This was a cross-sectional study carried out in Rivers State University Teaching Hospital, Port Harcourt with the aim of determining the Changes in Haemostatic Parameters in Pregnancy and puerperium. A total of 500 age-matched apparently healthy women of reproductive age, which consisted of 200 (40%) pregnant women, 200 (40%) puerperium mothers and 100 (20%) non-pregnant women who served as controls were studied. Their ages ranged from 16 to 41 years (mean 27.4 ± 4.3 years). The Platelets count, prothrombin time (PT), partial thromboplastin time with kaolin (PTTK) and fibrinogen concentration were determined using Standard Manual Techniques. Platelets count was carried out as described by Bain and Seed, PT and PTTK by Quick's methods while modified Clauss Method was used in the determination of Fibrinogen concentration. The pregnant women had significantly lower values of platelet count, 203.89 ± 65.2 × 109/L (range, 78-416) as compared to 257.0 ± 69.0 × 109/L, (range, 90-396 × 109/L,) of the non-pregnant subjects and the 249.1 ± 75.0 × 109/L, (range, 95-406 × 109/L) of the puerperium women (F = 28.437; P < 0.05). The prevalence of thrombocytopenia among the pregnant, puerperium mothers and non-pregnant control women were 53(26.5%), 15(7.5%) and 12(12.0%) respectively. The mean PT, 15.48 ±2.49 seconds (range, 14-16 seconds) of the non-pregnant control women were significantly higher than the mean PT, 11.36 ± 3.12 seconds (range, 10-16 seconds) of the pregnant women and the 14.28 ± 4.22 seconds (range, 13-16 seconds) of the puerperium women (F = 57.843; P < 0.05). The international normalized ratio (INR) of the pregnant women as compared to the non-pregnant and puerperium women were not statistically significant (F = 2.206; P > 0.05). The mean PTTK of the pregnant women, 44.1 ± 7.2 seconds (range, 43.3-46.1 seconds) were significantly higher than the PTTK of the non-pregnant women, 39.4 ± 8.1 seconds (range, 38.4-44.3 seconds) and the puerperium women, 40.32 ± 6.4 seconds (range, 41.3-43.3 seconds) (F = 20.512; P < 0.05). The mean fibrinogen concentration, 4.4 ± 0.80 g/L (range, 2.9 -5.1 g/L) of the pregnant women were significantly higher than the mean fibrinogen concentration, 3.6 ± 0.88 g/L (range, 2.8-4.4 g/L) of the puerperium women and the non-pregnant control women, 2.6 ± 0.72 g/L (range, 2.6-4.3 g/L) (F = 164.877; P < 0.05). The results point towards a hypercoagulable state in pregnant women, which is normal during pregnancy.
Haemostatic parameters, Puerpurium, Pregnancy
Pregnancy is a period of time between fertilization of the ovum by a spermatozoon (conception) and birth during which women carry their developing fetus in the uterus [1]. Normal pregnancy is estimated to last approximately between 38 and 42 weeks and is usually divided into three trimesters, namely first, second and third trimesters. The puerperium is the period spanning the first six weeks of delivery of the baby and placenta [2,3], when all the systems in the woman's body would have recovered from the effects of pregnancy and returned to their non-pregnant state.
These periods are characterized by several physiological alterations especially the components of the haemostatic system; which have to be taken into account before assessing any significant deviation from the ordinarily accepted normal blood values.
Haemostasis may be defined as a group of protective and integrated physiological processes by which blood is kept in the fluid state, haemorrhage is arrested and vascular patency is restored when necessary through clot dissolution. The haemostatic process which retains the blood within the vascular system basically consists of two steps, primary and secondary haemostasis [4]. In primary haemostasis, there is platelet adherence to the subendothelial matrix and aggregation, whereas, in secondary haemostasis, there is activation of the coagulation cascade, culminating in the activation of thrombin which then converts soluble plasma fibrinogen to fibrin resulting in local fibrin deposition [5].
