There are over 1 million Jehovah's Witnesses in the United States and nearly 8.5 million worldwide. Within the medical community, they are most notably known for their refusal of blood transfusions. Prior studies have shown that healthy euvolemic volunteers tolerate hemoglobin of 5 g/dL, although when faced with the stress of surgery their operative mortalities are over 30%. Herein we explore the use of Hemopure, HBOC-201, an investigational blood substitute, for a frail 72-year-old female Jehovah's Witness who acutely developed critical anemia due to an expanding hematoma which required operative intervention. The patient was weaned off vasopressor support by postoperative day one. She was transferred out of the intensive care unit on postoperative day nine, and by postoperative day 16, she had hemoglobin of 9 g/dL which she maintained until the time of her discharge. In our experience, Hemopure was well tolerated, and complimented supratherapeutic oxygenation for our elderly patient with life threatening critical anemia.
Hemopure, Critical anemia, Jehovah's witness, Blood substitute
ICU - Intensive Care Unit
There are over 1 million Jehovah's Witnesses in the United States and nearly 8.5 million worldwide [1]. Medically, these patients are well known for their refusal of blood transfusions, a practice established in 1945 based upon the literal interpretation of passages in Genesis and Leviticus in which those who eat blood are condemned [2,3]. Interpretation of this doctrine varies among members, although the official community continues to believe that membership and salvation are revoked for those who receive blood [4-8]. This becomes particularly difficult for healthcare providers in the setting of critical anemia and hypovolemic shock [9,10].
Transfusion protocols today are centered around a hemoglobin of 7 g/dL, although case reports involving Jehovah's Witnesses and select trials have provided insight into the outcomes of life-threatening anemia [11-14]. Carson, et al. described a 33% mortality for patients with a preoperative hemoglobin of less than 6 g/dL, and additional studies have shown a 44% mortality without transfusion for a hemoglobin less than 5 g/dL [13,14]. Within non-surgical patients, hemoglobin of 5 g/dL has been showed to be tolerated in healthy euvolemic individuals, although this threshold is not well understood in the critically ill, elderly, or patients with decreased cardiovascular reserve [15].
Herein we present a case report of a malnourished 72-year-old Jehovah's Witness who received HemoPure (HBOC-201, Hemoglobin Oxygen Therapeutics, Souderton, PA), an investigational blood substitute, after experiencing life threatening anemia while in the intensive care unit (ICU) [16].
A 72-year-old Jehovah's Witness with a history of stage three nasopharyngeal melanoma status post-resection with post-operative radiation in 2011 and follicular lymphoma status post-bendamustine in 2014 who presented with failure to thrive and concern for aspiration pneumonia. Since her head and neck radiation in 2011, she was only tolerating a liquid diet secondary to severe xerostoma and was recently experiencing worsening dysphagia. On admission, she was noted to have a 25% weight loss over the prior year, and depleted nutrition labs (albumin 2 g/dL, prealbumin 4 mg/dL), in addition aspiration pneumonia. Her oxygen requirements progressively increased on the floor, and she was transferred to the ICU in septic shock on hospital day seven.
Upon admission to the ICU, she had a right femoral central venous catheter placed which was ultimately removed a day later secondary to hematoma and pain around the site. When the central line was removed, the patient was noted to have a small 2 × 3 cm hematoma that remained stable over the following days. During her ICU stay, she continued to require 35-40 L high flow nasal cannula and experience symptomatic hypotension with diuresis. On ICU day 5, her hemoglobin was noted to be drifting and she was started on a proton pump inhibitor. The following day, her hemoglobin dropped from 7.3 g/dL to 5 g/dL with rapid expansion of her right groin hematoma overnight. Ultrasound demonstrated a femoral pseudoaneurysm with ateriovenous fistula between the superficial femoral artery and the common femoral vein. Before vascular surgery was able to definitively placed a covered stent across the artery, the patient's last recorded hemoglobin was 4.5 g/dL.
