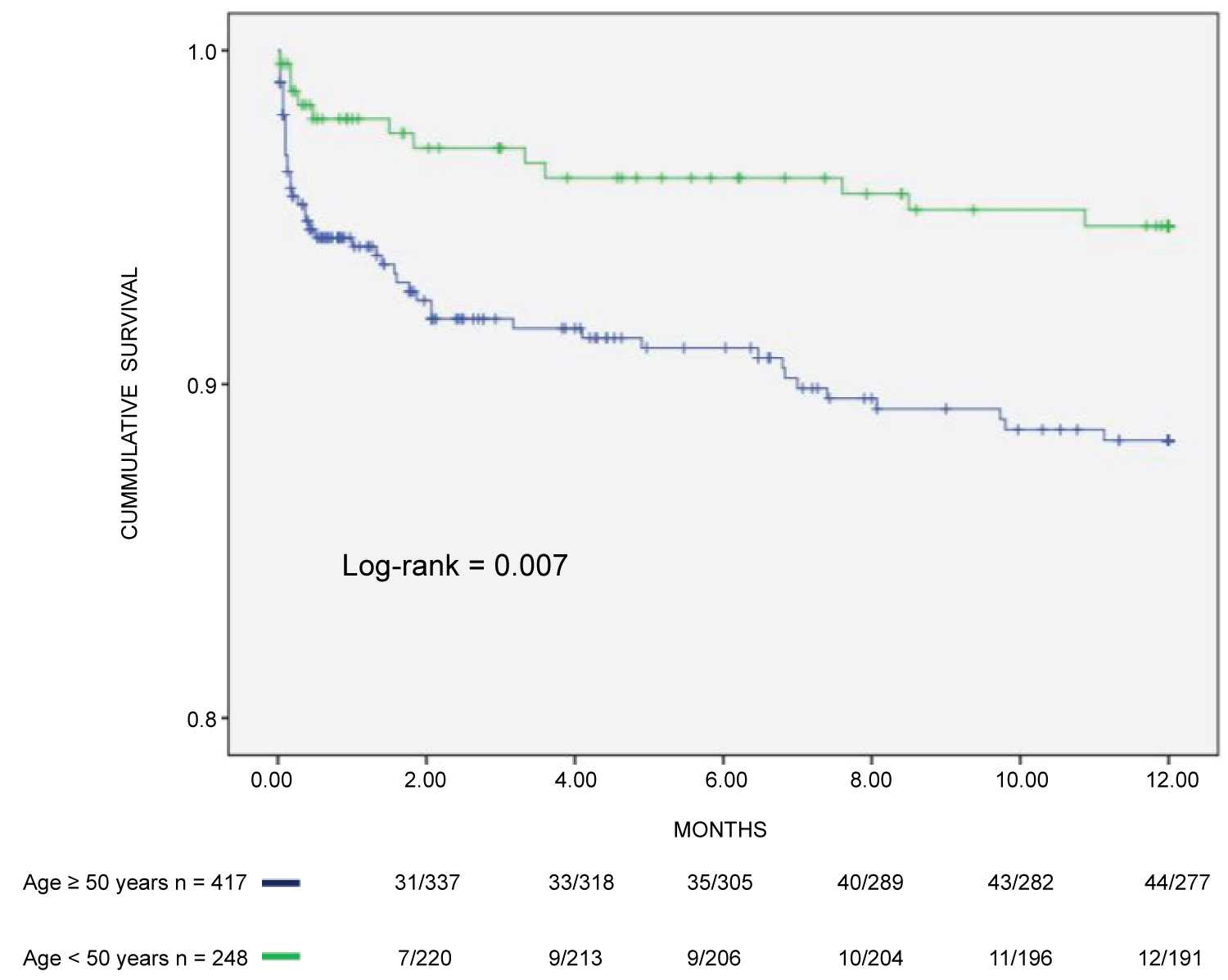 Figure 2: Composite incidence of cardiovascular events in CKD patients on hemodialysis assessed by age.
View Figure 2
Figure 2: Composite incidence of cardiovascular events in CKD patients on hemodialysis assessed by age.