When there is injury to the blood vessel there is a complex chain of events which includes vasoconstriction, platelet adhesion, platelet aggregation, platelet plug formation and subsequent blood coagulation to form a haemostatic plug. In other words, normal haemostasis is a complex interaction between the vessel wall and components of the blood which prevents excessive blood loss after vascular damage while maintaining a viable circulation by preventing thromboembolic conditions [6].
A bleeding tendency occurs when there is an injury and deficiency of clotting factors and platelets, inhibition of coagulation processes or excessive activity of the fibrinolytic system [7]. The essential role of the haemostatic system is a rapid response to the site of vascular injury in such a way that the effect is confined to the site of injury and the bleeding arrested. This is necessary to prevent further damage to the system.
However, even normal pregnancy is associated with a range of alterations to this haemostatic balance in such a way that the procoagulant effect becomes dominant, leading to a hypercoagulable state. Hypercoagulability is the state secondary to an increase in the concentrations of procoagulant factors, a reduction in the concentrations of the naturally occurring anticoagulant proteins and a decrease in fibrinolysis [8,9] that are associated with a predisposition to venous thrombosis. Venous stasis resulting from the gravid uterus combines with alterations in coagulation factors make pregnancy a hypercoagulable state.
Placental insufficiency which may occur due to thrombosis of placental blood vessels, may lead to repeated or recurrent miscarriages, stillbirth, intrauterine fetal growth retardation, pre-eclampsia, preterm delivery, and an increased incidence of thromboembolic phenomena in the pregnant woman [7,10]. In addition, a variety of haemostatic disorders can arise in the pregnant woman, ranging from the acute catastrophe of amniotic fluid embolism, with massive intravascular coagulation and haemorrhage, to the low-grade process of intravascular coagulation which occurs in pre-eclampsia, leading to maternal morbidity and mortality.
This research work was a cross-sectional study carried out on 500 apparently healthy women of reproductive age. They consisted of 200 pregnant women, 200 mothers in puerperium and 100 non-pregnant women. The pregnant women were attending the antenatal clinic at the Rivers State University Teaching Hospital, Port Harcourt. The mothers in puerperium were those who successfully delivered their babies without complications. The non-pregnant control women were age-matched female members of staff and students of the Rivers State University, Port-Harcourt and female members of staff of the Rivers State University Teaching Hospital, Port-Harcourt. The bio-data and medical history of each of the apparently healthy pregnant subjects who were attending the antenatal clinic at the Rivers State University Teaching Hospital, were obtained. All the participants were age-matched and were randomly chosen.
Apparently healthy women of reproductive age with no history of coagulation complications, or pregnancy induced hypertension. The bio-data and medical history of the subjects were obtained from their case notes. The women who were not apparently healthy, with history of coagulation complications or pregnancy induced hypertension or with obstetric disorders and those who did not give their informed consent were excluded.
Each of the participants of this study gave informed consent to participate and the study was approved by the ethical committee of Rivers State University Teaching Hospital, Port-Harcourt.
Five point five millilitres (5.5 ml) of venous blood sample was collected from each participant, of which 4.5 ml of the blood was added into a glass tube containing 0.5 ml of 32.0 g/l trisodium citrate solution and mixed for the determination of prothrombin time (PT), partial thromboplastin time with kaolin (PTTK) and fibrinogen concentration while 1.0 ml of the blood was added to dipotassium ethylene diamine tetra-acetic acid (EDTA) plastic microcontainer to the final concentration of 1.5 mg/ml and mixed for the determination of platelet number. The blood samples in the citrated containers were centrifuged at 2,500 g for 15 minutes and the plasma was separated into plastic containers for the analysis of prothrombin time (PT), partial thromboplastin time with kaolin (PTTK) and fibrinogen concentration, in the same day of sample collection or kept frozen at -20 ℃ before analyses.
Determination of Platelet Count (Manual Technique) was done as described by Bain and Seed (2006). The principle is based on 1 in 20 dilution of the whole blood with a filtered solution of 1% ammonium oxalate reagent which lyses the red cells leaving the platelets intact to be counted microscopically using an Improved Neubauer Counting Chamber and expressing the number of platelets counted per litre of whole blood.
