Background: A well-functioning blood transfusion service is essential for effective health-care delivery. Despite the fact that blood transfusions can save lives, the role of blood transfusion services is to assure the supply of safe blood from healthy donors. Although having a sufficient supply of blood is critical in blood transfusion, the caveat is that the collection and transfusion protocol must not put both the receiver and the donor in danger.
Identifying and attempting to retain repeat blood donors is critical. Understanding the most typical reasons for their deferral will enable us to prevent or remedy them as soon as possible, hence increasing their retention.
Objective: To determine the prevalence and causes of deferral among repeat blood donors in Dar es salaam, Tanzania.
Methodology: A cross-sectional study of 170 repeat blood donors at the Muhimbili National Hospital blood donation unit and the National Blood Transfusion Service (NBTS) form Dec 2021 to Jan 2022. Using a designed questionnaire donor's socio and demographic characteristics and assessment of donor's health and risk factors using NBTS questionnaire version 8.0. Donors were also tested for hemoglobin level using Copper sulphate method, ELISA test for HBV, HCV, and HIV, and Rapid Syphilis test using data provided in a developed questionnaire. Data were recorded and analyzed using Statistical Package for Social Science (SPSS) statistics software version 23 and p-values less than 0.05 were considered statistically significant.
Results: The men made up the majority of the 170 repeat blood donors, with an average age of 38 years. Seventeen percent of repeat blood donors were deferred. Temporary deferral was most commonly caused by low hemoglobin (41.4%), while permanent deferral was most commonly caused by the presence of TTIs (24.1 percent). Age above 45, female sex, and an inter-donation time of more than or equal to 5 months are all associated with deferral. Males were deferred in the majority due to TTIs (41%), whereas females were deferred in 75% due to low hemoglobin.
Conclusion: Deferral is common among repeat blood donors, and the leading cause is low hemoglobin and TTI. Deferral is associated with age over 45, female sex, and an inter-donation period of more than or equivalent to 5 months.
Repeat blood donors, Deferral, Muhimbili national hospital
Blood transfusion is a life-saving procedure that is used frequently in medical and surgical procedures. A reliable blood transfusion service is essential for effective health care delivery. Despite the fact that blood transfusions can save lives, the role of blood transfusion services is to assure the supply of safe blood from healthy donors [1]. While having an adequate supply of blood is critical in blood transfusion, the caveat is that the collection and transfusion protocol must not put the recipient or donor in danger [2]. This is accomplished by establishing donor deferral criteria and ensuring that prospective donors are thoroughly screened for transfusion-transmissible illnesses and other risk factors. Temporary or permanent deferrals are possible [3]. Temporary deferral means the prospective donor has been deferred due to a reversible, time-limited factor like low hemoglobin or high/low blood pressure, whereas permanent deferral means the prospective donor has been deferred due to non-removable, long-term factors like HIV, Hepatitis B or C, or syphilis infection (TTIs) [4-6]. All deferred donors should be treated with respect and care in a confidential manner, with a clear explanation of the rationale for the deferral and the opportunity to ask questions. Tanzania's National Blood Policy contains a basic guideline for prospective donor selection and deferral, albeit it is not explicit [2].
In Tanzania, there are two types of donors: Voluntary (non-remunerated) donors and family (replacement) donors. Voluntary donors are selfless people who donate blood for the sole purpose of saving lives without expecting anything in return. Blood donation drives in churches, universities, military camps, towns, and schools are generally used to mobilize these groups. Non-remunerated family (replacement) donors include people who donate for hospitalized family members, friends, or associates [2].
NBTS advocates voluntary non remunerated and repeat blood donation over family replacement donors; this is because VNRBD is likely to more be safer donors [7]. The NBTS report shows a decrease in the proportion of blood collected from VNRBDs from 58% in the previous year (2018/2019) to 41.2% in 2019-2020 [7].
This was a cross-sectional study conducted in Dar es Salaam, Tanzania, at Muhimbili National Hospital's blood bank and National Blood Transfusion Services. The study was conducted among repeat donors at MNH blood bank unit and NBTS in Dar es Salaam Tanzania attending between December 2021 to January 2022.