View Figure 2
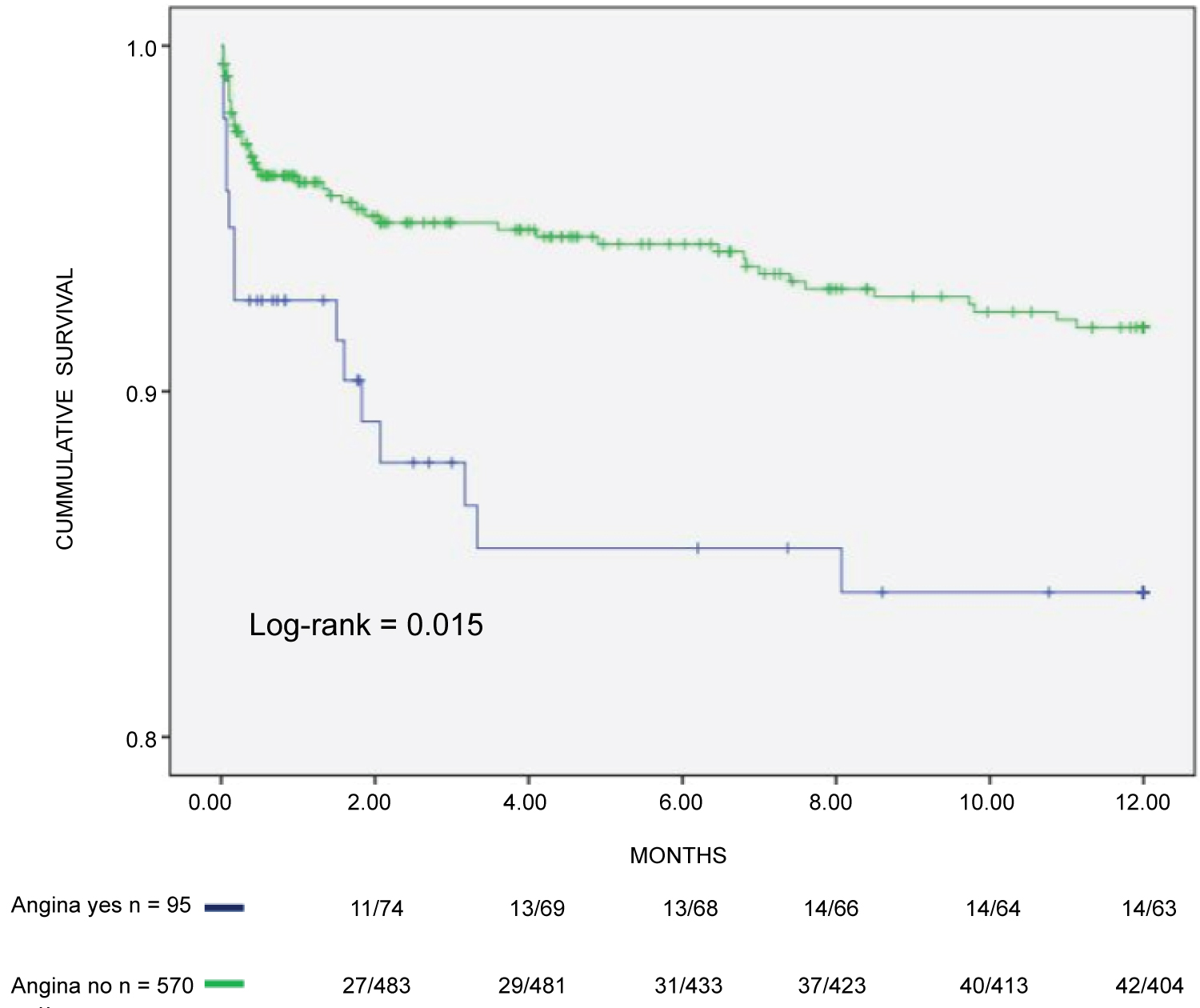 Figure 3: Composite incidence of cardiovascular events in CKD patients on hemodialysis assessed by angina.
View Figure 3
Figure 3: Composite incidence of cardiovascular events in CKD patients on hemodialysis assessed by angina.