Prothrombin time (PT) Determination (Quick Method) was done using Giesse Diagnostics Reagent Kit (Italy). Prothrombin time (PT) is the time in seconds required for citrated plasma to clot at 37 ℃ when tissue thromboplastin and calcium are added.
Partial thromboplastin time with kaolin (PTTK) test was determined using commercially prepared reagents obtained from CYPRESS Diagnostic Reagents Limited, Italy. In this kit cephalin, a brain lipid extract served as a platelet substitute. Micronised silica served as an activator of the contact factors XI and XII.
The determination of plasma fibrinogen level using the Giesse Diagnostics Reagent Kit (Italy) is a modified Clauss method based on thrombin clotting time. It is therefore known as the thrombin clotting time fibrinogen assay. The principle is based on dilution of citrated plasma which is mixed with an excess of thrombin and the coagulation time determined. The required time for clot formation in dilute plasma is inversely proportional to the fibrinogen concentration. The plasma dilution permits to minimize interferences of anticoagulants like heparin.
Student's t-test was used to compare the haemostatic parameters of pregnant and non-pregnant subjects. One-way analysis of variance (ANOVA) was employed to determine the effect of trimesters and age groups on haemostatic parameters. One sample t-test was used to assess the effect of biological age on haemostatic parameters and to check the effect of parity on haemostatic parameters. While Product moment correlation coefficient was used to assess the correlation between plasma fibrinogen and other variables.
A total of 500 age-matched apparently healthy women of reproductive age, which consisted of 200 (40%) pregnant women, 200 (40%) puerperium mothers and 100 (20%) non-pregnant women who served as controls were studied (Figure 1). Their ages ranged from 16 to 41 years (mean 27.4 ± 4.3 years).
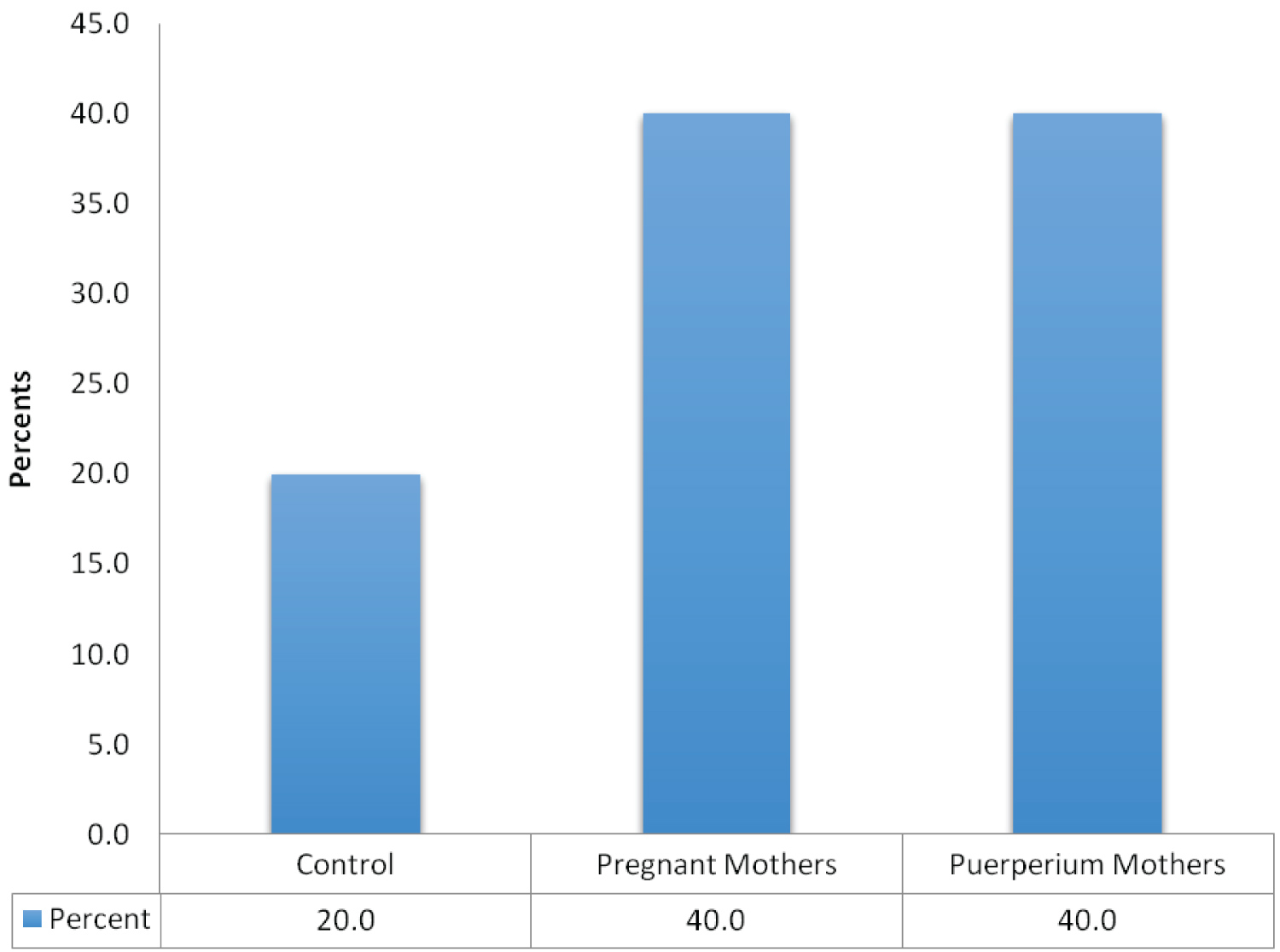 Figure 1: Frequency distribution of all the women studied.
View Figure 1
Figure 1: Frequency distribution of all the women studied.