Donors were given pre-donation counseling when they arrived to raise their awareness of the donor selection criteria, the blood donation process, and the tests that will be run on their blood. Registration was done with individual's full name, date of birth, gender and contact details and a unique donor number was assigned. Donor's blood pressure, pulse rate, temperature and weight were recorded. Then hemoglobin level measurement by using Copper sulphate method and those who qualified on all the above criteria were interviewed by using the donor questionnaire, data collection tool and signed consent. Donated blood was tested for TTIs and donors were told to come for their results voluntarily in two weeks. Blood samples for donors were collected about 4 mls in a red top blood collection tube for TTIs screening. HBV was screened by Murex HBsAg version 3.0 Elisa Test and HCV by Murex HCV Ag/Ab combination Elisa Test. HIV was screened by Murex HIV Ag/Ab Elisa test and syphilis by Espline TP Syphilis Rapid test. Male donors are recommended to donate again after three months while female donate after four months. Donors deferred during any stage were given information about the reason for the deferral, how to maintain healthy lifestyles and referred accordingly. The data collection tool was divided into three sections: The first section contained social-demographic information on the donor including age, gender, domicile, marital status, education, frequency and interval of donation, and when was the most recent donation. The second section used the NBTS's Standardized Donor Questionnaire (version 8.0) to assess donor medical history and risk. The third section contained the TTI results of the donors.
The data was cleaned, recorded, and entered into the Statistical Package for Social Science (IBM SPSS version 23) for analysis. The percentage of deferred repeat blood donors was calculated among all repeat blood donors who took part in the study. Cross tabulation with Pearson Chi-square test for categorical data and multivariate analysis were used to determine the relationship between deferrals and age, sex, inter-donation period, domicile, marital status, education level, and number of donations. In bar chats, the frequency of permanent and temporary causes of donor deferrals was distributed. Statistical significance was assigned to results with a p-value of less than 0.05.
On November 22nd, 2021, the Research and Publication Committees of MUHAS granted ethical permission for this study, as did the Directorate of Research and Publication of MNH through the Executive Director of MNH on December 3rd, 2021.
Participants were informed about the study and granted permission to participate, with those who agreed signing the consent form. During and after the study, confidentiality was preserved by securely storing donor records and entering data using just the donor's questionnaire number. The data was only accessible to those who were directly participating in the study. The information gathered will only be used for research and subsequent publishing.
A total of 2025 blood donors were attended between December 2021 and January 2022, among those 85% (1740/2025) were family replacement donors. VNRBD were 285 of which 65% (188/285) were repeat blood donors and of those 170 repeat blood donors (50 donors from NBTS) provided consent to participate in the study. The mean age of the repeat blood donors was 38 years (21 to 61 years), with majority of blood donors 41.8% (71/170) being in the 35-45 years-old age group. Ninety percent (153/170) of the repeat blood donors were male. Donors living in Dar es salaam constituted 92% (157/170) and 68.8% (117/170) of all repeat blood donors were married. Forty-five percent (78/170) had college/university education and about 56% (95/170) had donated more than five times in their life time. Approximately half of the repeat blood donors had inter-donation time interval of above or equal to five months (Table 1).
Table 1: Socio-demographic and donation characteristics of the repeat blood donors. View Table 1
Among all 170 repeat donors 17.1% (29/170) were deferred. The commonest cause of deferral at 41.4% (12/29) was low hemoglobin. Temporary causes constituted the majority of causes at 75.8% (22/29) these included low hemoglobin, high blood pressure and prior medication at 41.4%, 27.9%, 6.9% respectively.
Permanent causes contributed to 24.1% (7/29) and these were due to TTIs. Overall prevalence of TTIs was 4.1% (7/170) among all repeat blood donors. HBV infection constituted 10.3% (3/29) as the cause of deferral, syphilis was the second leading cause 6.9% (2/29) followed by HIV which was 3.4% (1/29) and one donor had co-infection of HIV, HBV and syphilis. All who had TTIs were male. Prevalence of HBV, syphilis and HIV in this study were 1.8%, 1.2% and 0.5% respectively among repeat blood donors in this study. Seventy-five percent (9/12) of females deferred were due to low hemoglobin while 41% (7/7) of males deferred were due to TTIs. Repeat donors with more than and equal to five months' inter-donation time were deferred due to low hemoglobin by 52% (11/21) compared to those with inter-donation time of less than five months whose majority were deferred due to TTIs 62.5% (5/8) (Figure 1, Figure 2, Figure 3, Figure 4 and Figure 5).
