Introduction: Malignant neural sheath tumors located in the head and neck region are very rare. Surgical treatment if possible is the best option, trying to obtain wide resection margins free of tumor.
Objects: To determine the incidence of malignant tumors of neural histology, in relation to nerve tumors originating in the head and neck and description of two clinical cases.
Methods: A retrospective and descriptive study was carried out by reviewing the electronic medical records of all patients who were diagnosed and treated for neural histology tumors originating in the head and neck, between March 1998 and December 2021.
Results: Eighteen patients were treated for nerve tumors originating in the head and neck. The benign tumors of neural origin were located in the nasal cavity and paranasal sinuses (6/18) and in the neck (10/18). Four originated from the facial nerve in the parotid, three from the cervical sympathetic nerve in the retro styloid carotid space, one in the submaxillary region, and two in the supraclavicular fossa.
The incidence of malignant nerve tumors was 11.11% (2/18).
Conclusions: The incidence of malignant neural sheath tumors in our study was 11.11%. Most neural sheath tumors are benign and can cause functional alterations due to compression of the nerve of origin or adjacent structures, but when the neoplasm grows rapidly malignancy should be suspected. The main treatment is surgery trying to obtain wide tumor-free margins.
Malignant neural sheath tumors, Head and neck, Infraorbitary nerve, Endoscopic surgery
Malignant neural sheath tumors, Head and neck, Infraorbitary nerve, Endoscopic surgery Malignant neural sheath tumors (MNST) are an infrequent type of soft tissue sarcoma, they can originate from the cranial, peripheral or autonomic nerves.
They can be sporadic, originate in previously irradiated regions, or in patients with neurofibromatosis type 1.
Location in the head and neck occurs in 10 to 15% of cases and represents 10% of neck sarcomas.
It is difficult to make a presumptive clinical or imaging diagnosis prior to the cytological or histological study, but a sign of malignancy is the rapid growth of the tumor.
The best treatment is surgery, trying to perform complete resections with a wide margin if the location of the tumor allows it.
To determine the incidence of malignant tumors of neural histology, in relation to nerve tumors originating in the head and neck and description of two clinical cases.
A retrospective and descriptive study was carried out by reviewing the electronic medical records of all patients who were diagnosed and treated for neural histology tumors originating in the head and neck, between March 1998 and December 2021.
All patients had histological confirmation of neural sheath tumor by cytology or excisional biopsy. Patients with intracranial neural tumors were excluded.
Eighteen patients were treated for nerve tumors originating in the head and neck. Seven were women and eleven men. The youngest was 16 and the oldest was 82 years old, the average age was 41 years.
Fourteen had a histological diagnosis of neurilemmoma and two of solitary neurofibroma.
One patient had histopathological and another cytological diagnosis of malignant Schwannoma (2/18).
The benign tumors of neural origin were located in the nasal cavity and paranasal sinuses (6/18) and in the neck (10/18). Four originated from the facial nerve in the parotid, three from the cervical sympathetic nerve in the retro styloid carotid space, one in the submaxillary region, and two in the supraclavicular fossa.
The incidence of MNST was 11.11% (2/18).
1) Sixty-tree year-old woman consulted for a tumor on the left cheek, painful on palpation and with facial hypoesthesia on that side.
Nasal endoscopy was normal and Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) revealed a subcutaneous tumor without skin infiltration, 8mm in diameter with post-contrast enhancement. It was located at the emergence of the infraorbital nerve from the maxillary sinus (Figure 1).