View Figure 1
Analysis of Variance (ANOVA) was used to test the influence of Demographic and Haemostatic parameters of the Pregnant, Non-pregnant and Puerperium women. Table 1 shows the comparison of the demographic and haemostatic parameters of the pregnant, non-pregnant controls and the puerperium women, in which their mean ages is not statistically significant (F = 2.502; P > 0.05). Parity of the puerperium women (2.05 ± 1.28) was significantly higher than that of Pregnant (1.10 ± 1.16) and Non-pregnant (1.16 ± 1.31) women, (F = 33.849; P < 0.05). The pregnant women had significantly lower values of Platelet Count, 203.89 ± 65.2 × 109/L (range, 78-416) as compared to 257.0 ± 69.0 × 109/L, (range, 90-396 × 109/L,) of the non-pregnant subjects and the 249.1 ± 75.0 × 109/L, (range, 95-406 ×109/L) of the puerperium women (F = 28.437; P < 0.05). The mean Prothrombin time, 15.48 ± 2.49 seconds (range, 14-16 seconds) of the non-pregnant control women were significantly higher than the mean prothrombin time, 11.36 ± 3.12 seconds (range, 10-16 seconds) of the pregnant women and the 14.28 ± 4.22.49 seconds (range, 13-16 seconds) of the puerperium women (F = 57.843; P < 0.05). The international normalized ratio (INR) of the pregnant women (1.07 ± 0.1) as compared to the non-pregnant (1.11 ± 0.1) and puerperium women (1.09 ± 0.22) were not significantly different (F = 2.206; P > 0.05). The mean partial thromboplastin time with kaolin (PTTK) of the pregnant women, 44.1 ± 7.2 seconds (range, 43.3-46.1 seconds) were significantly higher than the mean partial thromboplastin time with kaolin (PTTK) of the non-pregnant women, 39.4 ± 8.1 seconds (range, 38.4-44.3 seconds) and the puerperium women, 40.32 ± 6.4 seconds (range, 41.3-43.3 seconds) (F = 20.512; P < 0.05). The mean Fibrinogen concentration, 4.4 ± 0.80 g/L (range, 2.9 -5.1 g/L) of the pregnant women were significantly higher than the mean fibrinogen concentration, 3.6 ± 0.88 g/L (range, 2.8-4.4 g/L) of the puerperium women and the 2.6 ± 0.72 g/L (range, 2.6-4.3 g/L) of non-pregnant control women, (F = 164.877; P < 0.05).