View Figure 3
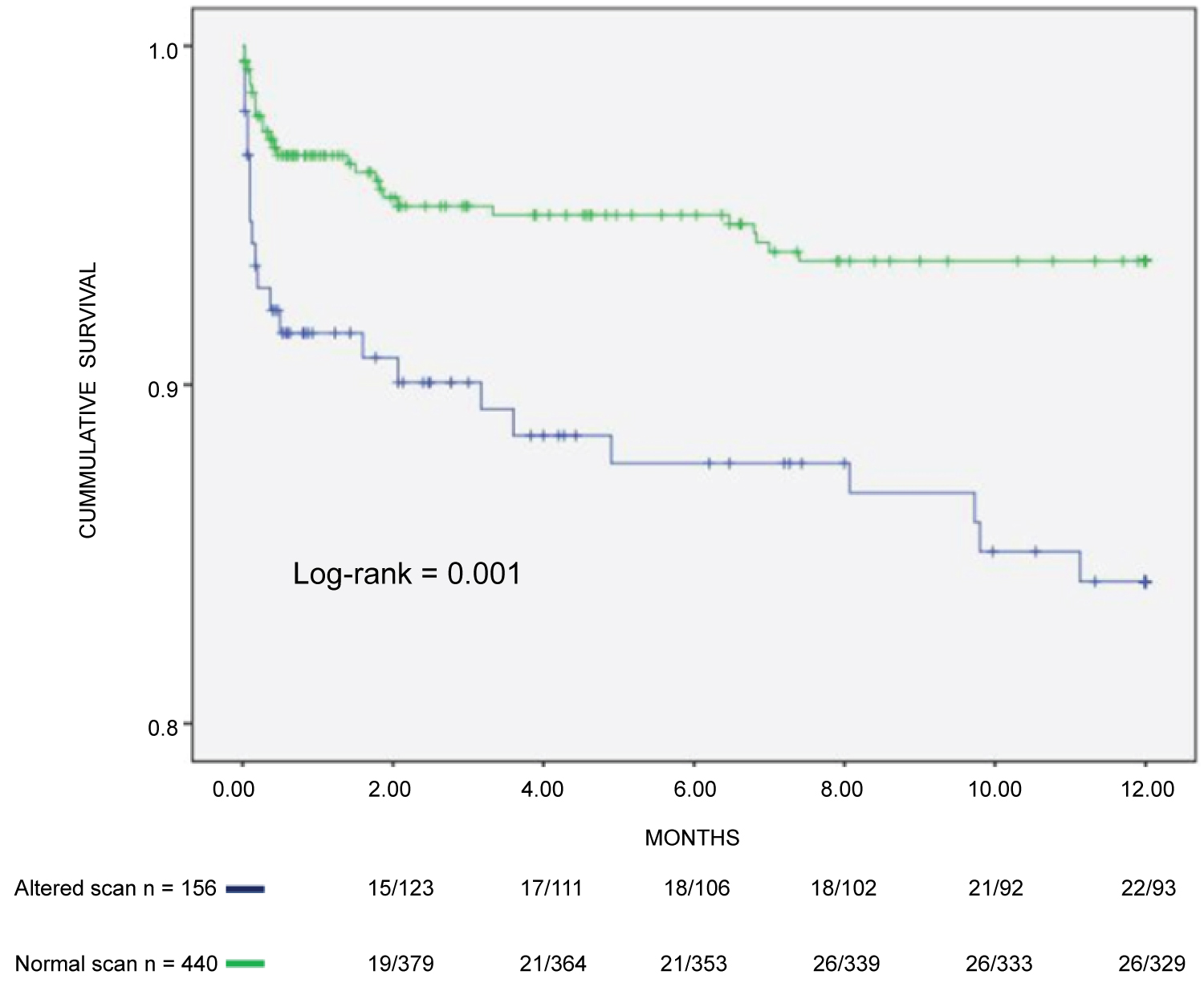 Figure 4: Composite incidence of cardiovascular events in CKD patients on hemodialysis assessed by myocardial scan.
View Figure 4
Figure 4: Composite incidence of cardiovascular events in CKD patients on hemodialysis assessed by myocardial scan.
View Figure 4
Death occurred in 110 patients. In 29 patients, the cause of death was cardiovascular (26% of all deaths). Table 4 shows the relationship between CV events and CV deaths. Fifty-five percent of CV events led to death (29/53), myocardial infarction, sudden death, and stroke being the most frequent. Of note is the very high incidence of death associated with myocardial infarction and stroke, many times higher than that observed in the general population.
Table 4: Cardiovascular events and cardiovascular deaths in renal transplant recipients during the first 12 months post-operation. View Table 4
The baseline variables significantly associated with CV death on univariate analysis were diabetes and altered myocardial scan (Table 5). Age ≥ 50 years and white race came close but did not achieve significance. Multivariate analysis that included race, age, diabetes, and abnormal scans showed that an altered myocardial scan (HR: 2.601; CI%: 1.129-5.988) was the sole predictor of CV death (Table 6 and Figure 5).