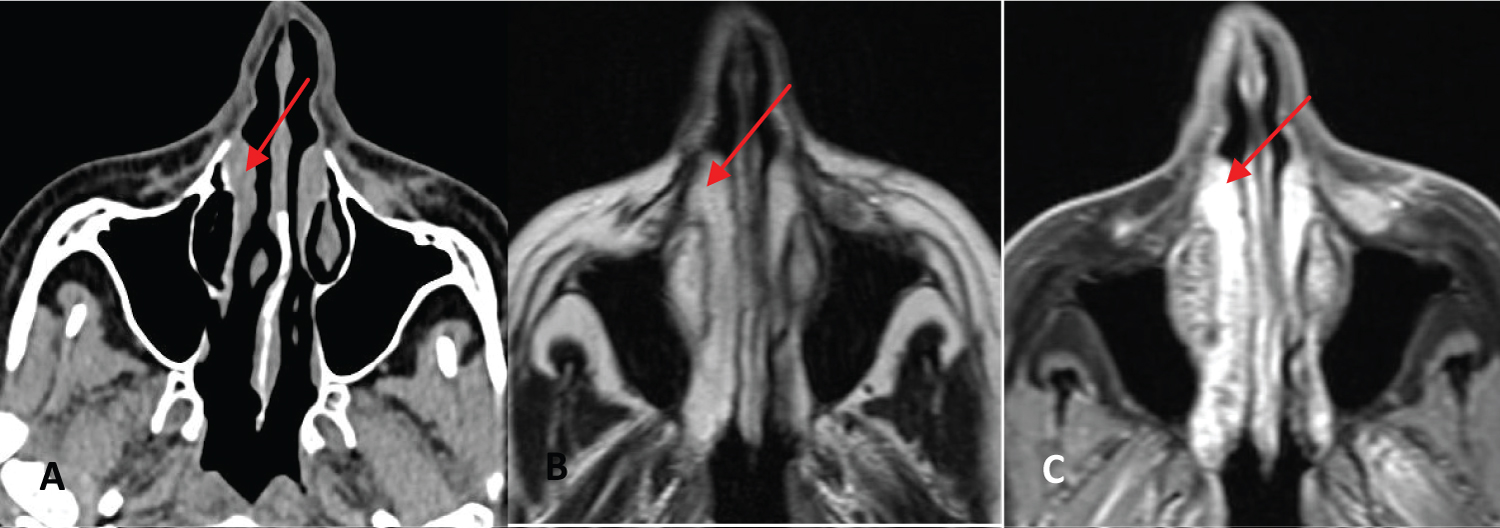 Figure 1: A: CT where a nodular lesion is observed adjacent to the emergence of the infraorbital nerve, B y C: Axial MRI in T1 and T2 showing a subcutaneous tumor without skin infiltration at the emergence of the infraorbital nerve (red arrows).
View Figure 1
Figure 1: A: CT where a nodular lesion is observed adjacent to the emergence of the infraorbital nerve, B y C: Axial MRI in T1 and T2 showing a subcutaneous tumor without skin infiltration at the emergence of the infraorbital nerve (red arrows).
View Figure 1
A sublabial approach and an anterior maxillary sinusotomy were performed, resecting the tumor that was attached to the infraorbital nerve, which could be preserved.
The intraoperative biopsy was reported as a lesion consisting of spindle cells with atypia, so it was decided to resect the nerve until it entered the pterygomaxillary fossa and the surrounding premaxillary soft tissue (Figure 2).
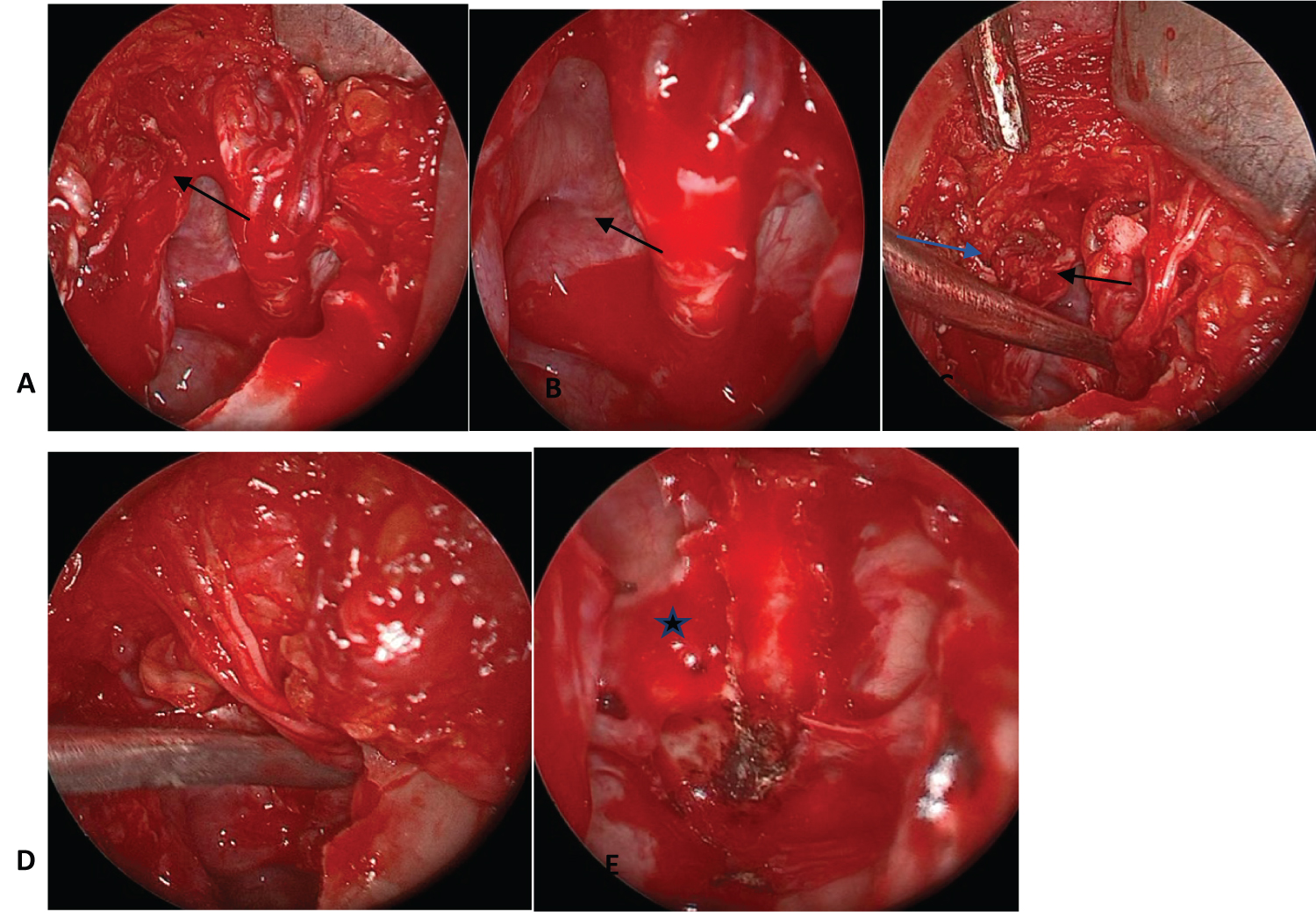 Figure 2: Endoscopic view of the sublabial approach and anterior maxillary antrostomy.
Figure 2: Endoscopic view of the sublabial approach and anterior maxillary antrostomy.
A y B: infraorbital nerve tumor (black arrows), C: infraorbital nerve tumor dissection for intraoperative histological study (black arrow: infraorbital nerve, blue arrow: tumor), D: infraorbital nerve after tumor resection, E: the bony canal of the infraorbital nerve is observed in the orbit floor after nerve resection until its entry into the pterygomaxillary fossa (⋆).
View Figure 2
The postoperative histopathological study was reported as a malignant spindle cell neoplasm compatible with malignant Schwannoma and immunostaining was negative for ERG, MYOD-1, CK 818, Desmin, p40, HMB45, Melan A and positive for S100 and diffuse positive for SOX10.
It was diagnosed that the sector of the infraorbital nerve that was resected in the roof of the maxillary sinus had neoplastic infiltration.
Positron emission tomography did not detect pathological uptake in other body sites. A new surgery was indicated to widen the margins of the previous surgery.
By a trans nasal approach with endoscopes, a wide median antrostomy with resection of the pterygoid process and the posterior wall of the left maxillary sinus were performed.
The superior maxillary branch of the trigeminal nerve (V2) was resected together with the fat from the pterygomaxillary fossa, preserving the mandibular ramus (V3) (Figure 3).