Table 1: Comparison of the demographic and haemostatic parameters of the pregnant, non-pregnant and the puerperium women. View Table 1
Analysis of variance (ANOVA) was also used to test the influence of Haemostatic parameters of gestational age (trimesters) of the Pregnant and Puerperium women. Table 2 denotes that gestational age (trimesters) had no significant influence on the haemostatic parameters of the pregnant women except the mean Prothrombin Time and partial thromboplastin time with kaolin (PTTK). The mean Platelets Count of the second trimester (219.8 ± 87.8 × 109/L) is significantly lower than the mean platelets count of the first (257.0 ± 69.0 × 109/L) and third (249.1 ± 75.0 × 109/L) trimesters of the pregnant women (F = 03.784; P > 0.05). The mean Prothrombin Time of the third trimester, 10.60 ± 2.20 (10.0 - 11.2 seconds) is significantly lower than the mean prothrombin time of the second, 11.4 ± 3.12 (10.0-12.0 seconds) and the first, 14.10 ± 0.99 (12.0-16.0 seconds) trimesters of the pregnant women (F = 16.760; P < 0.05). While, the mean partial thromboplastin time with partial thromboplastin time with kaolin (PTTK) of the first trimester of the pregnant women were also significantly higher than the mean partial thromboplastin time with PTTK of the second and third trimesters (F = 4.603; P < 0.05). Whereas, the mean