Table 5: Pre-transplant variables and cardiovascular death during early (12 months) post-operative period in patients undergone renal transplantation n = 665, univariate analysis. View Table 5
Table 6: Pre-transplant variables and cardiovascular death during early (12 months) post-operative period in patients undergone renal transplantation n = 665, multivariate analysis. View Table 6
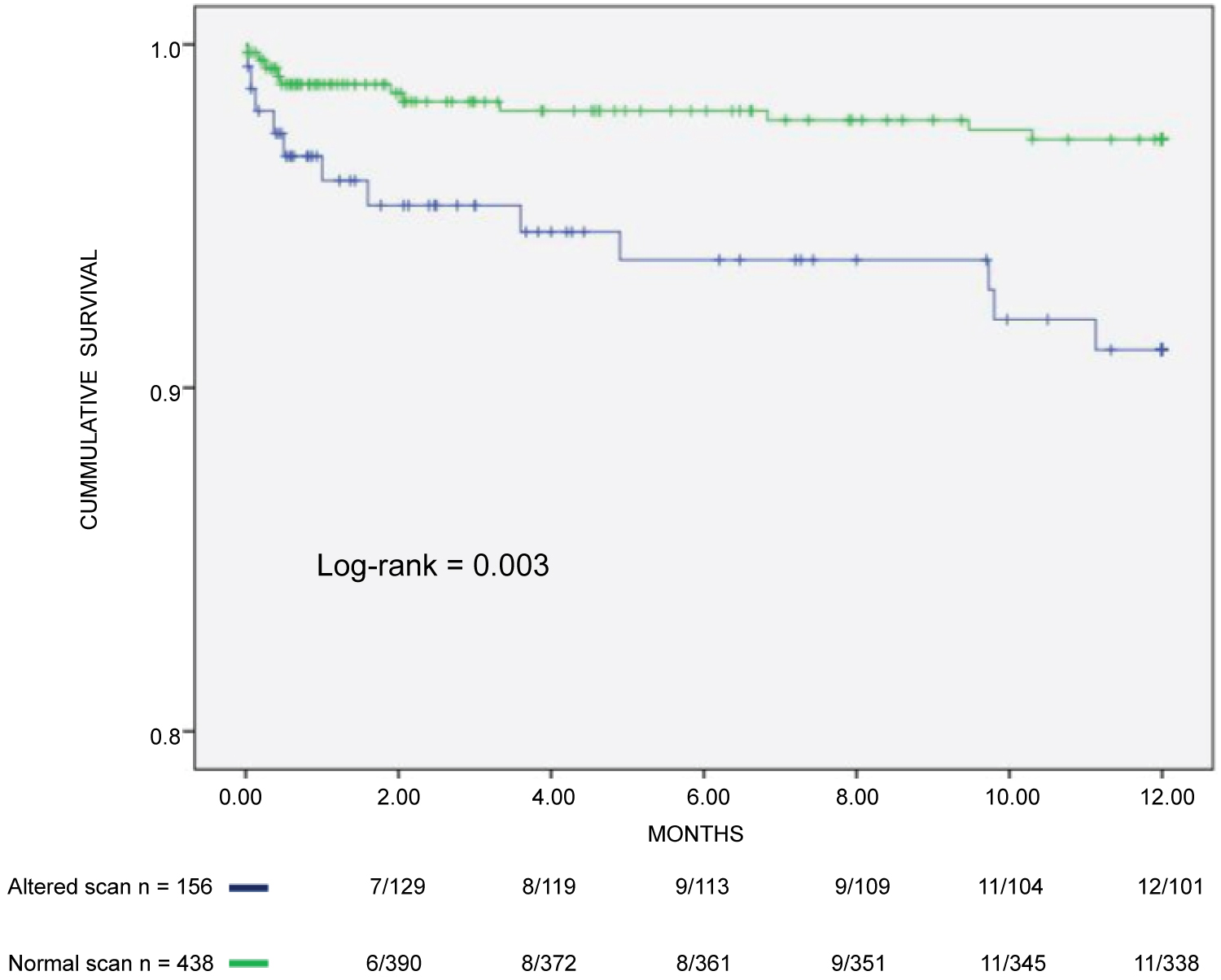 Figure 5: Incidence of cardiovascular death in CKD patients on hemodialysis assessed by myocardial scan.
View Figure 5
Figure 5: Incidence of cardiovascular death in CKD patients on hemodialysis assessed by myocardial scan.