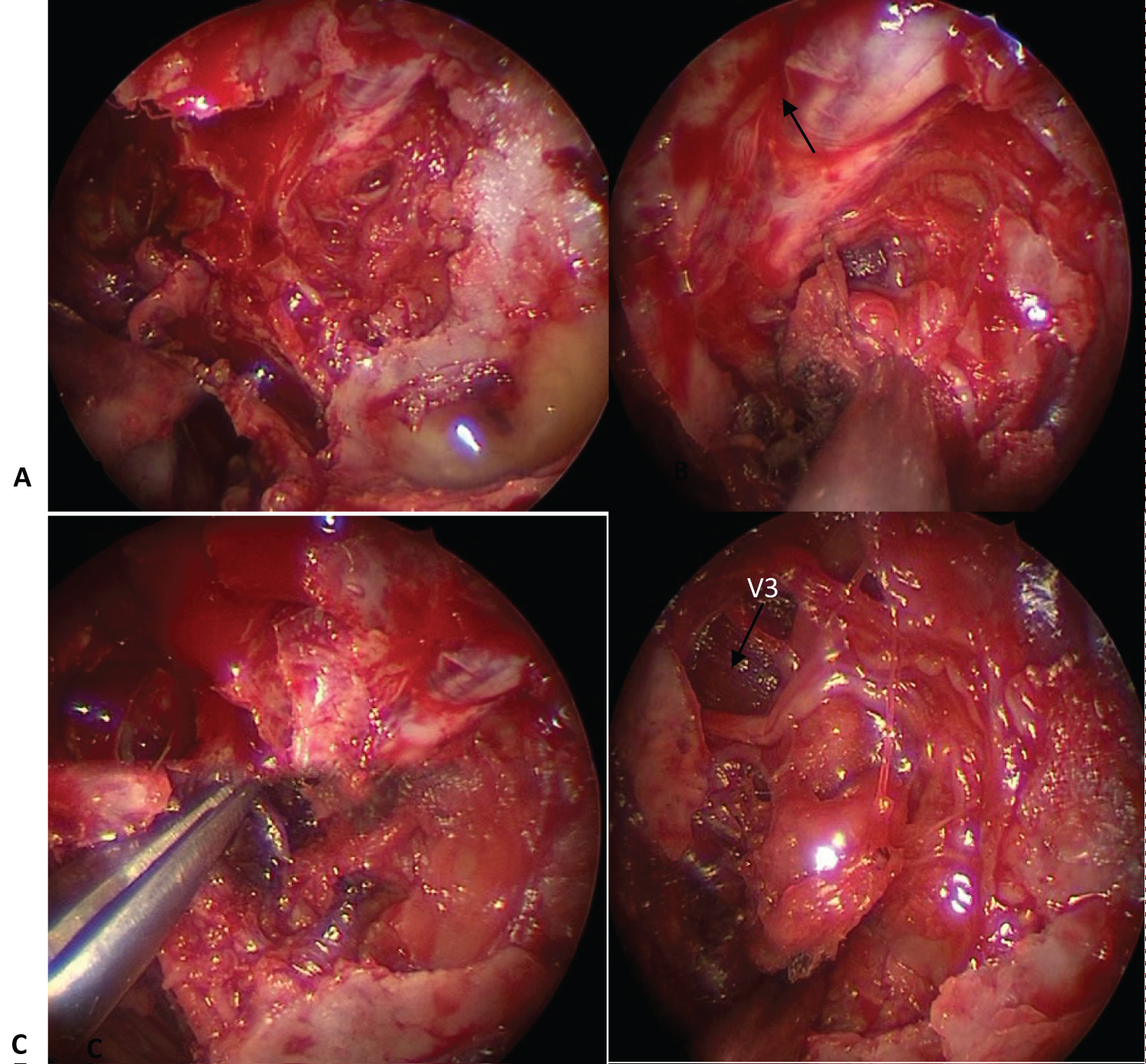 Figure 3: Endonasal approach with endoscopes to the maxillary pterygoid fossa (MPF).
Figure 3: Endonasal approach with endoscopes to the maxillary pterygoid fossa (MPF).
A: pterygoid process and posterior wall of the maxillary sinus resection to access the MPF,
B: MPF dissection showing the orbital cone (arrow) and the pterygoid muscles, C: V2 resection,
D: V3 preservation (arrow)
View Figure 3
The histopathological study of the resected tissues did not diagnose neoplasia.