Fibrinogen concentration of the first trimester of the pregnant women (3.4 ± 0.8 g/L) is also not significantly lower than the mean Fibrinogen concentration of the second (3.7 ± 0.72 g/L) and third (3.6 ± 0.88 g/L) trimesters (F = 1.850; P > 0.05). The difference in the mean international normalized ratio (INR) of the three trimesters were not statistically significant (F = 0.470; P > 0.05).
Table 2: Haemostatic parameters of the pregnant women based on gestational age. View Table 2
Figure 2 summarizes the prevalence of thrombocytopenia among the Pregnant, Puerperium Mothers and Non-Pregnant Women (Control). The pregnant women displayed higher frequency (26.5%) while the puerperium mothers had 7.5% and the Non-Pregnant Control Women had 12.00%. Thrombocytopenia is taken to be a platelet count < 100.0 X 109/L.
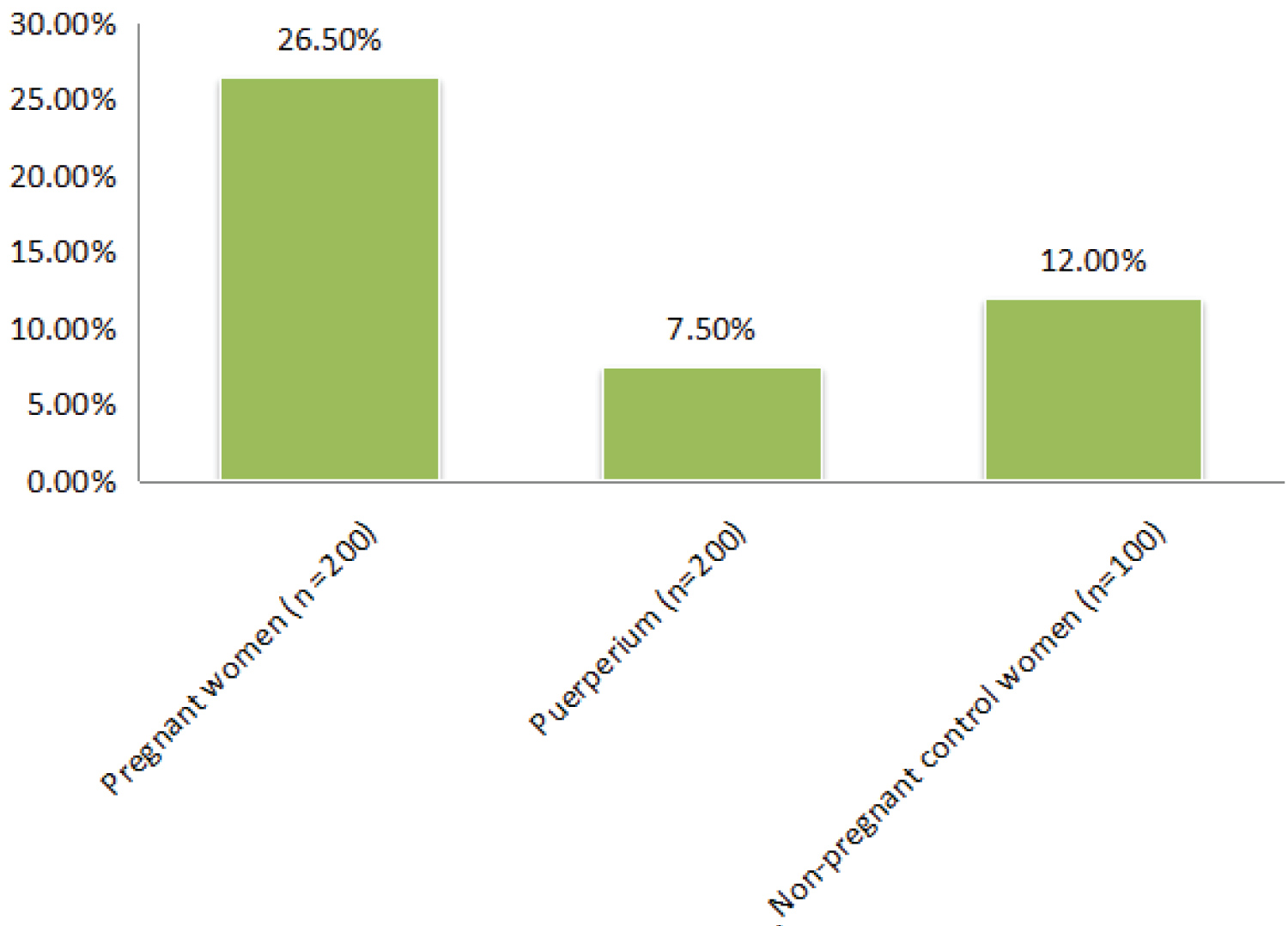 Figure 2: Prevalence of thrombocytopenia among the pregnant, puerperium mothers and non-pregnant control women.
View Figure 1
Figure 2: Prevalence of thrombocytopenia among the pregnant, puerperium mothers and non-pregnant control women.
View Figure 1
Figure 3 shows the prevalence of thrombocytopenia among the pregnant women according to gestational age (trimesters). The first trimester had 5 (16.7%), the second had 24 (20.0%) and the third trimester had 24 (48.0%) thrombocytopenia.