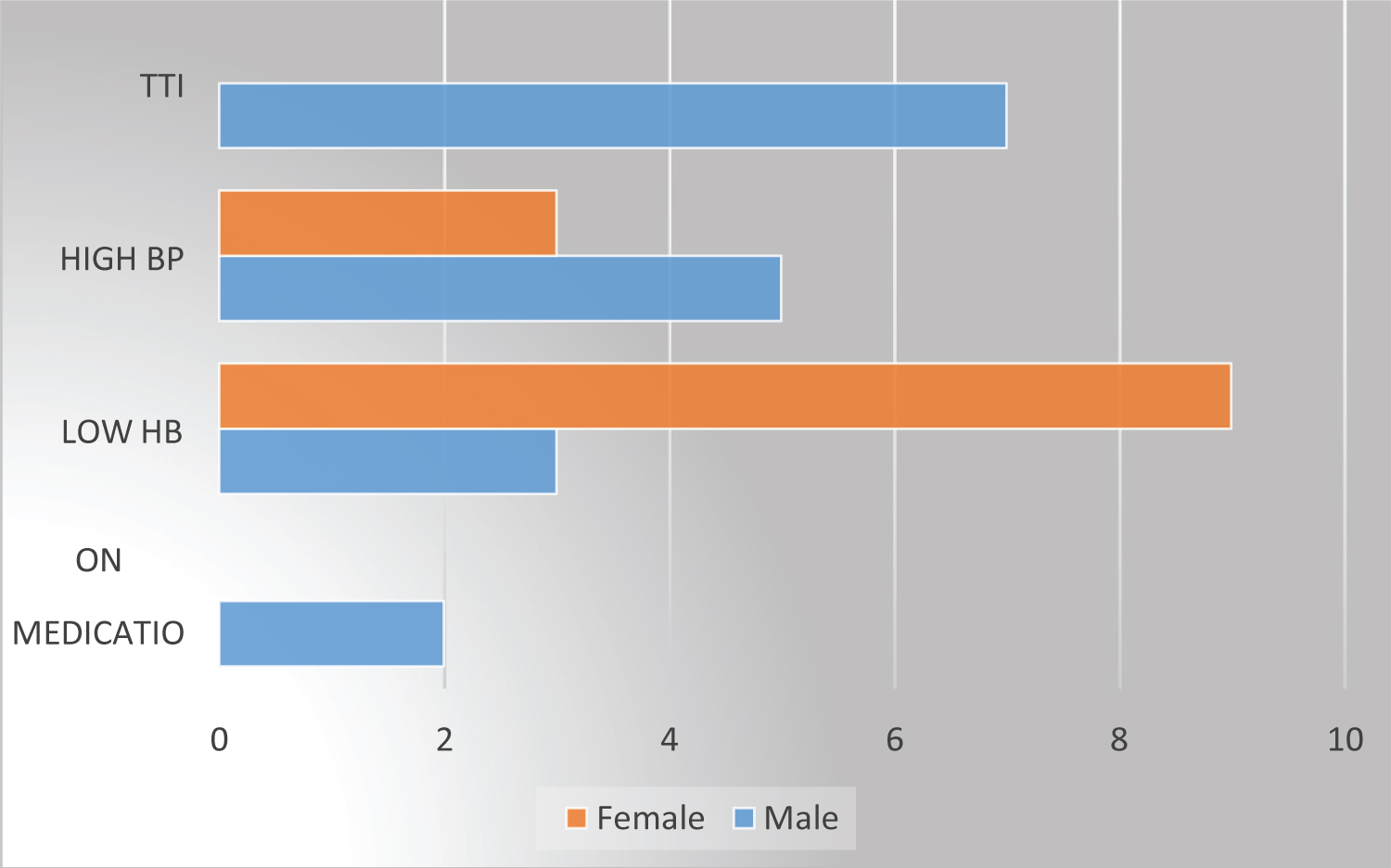 Figure 1: Causes for deferral by sex.
View Figure 1
Figure 1: Causes for deferral by sex.