View Figure 5
The purpose of our study was to verify the most significant risk factors present in patients on the renal transplant waiting list that may interfere with the incidence of major cardiovascular events and cardiovascular death during the first 12 months after transplantation using data from the pre-transplant workup. The identification of patients at higher risk would allow for better patient selection and also help to implement measures to reduce the incidence of CV complications during the early post-transplantation period. We found that the incidence of major CV events, observed during the initial post-transplant period, was predicted by age ≥ 50 years and variables associated with myocardial ischemia. Moreover, myocardial ischemia, as assessed by myocardial perfusion testing, was the sole predictor of cardiovascular death. These results suggest that patients with documented pre-transplantation myocardial ischemia should be considered at a higher risk of developing early CV complications and managed accordingly before, during, and after the transplantation. Because the endpoints in this study were the composite incidence of CV events and CV death, myocardial ischemia may be interpreted as a marker of atherosclerotic burden instead of ischemic heart disease considered in isolation.
In our series, the incidence of CV events was 8.4% during the first post-transplant year. Works that explored the incidence of CV events during the same time interval reported incidence that varied between 3.1 to 38% [11-16]. This marked difference may be caused by different criteria to define CV events. One the largest series so far, comprising 23,575 subjects, reported an incidence of 3.1% [15], but the endpoint was limited to coronary events. A French investigation reported an incidence of composite events close to 15% at 1 year, not very different from ours [16]. The relatively low incidence of CV complications in this study probably reflects the influence of our protocol on patient selection and the aggressive use of preventive measures during the initial post-transplant period. Our incidence of MI (2.8%) and unstable angina (1.2%) are among the lowest reported in the literature. However, that figure may have underestimated the real incidence of acute coronary syndrome because we ignore the cause(s) of sudden death in our patients.
The KDIGO [17] guidelines recommend cardiovascular evaluation in all renal transplant candidates with emphasis on the diagnosis and treatment of coronary artery disease. Myocardial perfusion studies are the preferred functional test for CAD and have been shown to be as good as coronary angiography at predicting future cardiovascular events in patients with chronic kidney disease [18], although its usefulness may be limited in patients at a higher risk of events [8]. Herein, we observed that myocardial ischemia, but not coronary artery disease assessed by angiography, predicts early CV events. There are at least two possible explanations for that fact. First, patients with more complex or multivessel coronary disease either underwent revascularization before transplantation, were excluded from the list, or died before being transplanted. Second, it is conceivable that the effect of CAD on prognosis can only be observed during longer periods of follow-up, as we have previously reported [19]. The high proportion of CAD in this study is probably a consequence of our diligent assessment of the disease based on risk, not only on symptoms.
In this work, most traditional risk factors were not predictors of events. This result is consistent with data from other studies [5,6,20,21]. For instance, the PORT study, a large multicenter investigation, observed that traditional modifiable CV risk factors were very poor predictors of cardiac events in patients with advanced CKD [15]. Indeed, traditional risk calculators validated in the general population, including the Framingham score, do not fully explain the increased incidence in CV events in renal transplant recipients [6,12].
The incidence of major CV events and CV death observed during the initial post-transplant period were predicted by variables associated with myocardial ischemia. These results suggest that patients with documented pretransplantation myocardial ischemia should be considered at a higher risk of developing early CV complications and managed accordingly before, during, and after the operation. The identification of patients at higher risk would allow for better patient selection and also help to implement measures to reduce the incidence of CV complications during the early post-transplantation period. It is also important to note that CV events were associated with a high rate of death, emphasizing the importance of MACE prevention in this group of patients.
This was a unicentric retrospective study. This study was conceived to estimate the risk of CV complications using data collected before kidney transplantation in patients on the waiting list. Therefore, the results presented here cannot be used to estimate the risk in patients already engrafted and also do not apply to patients who had survived the early post-transplant period. There were no prespecified criteria to refer patients for pretransplant CV evaluation. The number of patients removed from the list was not assessed. The decision to withdraw patients from the list was beyond the reach of the study team. We did not include data relative to electrolytes and metabolic/endocrine parameters, or inflammation markers with the potential to influence results. Although we took pains to enforce the use of cardioprotective medication, some adjustments had to be made by the physicians in charge due to side-effects.
1. Jose JG De Lima: Participated in research design, Participated in the writing of the paper, Participated in the performance of the research, Participated in data analysis.
2. Luis Henrique W Gowdak: Participated in research design, Participated in the performance of the research, Participated in data analysis.
3. Flavio J de Paula: Participated in research design, Participated in data analysis, Participated in drafting the manuscript.
4. Elias David-Neto: Participated in data analysis, Participated in research design, Participated in drafting the manuscript.
5. Luiz A Bortolotto: Participated in research design, Participated in data analysis, Participated in drafting the manuscript.