Given her life concerning anemia, she was enrolled in an investigational trial and given four units of HemoPure, HBOC-201, over the next 24 hours. The first two units were given at 250 cc/hr after she returned from the operating room. At that time, her blood pressure was also being supported with epinephrine and vasopressin. On postoperative day one, she continued to require vasopressors and her percent methemoglobinemia was noted to be 4.6%. She was given an additional two units of HemoPure at 250 cc/hr and her fraction of inspired oxygen was increased to 100% to increase the partial pressure of dissolved oxygen and improve distal oxygenation. All vasopressors were weaned off twelve hours later on postoperative day one and her fraction of inspired oxygen was therefore weaned back to 65%. Her percent methemoglobinemia peaked at 8.6% early on postoperative day two, after which point it steadily returned to normal on postoperative day seven.
In addition to HemoPure, her synthetic function was supported by folic acid (1 mg daily), cyanocobalamin (1,000 mg daily), thiamine (50 mg daily), erythropoietin (20,000 units daily), and iron (125 mg daily). Vitamin C (500 mg every 12 hours) was also administered to counter the oxidizing effects of HemoPure and to offset the methemoglobin created by maximizing her dissolved oxygen (goal 300-400 mmHg).
She was extubated on postoperative day 3 and by postoperative day 6 her hemoglobin had improved to 5.7 g/dL. She was able to be weaned to room air by postoperative day 9 and transferred out of the ICU that evening. On postoperative day 16, her hemoglobin reached 9 g/dL and remained between 9 and 10 g/dL until the time of her discharge.
Hemopure is a previously studied purified, polymerized, and cross-linked a cellular bovine hemoglobin that was introduced by Hemoglobin Oxygen Therapeutics in 1995 as an alternative to blood transfusions in the acutely ill, those without an available cross match, or those opposed to receiving blood transfusions [16]. Currently it is approved in South Africa, otherwise continues to carry investigational drug approvals throughout participating hospitals in the United States.
Hemopure has a higher affinity for oxygen than native hemoglobin (P50 of 40 mmHg vs. 27 mmHg), producing a slight right-shift effect, but otherwise carries the same 1.39 mL of oxygen per gram of hemoglobin. It comes in 250 cc units which have a shelf life of 2-3 years and does not need to be prepared prior to administration. Hemopure is run at 250-500 cc/hr through peripheral or central access and can have a mild hypertensive effect on patients during administration. No serious adverse events have been documented in the studies to date, aside from methemoglobinemia secondary to increased oxygen delivery and the lack of sufficient methemoglobin reductase - which is normally present in native red blood cells [16-21].
Hemopure is purple and causes errors in the reporting of laboratory values, many times being read as hemolyzed when they are not [22]. Furthermore, the functional carrying capacity of oxygen should be measured as total free hemoglobin. Every unit of Hemopure raises the total free hemoglobin by 0.63 g/dL, although in our experience quantitatively measuring the response was difficult. Clinically, we immediately saw an effect, as we were able to come down on our vasopressors entirely within 24 hours after her surgery. We administered a total of four units - two units at a time approximately 16 hours apart - which is in line with the expected half life of Hemopure (19-24 hours). Lastly, as reported by other groups we supported our patient through her immediate postoperative period with supratherapeutic supplemental oxygen and partial pressure of oxygen goals between 300 and 400 mmHg (Figure 1) [17-21]. Supratherapeutic oxygenation, in addition to Hemopure, likely contributed to the transient rise in methemoglobinemia experienced by this patient. We stopped administering Hemopure once our patient was stable off vasopressors with evidence of appropriate end-organ perfusion.
