Frailty is a geriatric syndrome related to adverse health outcomes in the elderly, due to a decrease systems' functional reserve. Cancer is a common pathology in the elderly, and we need tools for identifying the response to treatment and prognosis of elderly cancer patients. This short revision aims to assess the significance of the detection of frailty in the elderly patient with a tumor as a possible prognostic factor in terms of mortality, and the impact of the 2013 Frailty Consensus in the research activity.
A review of the literature from 2013 (when an International Consensus on frailty was published) to 2016 was made, choosing works that used some of the frail scales proposed by the consensus and had mortality results with a correct description of the stadistic analysis.
15 papers were selected, finding an increased mortality risk in frail older people (OR from 2.07 to 12.5). The number of papers related to frailty in cancer patients increased from 1 in 2013 to 10 in 2015.
Frailty must be detected in old cancer patient as a potential prognosis factor that can help in choosing the better treatment. The impact of this entity in publications is growing since the International consensus of 2013, but further research must be made to establish a gold standard for the detection of the syndrome, and analyze all the consequences of frailty in the evolution and prognosis of cancer.
Frail elderly, Neoplasms, Mortality, Risk
Frailty is a syndrome related to adverse health events and an increased risk of mortality and morbility [1]. As a result of an older population, we can find a higher number of frail patients. Frailty is more common in older people, and it is associated with sarcopenia (although they are different entities) [2] and cardiovascular risk [3]. Frail patients present disability more frequently than nonfrail people, and need more social attention [4].
Cancer is frequent among older patients. About the 60 per cent of the new diagnosis of cancer is set on people over 65-years-old, and the 30 per cent in patients that are 75 or older [5].
Elderly are more likely to present neoplasias due to loss of function of the different cell molecular structures. This is often reflected in cell atrophy, but also in the loss of the ability to keep the genome stable, producing mechanisms that contribute to uncontrolled cell proliferation both in molecular and tissue levels. In this way, we can understand cancer as an age-related illness [6], which shares the pathophysiological mechanisms of frailty in relation to the loss of molecular functions.
In 2013, a group of international experts remarked the importance of frailty as a predictor of outcomes, and a measurement of the "biological age" of the individuals. Frail individuals have a lower life expectancy. They recommended the use of well validated scales as FRAIL scale, the Groningen Frailty Indicator (GFI) or the Canadian Study on Health and Aging Frailty Index (CSHA), among others [7].
The presence of frailty can be a determining factor in the response of an elderly cancer patient to the various treatments and the associated morbidity, as well as in the survival rates. This short revision aims to assess the significance of the detection of frailty in the elderly patient with a tumor as a possible prognostic factor in terms of mortality. Moreover, the impact on publications of the recommendations made by the international experts on geriatrics in 2013 will be examined.
A revision of the literature published from 2013 to May of 2016 about this subject has been made, in order to analyse the importance of frailty as a prognosis factor in cancer.
A Medline search strategy was developed, by using the search form "cancer" AND "frailty" AND "mortality", and applying special criteria for searching just the publications from 2013 to 2016, so the impact of the recommendations of the International Geriatrics Societies in 2013 can be analysed.
Publications needed to meet specific criteria for being considerate. They should use some of the scales proposed by the international consensus in 2013 for measure frailty: Groningen Frailty Index (GPI), modified Frailty Index (mFI), Fried criteria, Frail scale, Canadian Study on Health and Aging Frailty Index (CSHA), Gerontopole Frailty Scale [7].
Articles must contain mortality results related to neoplasias in the elderly. Furthermore, statistics must be defined properly, giving and odds ratio (OR) or similar with a p value if possible. Confidence interval was not an essential criteria, but studies without it were remarked to signal the deficit.
Prospective and retrospective studies were included if they complied with the eligibility criteria.
The reading of the title and the abstract of all the results of the search was made, proceeding to read the complete articles specific on cancer on the elderly that complied the exposed criteria. The review was made by two independent investigators, resolving the conflicts by consensus.
The selected studies were classified depending on the publication year and the treatment applied to patients, as well as if they were general studies on cancer or related to any specific neoplasia. Characteristics as if they were prospective or retrospective, the sample size and the odds or hazard ratio with p value and confidence intervals were extracted. The kind of treatment received by patients and the frailty scale employed were recorded.
The principal outcome measured was mortality among frailty patients. Results on morbidity or response to treatment were analysed too.