View Figure 1
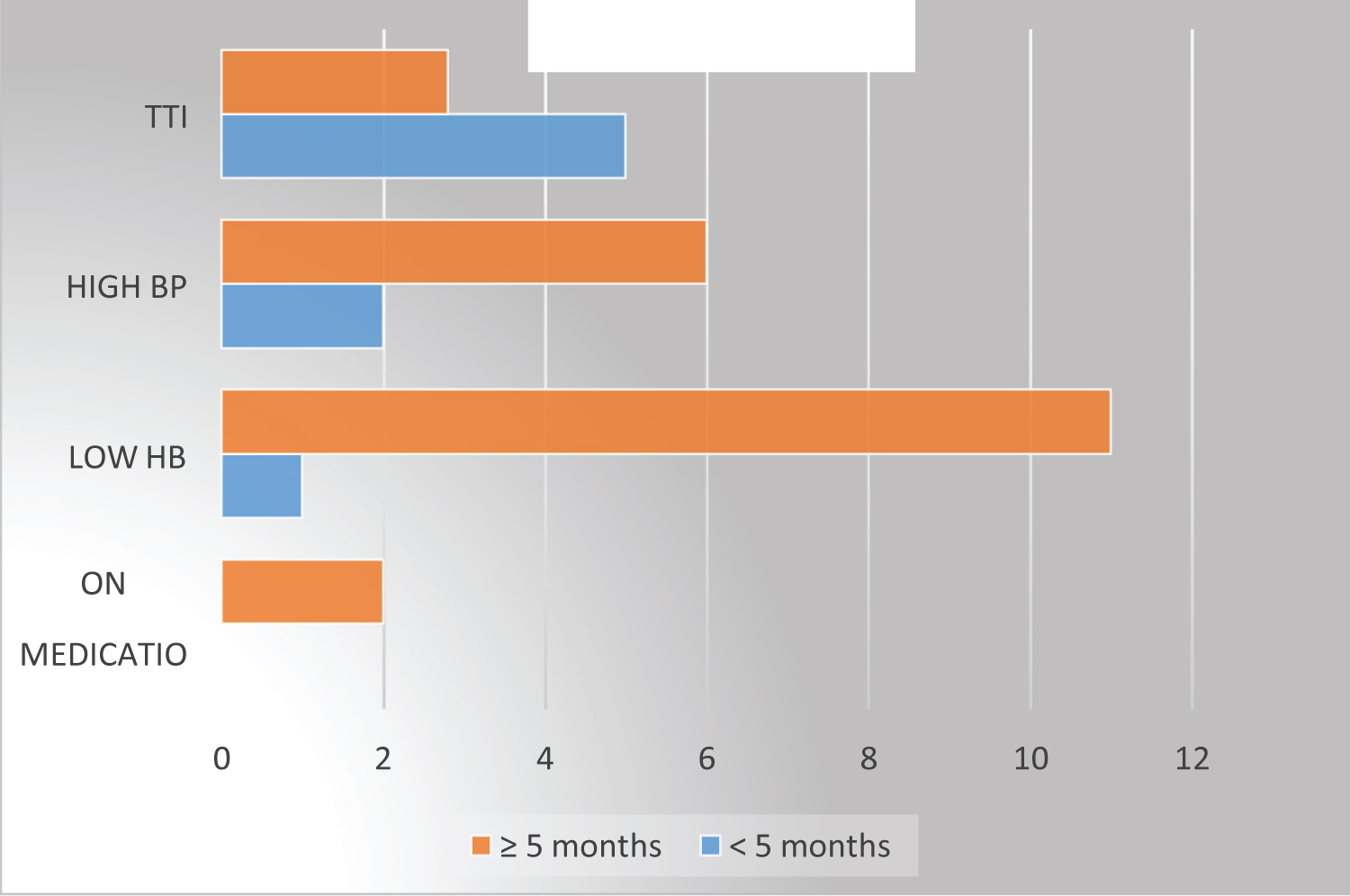 Figure 2: Causes for deferral by inter donation time.
View Figure 2
Figure 2: Causes for deferral by inter donation time.
View Figure 2
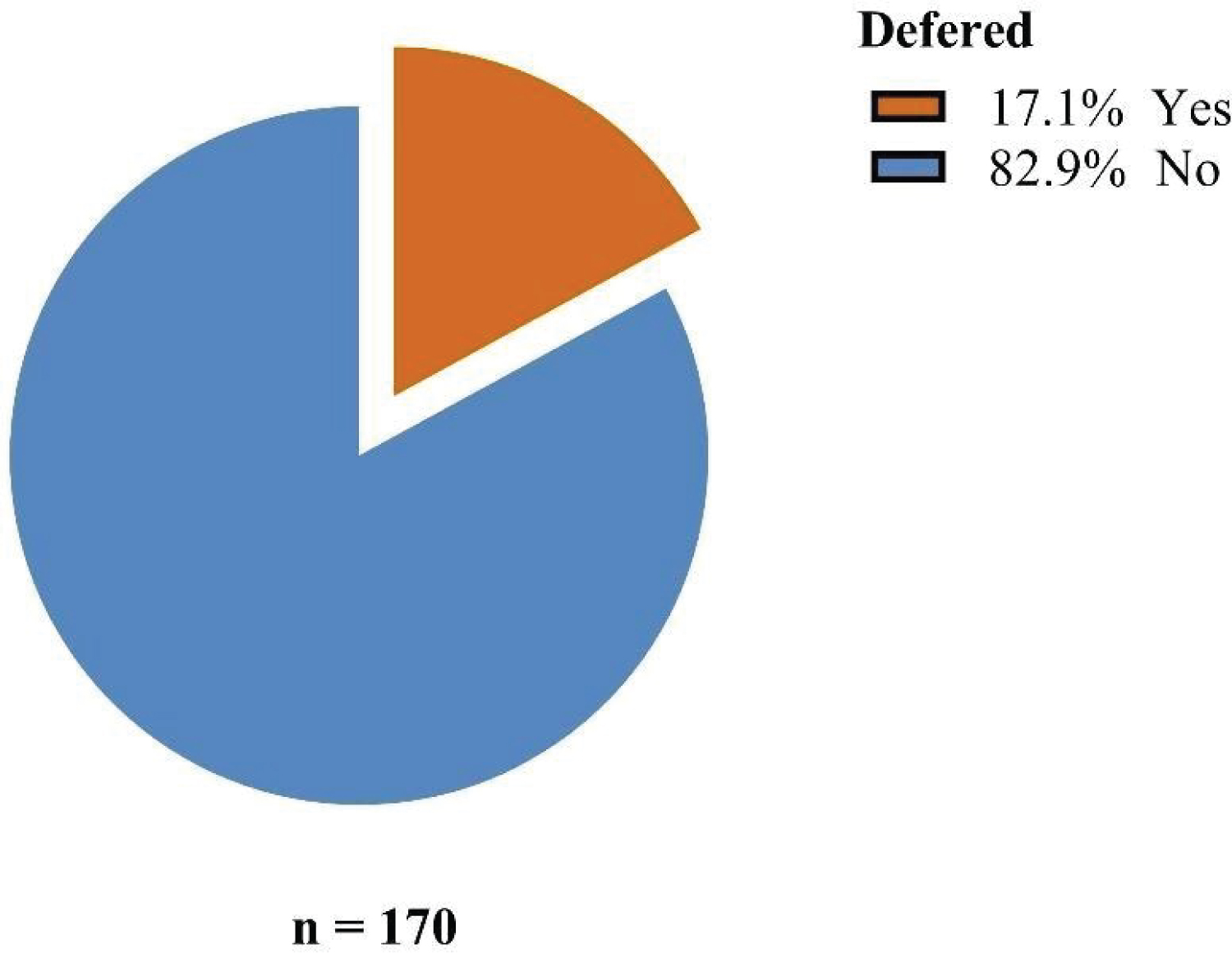 Figure 3: Prevalence of deferral in repeat blood donors.
View Figure 3
Figure 3: Prevalence of deferral in repeat blood donors.
View Figure 3
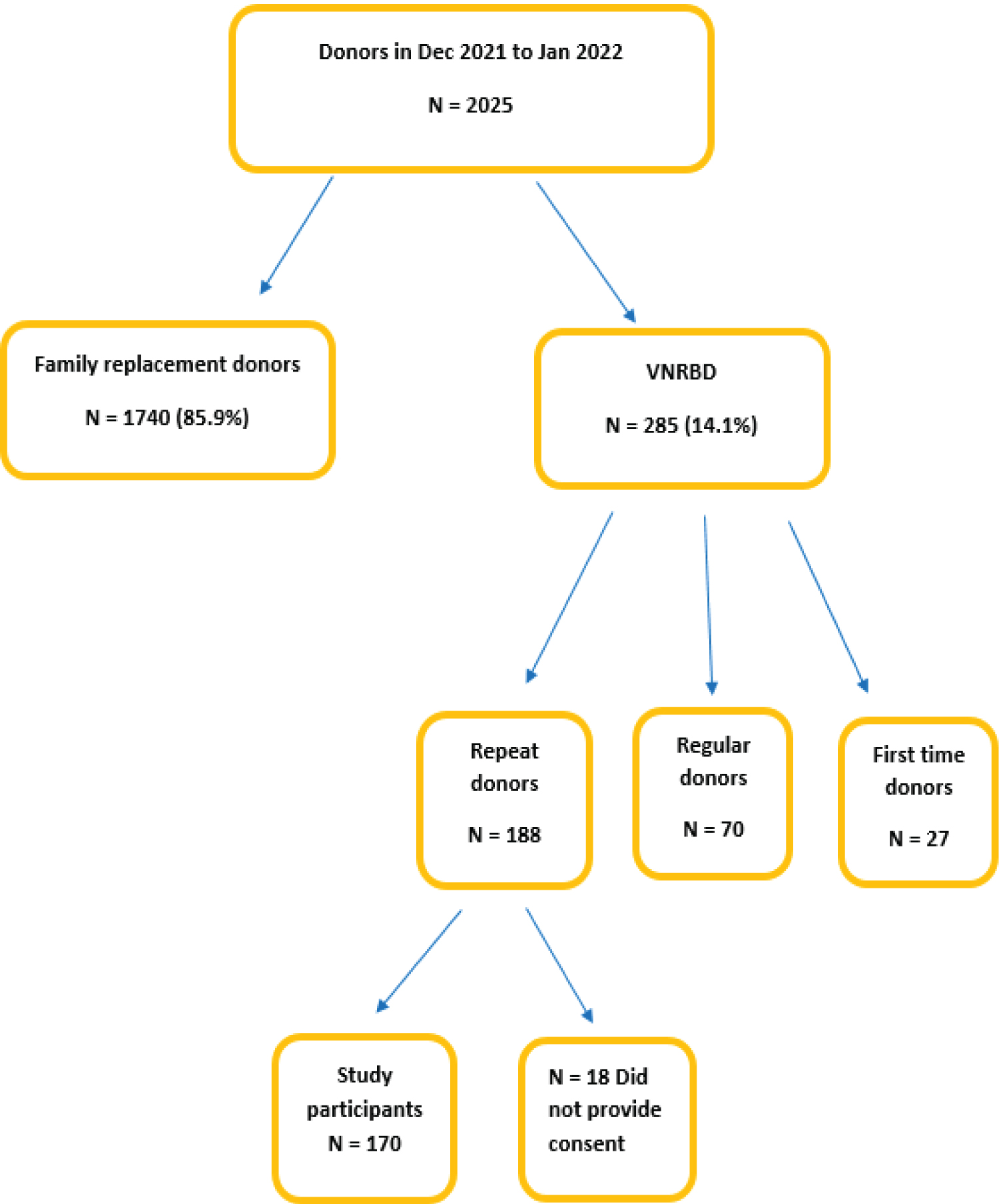 Figure 4: Flow chart of repeat donor recruitment.
View Figure 4
Figure 4: Flow chart of repeat donor recruitment.
View Figure 4
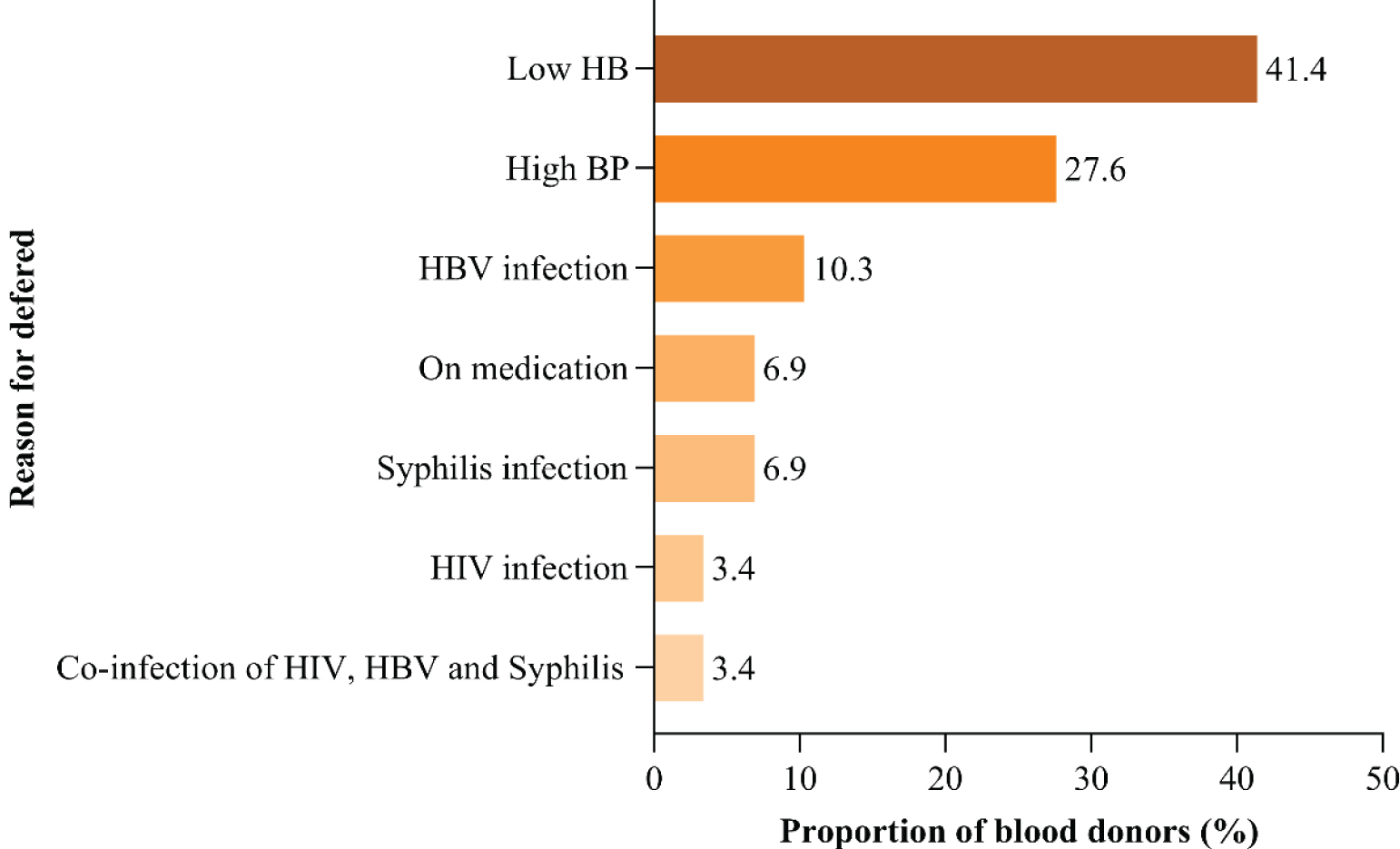 Figure 5: Reasons for deferral among repeat blood donors.
View Figure 5
Figure 5: Reasons for deferral among repeat blood donors.
View Figure 5
Age above 45 years, female sex, residence, marital status and inter-donation time of more than or equal to five months were found to be significantly associated with deferral (Table 2). Upon doing univariate analysis it was found that age above 45 years, female sex, marital status and inter-donation time of more or equal to five months were significantly associated with deferral.