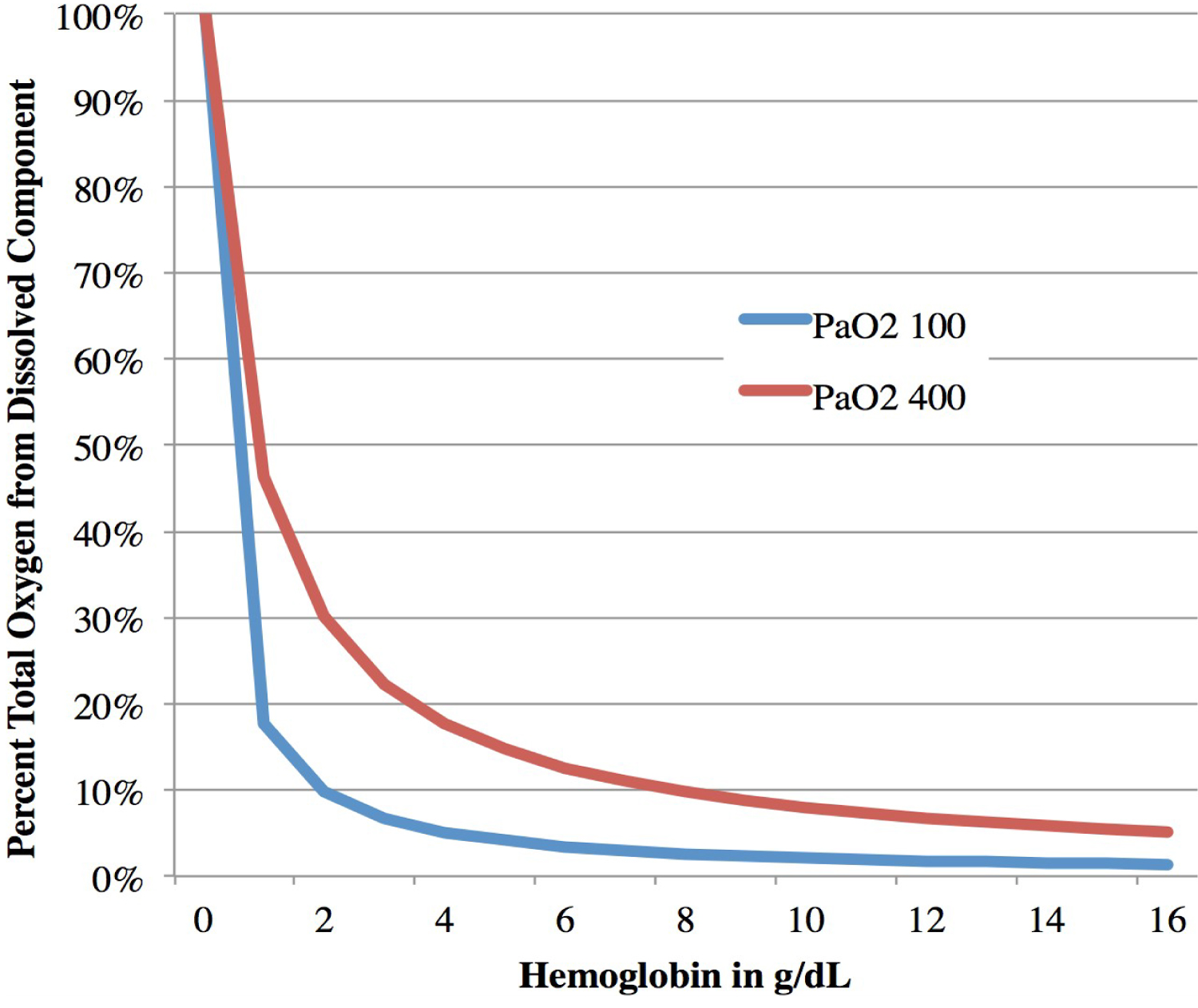 Figure 1: Percent contribution of dissolved oxygen relative to oxygen delivery at varying hemoglobin levels.
View Figure 1
Figure 1: Percent contribution of dissolved oxygen relative to oxygen delivery at varying hemoglobin levels.
View Figure 1
In our experience, Hemopure and temporary supratherapeutic oxygenation allowed us to successfully oxygenate an elderly patient during an episode of critical anemia. Side-effects of methemoglobinemia were observed, although temporary. The patient survived to discharge, supporting the use of alternative blood products in critical patients with religious objections to blood transfusions.
The relationship above is based upon the equation oxygen carrying capacity = (hemoglobin × saturation of oxygen × 1.34 mL oxygen/gram of hemoglobin) + (partial pressure oxygen × 0.003 mL oxygen/ 1 mmHg of oxygen tension). Percent total oxygen from dissolved component = (partial pressure oxygen × 0.003 mL oxygen/1 mmHg of oxygen tension)/oxygen carrying capacity based on a given partial pressure of oxygen and hemoglobin.