Statistics: no statistic analysis could be made, due to the differences between the works in terms of sampling and objectives. A descriptive analyse was made, resuming the results of the publications.
Study selection: a PRISMA diagram explains the flow of the studies through the review (Figure 1). 232 articles were found, but just 19 papers examined frailty in oncology patients following one of the scales proposed by the International Consensus. Three of them measured toxicity, polypharmacy, morbidity or response to treatment, not mortality. Another one was discarded as in its result there was no odds ratio or similar parameter.
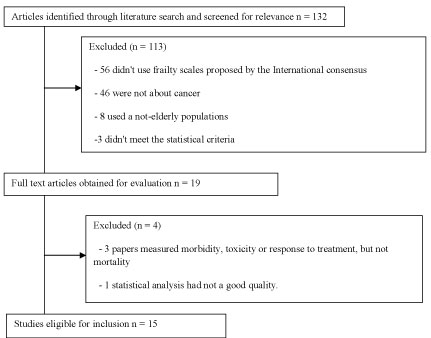 Figure 1: PRISMA diagram explaining the flow of the studies through the review. View Figure 1
Figure 1: PRISMA diagram explaining the flow of the studies through the review. View Figure 1
Characteristics of the included studies are presented in Table 1 [8-22]. 5 studies had less than a hundred participants [10,15,18,20,22], 6 between a hundred and a thousand [11,12,14,19,21], and 5 more than this [8,9,13,16,17]. The population of three studies had any type of cancer [12,14,17], two urologic neoplasias [8,13], six digestive-related cancer [9,10,19-21], one was not specific but excluded skin cancer [11], another talked about lymphoma [18], one included neoplasias of the head, neck and skin [13] and two studied patients with gynaecological cancer (breast [22] or any other [16]).
Table 1: Studies selected and its principal characteristics. View Table 1
Four studies measured frailty thought the Modified Frailty Index from the Canadian Study on Health and Aging Frailty Index and sarcopenia [8,9,14,16], and another used this scale and the Short Physical performance Battery [20], The Groningen Frailty index (GFI) was used by six research groups [12,15,18,19,21,22], one used this index and the Timed up-and-go test too [10], and one else employed this tool combined with other measures [19]. The Canadian Study on Health and Aging Frailty Index was used in one publication [13], as well as the non-modified Frailty Index [11]. One of the studies used various frailty scales to identify frail and prefrail patients [17].
Frailty was associated with a higher risk of mortality in all studies but three of them. The Groningen Frailty Index failed to alert from mortality in two studies [10,15], and the modified Frailty Index in one [19]. The increased mortality risk goes from de 2.07 [8] to 12.5 [16].
Some of the works accepted measured other outcomes as ICU admission [20], or morbidity related to the cancer process [16,17], as well as response to treatment [18]. In all cases, frailty was a predictor of a worse evolution of the neoplasia.
The number of articles about the studied subject increased significantly from 2013 to 2015, from one investigation [22] to ten [9-19] each year.
This revision has shows, as previous work, that frailty is clearly associated with higher mortality in old cancer patients [23]. Nevertheless, as there is no common standard for a frailty definition [4], studying the real impact of this entity among old cancer patients is quite complicated. In general, it is recommended to make a screening for frailty in older patients with oncological diseases, but the available frailty screening tools have not enough discriminative power to be useful in further assessment [24].
Frailty is a complex syndrome that must be suspected by geriatricians, family or general doctors [4], who usually knows better the patient, as it is a dynamic situation. It is important for oncologist, when the cancer diagnosis is made, to be assessed by other specialist on the patient way of live and the evolution of his health and functional abilities in the last years, in order to understand the possible implications of aging and frailty in the healing process. This complex procedure that includes physical, psychological, mental, functional and social evaluation of the elderly is called "geriatric assessment" [25].
Frailty represents an easy way of understanding the prognosis of a patient, as it is related with the functional reserve of the different organs and systems. A frail patient will not elaborate an appropriate answer to stress factors, so the homeostasis will be broken and disease, mortality or any other adverse health outcome will take place [1], as it has been demonstrated in this review.
This syndrome is related to sarcopenia and disability, although they are not synonyms. Understanding the frailty level of a patient is an easy way of evaluate the general status of the elderly within a few minutes [4]. The problem arrives when we have to choose one of the existing frailty definitions.