Table 2: Factors associated with the deferral among repeat blood donors. View Table 2
These were further analyzed by multivariate analysis where age above 45 years, female sex and inter-donation time of more than or equal to five months had significant association with deferral. Those with age above 45 years were ten times more likely to be deferred compared to those less than 35 years. Female sex were eight times more likely to be deferred compared to male sex. Donors who donated more than or equal to five months ago were three times more likely to be deferred compared to those with less than five months (Table 3).
Table 3: Univariate and multivariate analysis of the factors associated with deferral. View Table 3
The goal of this study was to find out how common deferral is among repeat blood donors in Dar es Salaam and what causes it. The prevalence of deferral among repeat blood donors was found to be 17.1% in this study, and to the best of our knowledge, no other study on the prevalence of deferral among this type of donor has been conducted in Tanzania, therefore there is no study to compare. Eighteen percent of repeat blood donors were deferred in Japan [8] and repeat donors accounted for 77 percent of deferred donors in the Ivory Coast [9]. Saudi Arabia and Iran exhibited lower prevalence among all donors in India, with 5.6 percent, 4.3 percent, and 4.5 percent, respectively [10-14]. Studies on the prevalence of deferral among potential donors in Ethiopia, Nigeria, and the Ivory Coast [9,13,15-17] found 38.8%, 16 percent, and 10%, respectively, whereas a study in Tanzania [18,19] found 12.7 percent. These disparities in deferral rates are related to differences in donor selection standards, population awareness of donor eligibility criteria, and country socioeconomic situation.
Low hemoglobin was the most common reason for deferral in this study, accounting for 41.4 percent of all deferrals. Low hemoglobin was similarly found to be the major reason of deferral in a Tanzanian research [18]. Anemia was the major cause of temporary deferral in Nigeria, accounting for 21.9 percent and 39 percent [16], respectively, and 42.5 percent [15] in Ivory Coast. Anemia is the most common reason of deferral, according to studies in the Netherlands and India [20,21]. According to studies, the general population has a significant frequency of anemia, which limits the donor pool.
According to the socio-demographic characteristics of donors in this study, 90% of repeat blood donors are men. In studies in the Ivory Coast [9] and Nigeria [22], the majority of prospective donors were male (75.2 percent and 84 percent, respectively). A research in NBTS reports 86.7% of all blood donors were male [7] and in Northern Tanzania male donors accounted for 79.1% of all donors [18].
Female donors were found to be 39 percent [23] and 40 percent [24] lower in Nigeria and Ethiopia, respectively. Female donors account for barely 5% of all donors in Iran [25]. Women don't donate as often as men do because they don't feel as healthy as men do as a result of the monthly blood loss or because of pregnancy and lactation.