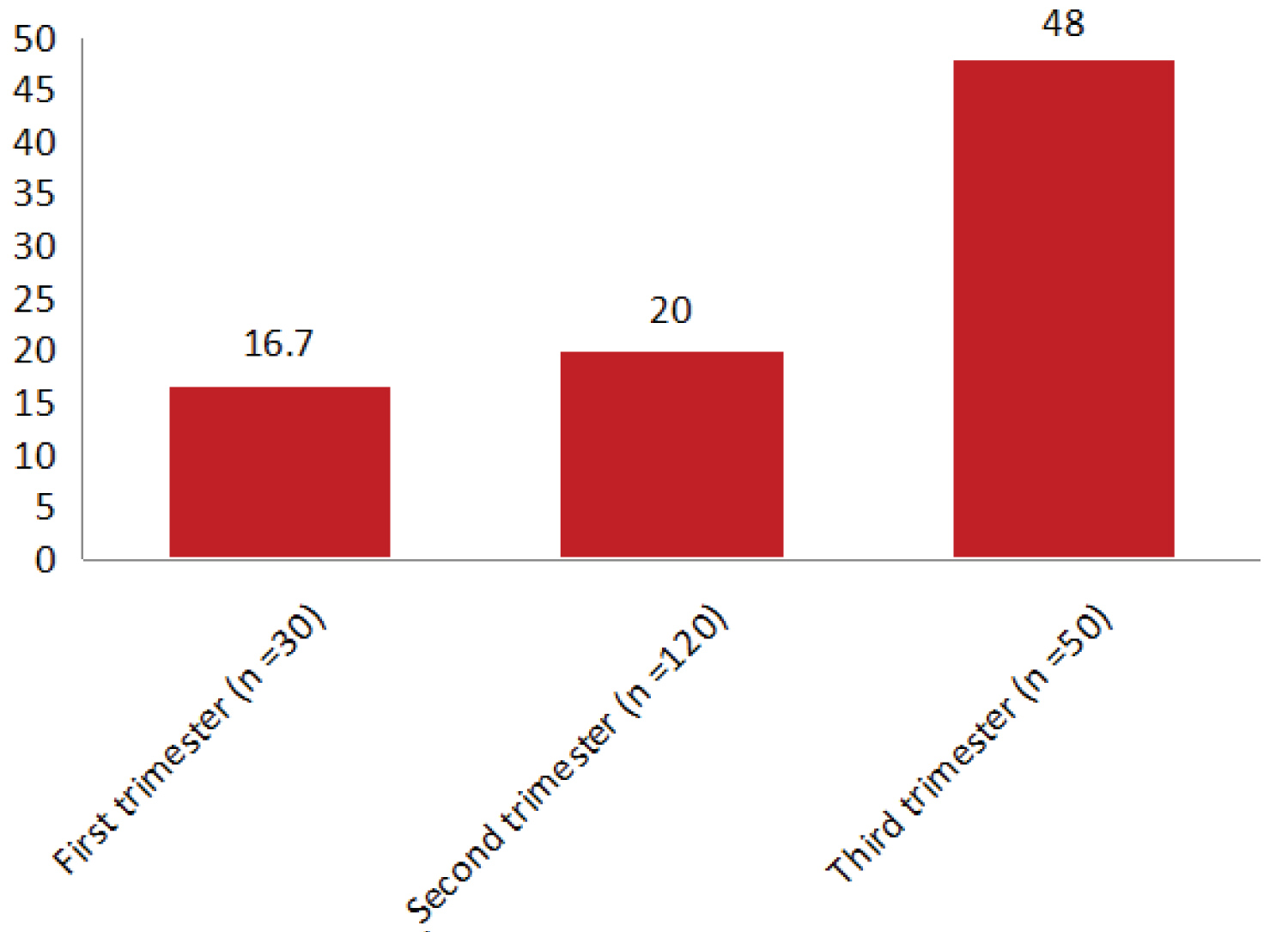 Figure 3: Shows the prevalence of thrombocytopenia among the pregnant women according to gestational age (trimesters). The first trimester had 5 (16.7%), the second had 24 (20.0%) and the third trimester had 24 (48.0%) thrombocytopenia.
View Figure 3
Figure 3: Shows the prevalence of thrombocytopenia among the pregnant women according to gestational age (trimesters). The first trimester had 5 (16.7%), the second had 24 (20.0%) and the third trimester had 24 (48.0%) thrombocytopenia.
View Figure 3
It has been established that normal pregnancy is associated with major changes in many aspects of haemostasis all contributing to maintain placental function during pregnancy and to prevent excessive bleeding in delivery. This phenomenon, however, also predisposes pregnant women to thromboembolism both during pregnancy and in puerperium. It is, thus, important to know the nature of those normal changes in the haemostatic test parameters in uncomplicated pregnancies in order to diagnose and manage common haemostatic problems of pregnancy.