Forty days later, a nodular lesion was detected on the left cheek. The cytology of the lesion was compatible with malignant spindle cell neoplasia. MRI revealed a subcutaneous nodular lesion without skin infiltration.
An excision of the skin and soft tissues of the cheek was performed with a 1cm margin of healthy tissue. The defect was reconstructed with a Mustardé flap.
She received postoperative treatment with intensity modulated radiotherapy with a dose of 5500cgy (Figure 4).
 Figure 4: Subcutaneous tumor resection and Mustardé flap reconstruction (A, B, C, D), E, F: postoperative
In the imaging controls, no recurrences were detected during the short follow-up period (6 months).
View Figure 4
Figure 4: Subcutaneous tumor resection and Mustardé flap reconstruction (A, B, C, D), E, F: postoperative
In the imaging controls, no recurrences were detected during the short follow-up period (6 months).
View Figure 4
2) 82-year-old man consulted for a rapidly growing lateral right neck tumor in recent months and dysphonia. He had consulted 8 years earlier for the same tumor, which at that time was smaller in size, and he refused surgical treatment. The cytology at that time was reported as elements of a cystic area without atypia, and the images showed that the neoplasm was compatible with a neurilemmoma.
Videostroboscopy of the larynx revealed right vocal cord paralysis and the MRI revealed an extensive lateral right neck tumor measuring 104 x 96 x 78mm in its craniocaudal, anteroposterior, and transverse diameters, located in the carotid space with a multicystic appearance and peripheral enhancement with contrast.
It displaced the internal and external carotid arteries forward and the jugular vein laterally (Figure 5).
 Figure 5: MRI: Coronal (A) and axial (B) slices showing an extensive neoplasm in the neck with a multicystic appearance with post-contrast enhancement.
View Figure 5
Figure 5: MRI: Coronal (A) and axial (B) slices showing an extensive neoplasm in the neck with a multicystic appearance with post-contrast enhancement.
View Figure 5
Puncture under ultrasound was reported as malignant spindle cell neoplasm and immunostaining was negative for S100, SOX10, CD33, leukocyte common antigen, CD1-A, CK, and Desmin.
Due to the clinical and imaging characteristics, it was compatible with malignant Schwannoma. PET diagnosed multiple metastases in the pleura, lung, liver, and bone (Figure 6).
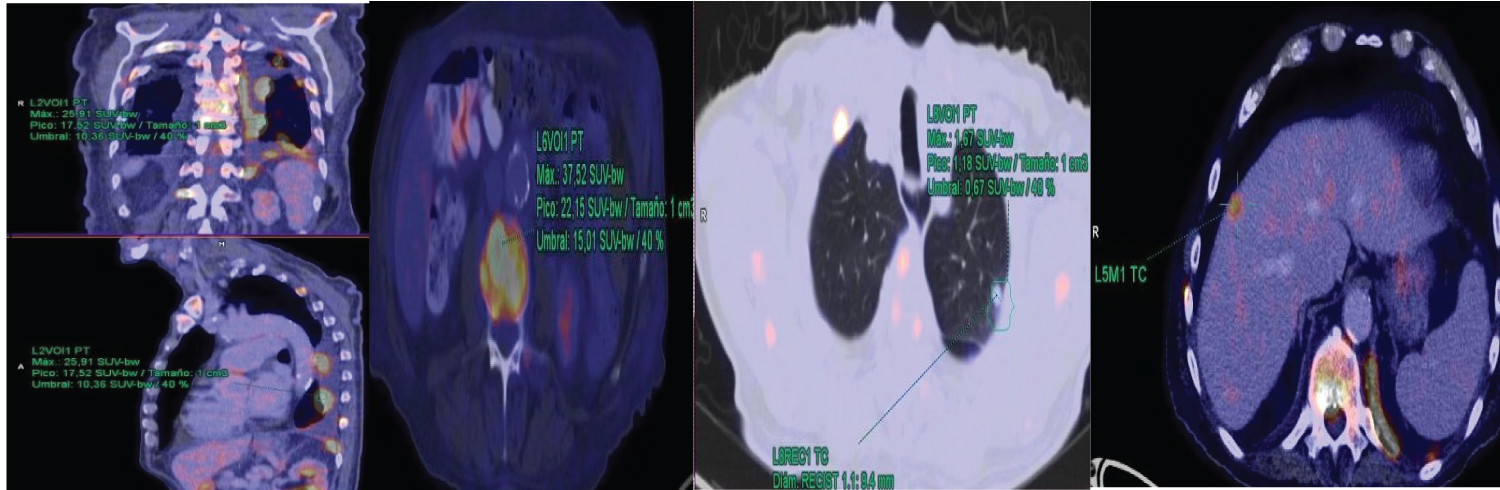 Figure 6: PET-CT: multiple metastases in bone, pleura, lung and liver.