There are two approximations to frailty. In one hand, authors like Fried, et al. define frailty as a phenotype, so it can be found in patients who gather some symptoms and signs as slow gait speed, low grip strength, decreased aerobic capacity, fatigue and/or weight decrease [7]. It is necessary to know the parameters of the studied population, so we can compare the results of the physical examination of our patient with them. Furthermore, a dynamometer is needed to obtain all the parameters of the phenotype definition. Theses drawbacks do not ease the application of the phenotype definition of frailty. In this revision, just two papers used phenotypic definitions of frailty [10,22].
On the other hand, authors like Rockwood have developed frailty scales from an addition of physical, mental, psychological and social deficits. Is the case of scales like the one of the Canadian Study on Health Aging group (CSHA), the modified Frailty Index (mFI) or the Groningen Frailty Index (GFI) [7]. One of the most important difficulties of these scales is that one of the deficits can explain the outcomes by itself, and these tools give the same prediction capacity to items as different as ischemic heart disease or widowhood in some cases. Nonetheless, most studies of this revision have used an accumulation of declines definition [9,11-19,21,22].
Three years ago, an International Consensus on frailty was proclaimed, trying to underline the importance of this entity and encouraging researches to examine the real impact of this syndrome in the different pathologies [7]. As a result, and as is showed in this paper, the number of publications has increased. Most of this publications use frailty within the addition of deficits definition.
There is a third way of defining frailty. The FRAIL scale mixes aspect from the phenotype and the addition of deficits definition. Through five questions (four about fatigue, aerobic capacity, strength and weight loose and one about number of a defined classification of illnesses) can determine if an individual meets the criteria for frailty, is not frail or can be classified in an intermediate state called "prefrailty" [26]. No works have been found that use the FRAIL scale as a prognosis tool for cancer patients.
Frailty has been related with and increased risk for mortality and morbidity derived from neoplasias and its treatment [8,10-12,14-22]. This result is consistent with studies in other pathologies [1], as cardiovascular diseases [3]. Frailty maximizes the cardiovascular risk through the generation of an increased trend to inflammation, and a decreased muscle mass that carries to insulin resistance. Inflammation provided by cancer can be added to the one derived from frailty, and produce a higher number of adverse health outcomes [6]. Nevertheless, the physiological influence of frailty and its metabolic ways must be defined in cancer patients.
Old patients have an immune system that does not react properly to infection. Cancer patients have a greater risk of infection due to the loss of immune response and to the suppression of it secondary to the treatments. Frailty is related to immunosenescence what means that frail people will respond worst to infection and its treatment if presented, because their immune system can no longer attack the microorganisms as well as it did before [27,28]. This can be part of the reason of the increased mortality and morbidity among old frail cancer patients.
Only three works were not compatible with the increased mortality and morbidity associated with frailty. The study led by Bras' population included only patients with neck, head and skin neoplasias [15]. This neoplasias are not very common among elderly, and are infrequent in general population, so results are not quite representative of the elderly population and other risk factors might be associated with this type of cancer. Buettner, et al. designed an study that tried to describe the potential of sarcopenia in predicting risk of mortality in elderly cancer patients, adding this prediction power to frailty. They demonstrated that frail and sarcopenia individuals with sarcopenia suffer more complications and have a higher one-year mortality than frail non-sarcopenic people [9]. As sarcopenia ad frailty are related, when we identify frail people with lower muscle mass we are selecting a group with higher risk of adverse outcomes , because they have two different syndromes that are related to mortality, morbidity and disability by themselves [2]. Ugolini, et al. didn't find connection between frailty (by using the Groningen frailty Index) and mortality10, but they did with the Timed up-and-go test, which is considered an executive function test related to frailty [7].
Frailty is a geriatric syndrome that should be taken into account when deciding the treatment in elderly cancer patients. As this entity is firmly related to increased mortality and morbidity, as well as poorer response to treatment, frailty must be checked in every old patient as a tool to decide the options of recovery, and consequently the best way to treat the neoplasia.
Although most cancer-related studies use the accumulation of deficits definition of frailty, it is possible that combining it with the phenotype definition increases the capacity of prediction of this syndrome, in terms of mortality, morbidity or response to treatment. Further research must be done in this field.
Since the publication of the Consensus on Frailty, many work on frailty has been developed. The importance of this syndrome is growing, and it is being subject of research in different fields, like cancer, due to its potential implications in the management of the patient because of the prognosis value it has in terms of life expectancy and response to treatment.