This current study showed significant differences in the mean values of platelet counts among the pregnant women, those in puerperium and the age-matched non-pregnant control women. The mean platelets count of the pregnant women was lower than those in the puerperium and the age-matched non-pregnant control women (F = 28.437; < 0.05). There was also a progressive decrease in the values of platelets count during pregnancy. This is in line with some previous findings [11-13] but some other authors reported no significant difference [14,15]. The progressive decrease in platelet numbers can be attributed to haemodilution, increased consumption with reduced life span and increased aggregation by increased levels of thromboxane A2 at placental circulation [16,17]. Platelets passing over the often scarred and damaged trophoblast surface of the placenta suffer accelerated destruction or consumption. Increased consumption of platelets in the uteroplacental circulation has been suggested to be the main explanation of the reduction in the number of circulating platelets.
In contrast, studies by Bretelle, et al. [18] and Buseri, et al, [19] reported an increase in platelet count in pregnancy while Hellgren [20] reported that in normal pregnancy, platelet count is within normal range. The divergent views may be associated with differences in technique, improper sample collection, technical error, small sample size and more importantly racial difference. Variations in platelet counts during pregnancy have been associated with race and limited number of pregnant women used for the study [21,22]. Maternal age and parity had no effects on the platelet count during pregnancy in this study.
Platelet counts in the gestational period also showed variations in the three trimesters (Table 2). The mean platelets count of the second trimester (219.8 ± 87.8 × 109/L) was significantly lower than the mean platelets count of the first (257.0 ± 69.0 × 109/L) and third (249.1 ± 75.0 × 109/L) trimesters of the pregnant women (F = 3.784; P < 0.05), probably depicting the peak of haemodilution. However, the number of cases with significantly reduced platelet numbers is more apparent during the third trimester of pregnancy in this study (Figure 3). This implies that gestational age based on trimesters had significant influence on the mean platelets count of the pregnant women. This is in consonance with the findings of some previous authors [23-25]. According to Boehlen, et al. [26], platelet count decreases by an average of 10% during the third trimester as a result of haemodilution or accelerated destruction leading to younger and larger platelets production, which have increased number of platelet granules that enhance platelet function.
This study has shown that normal pregnancy is associated with changes in the haemostatic parameters studied, platelet count, prothrombin time (PT), partial thromboplastin time with kaolin (PTTK) and fibrinogen concentrations.
Significant differences in the mean values of platelets count were found among the pregnant women, those in puerperium and the age-matched non-pregnant control women (P < 0.05). The mean platelets count of the pregnant women was lower than those in the puerperium and the age-matched non-pregnant control women. There was also a progressive decrease in the values of platelets count during gestation with significant differences in the three trimesters (P < 0.05). The mean platelets count of the second trimester was significantly lower than the mean platelets count of the first and third trimesters of the pregnant women. Another specific finding in relation to platelets is the prevalence of thrombocytopenia (defined as platelet count less than 100.0 × 109/l) in this study, which was 26.5% among the pregnant women, 7.5% in puerperium women and 12.0% among the non-pregnant women. This suggests that thrombocytopenia is a relatively common phenomenon among women of child-bearing age in our environment.
This study found the mean prothrombin time of the pregnant women to be significantly shorter (P < 0.05) than the mean prothrombin time of the age matched non-pregnant control women. The international normalized ratio (INR) of the pregnant women as compared to the non-pregnant and puerperium women was not statistically significant, (P > 0.05) which suggest no likelihood of any significant bleeding possibilities in normal pregnancy.
This study has shown that Pregnancy influences haemostatic parameters, and has established that the haemostatic parameters of pregnant women differ from those of non-pregnant and puerperium females in our environment which necessitate having different normal reference values. This study has also come up with base-line values for platelet count, prothrombin time (PT), partial thromboplastin time with kaolin (PTTK) and fibrinogen concentrations among pregnant, non-pregnant and puerperium women for the very first time in our environment.