View Figure 6
Figure 6: PET-CT: multiple metastases in bone, pleura, lung and liver.
View Figure 6
Palliative treatment was indicated.
Malignant neural sheath tumors of peripheral nerves comprise a group of neoplasms that can differentiate into various elements of the neural sheath, including Schwann cells, perineurial fibroblasts, and fibroblasts [1].
Within this group are malignant schwannomas, neurofibrosarcomas and neurogenic sarcomas [2].
MNST are rare, they represent between 5 to 10% of soft tissue sarcomas and have an incidence of 0.001% [3]. They can originate in three contexts: sporadic in approximately half of the cases, associated with type 1 neurofibromatosis, or they can be induced by previous radiation treatments [2,4].
Sporadic malignant neural sheath tumors occur more frequently in elderly patients and those induced by radiation are more common after radiation treatment of breast pathologies or lymphomas with a mean latency time of 15 to 16 years [5].
Boumaza, et al. [6] reported the results of 73 patients who were treated over a 20-year period for tumors of neural histology located in the neck. Forty-four were Schwannomas, 22 neurofibromas, 3 neuroblastomas, and two had malignant neural sheath tumors (3%).
One was a sporadic neurofibrosarcoma and the other originated from a malignant transformation in a patient with neurofibromatosis type 1.
In another study [7] they reported one malignant Schwannoma among 52 head and neck neurilemmomas treated over a period of 8 years (1.92%).
Most neural tumors located in the nasal cavity and paranasal sinuses are benign. Malignant neoplasms are exceptional, with 30 to 40 cases described in the literature [8].
In a review of 430 cases of non-epithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx, they reported only 4 cases of MNST [9].
In our study, the incidence of MNST was higher than that described in the literature (11.11%).
The two described cases of malignant nerve neoplasms were sporadic, one had an initial diagnostic of MNST and the other originated from a benign Schwannoma in an 82-year-old patient who had rejected surgery 8 years earlier
MNST are very aggressive tumors with a poor prognosis.
Survival at 5 years is between 32 to 52% or 50% in sporadic tumors [6].
Factors associated with a poor prognosis include tumor size > 5 cm, positive resection margins, advanced age, initially diagnosed metastases, and type I neurofibromatosis-associated tumors.
In one study, they included the location of tumors in the head and neck as a factor of poor prognosis [10].
The main treatment of MNST is surgical, with the objective of obtaining free resection margins.
Adjuvant radiotherapy can be used to assist surgery in the local control of the disease when the resection margins cannot be wide due to the location of the tumor or when these are positive.
In the patient with malignant Schwannoma of the infraorbital nerve, postoperative radiotherapy was indicated despite the fact that the resection margins were free of disease due to the proximity of the tumor to the skull base and to the eye.
Yao Xu, et al. [10] reported that overall survival did not improve with the addition of radiotherapy to surgical treatment.
The reported incidence of metastases in MNST located in the head and neck and other sites was 14.3% (109/764) [10].
The second patient described in our study with a MNST in the neck had multiple distant metastases associated with rapid tumor growth 30 days before the consultation.
The role of systemic treatment with chemotherapy in MNST is controversial [11].
The incidence of malignant neural sheath tumors in our study was 11.11% (2/18).
Most neural sheath tumors are benign and can cause functional alterations due to compression of the nerve of origin or adjacent structures, but when the neoplasm grows rapidly malignancy should be suspected.
The main treatment is surgery trying to obtain wide tumor-free margins.
We declare no conflicts of interest