The majority of repeat blood donors in this study (41.8 percent) were between the ages of 35 and 44, which matches findings from studies on Kilimanjaro, where the majority of donors were between the ages of 18 and 44 [26] and 23.5 percent were between the ages of 31 and 45 [18]. This age gap is determined by the donor population chosen, for example, some studies were conducted among university students and did not include just repeat donors.
In this study, the overall prevalence of TTIs was 4.1 percent. Among all repeat blood donors, with Hepatitis B infection accounting for 10.3 percent of the cases, followed by syphilis and HIV. Previous research in Africa [9,19,27-29] have found a similar trend, while investigations in Tanzania's Dar es Salaam and Northern Zone found a lower prevalence [30,31]. The failure to notify repeat blood donors of positive TTIs results contributes to this, since research in Dar es salaam in 2017 [30] found that just 8.5 percent of infected blood donors were told of a positive result and in 2019 NBTS reported a blood donor notification of 15% [7].
Deferral was associated with age over 45 years by 29.7% (p 0.008) among research participants, which is similar to a study from Tanzania on blood donors at northern zone blood transfusion center where donors in the 44-61 years age range were deferred by 27% [18]. However, a research in Saudi Arabia found lower values of 11% among people over 45-years-old [32]. These findings can be explained by the fact that as people get older, they are more likely to develop comorbidities and other health issues that may prevent them from donating blood.
When compared to male donors, 52.9 percent of females were deferred (p0.004), and the majority of females were deferred due to low hemoglobin, which was the most common reason for deferral in this study. Studies from other parts of the world, such as Saudi Arabia [33,34], Nigeria [15,19] and Northern zone Tanzania [18], have also found high female deferral rates. High deferral rates in females can be explained by anemia, pregnancy, lactation, or childbirth, all of which are factors for donor exclusion.
TTIs were the most common reason of deferral in male participants in this study, accounting for 41% of all deferrals. Males were two times more likely than females to be TTIs positive, according to a study conducted in northern Tanzania [31,35-38]. Also, according to Cameron study [39], male donors had a significant high frequency of HBV infection. Males had higher seropositivity than females, which could indicate that methods of exposure other than sex are involved, such as sharing razors to shave hair. Females are more likely to seek medical help and have access to screenings, such as prenatal screening.
In this study, 75% of females were deferred due to insufficient hemoglobin levels. According to research in Tanzania, women of reproductive age have a high frequency of iron deficiency anemia [40], therefore it's possible that even female donors will have a high incidence of anemia. More research is needed in this area to determine the types of anemia often encountered among repeat blood donors.
Participants with an inter-donation period of more than or equal to five months were more likely to be deferred (p0.04) than those with less than five months, with low hemoglobin being the most common reason for deferral in those with fewer than months. A research from South Africa revealed no link between longer donation interval and low hemoglobin.
Donors who waited longer to donate were less likely to develop anemia, according to studies in Europe; however, this may differ between sexes, and in the United States, those who waited longer were less likely to be deferred. These findings are impacted by gender in this study, as the majority of those who waited longer were females, and majority of females deferred were due to low hemoglobin.
Deferral is very common among repeat blood donors. Low hemoglobin is the most common temporary reason for deferral, with transfusion transmissible infections being the most common permanent reason. Deferral is associated to age over 45, female sex, and an inter-donation period of more than or equivalent to 5 months. Males were largely deferred due to TTIs, whereas females were mostly deferred due to low hemoglobin.
1. Prevalence of anemia is still high in repeat donors, hence donors need to be counselled to do further studies to evaluate the cause of anemia.
2. Donors above 45 years needs regular health checkup before presenting themselves at donation center.
3. Health education on risks, transmission and prevention of transfusion transmissible infections especially in male donors and all donors in general as there is still high prevalence of TTIs in our setting.
4. Repeat blood donors who did not come for their results need to be notified of their serology results and referred accordingly.
5. Need of National database which is linked to all donation centers to keep records of TTIs in repeat blood donors and all donors so that this information may be useful when they present themselves for the next donation.
6. Strengthening of hemovigilance as a look back system to all blood donor's records.
1. This was cross-sectional study with a small sample size, there is need for a larger study which maybe both retrospective and prospective to assess information of repeat blood donors in the NBTS and other donation centers. This will provide analysis of multiple causes and associated factors of deferral.
2. Lack of full blood pictures and peripheral smear at least for those deferred donors who had low hemoglobin as baseline to investigate the cause of anemia.
The authors declare no conflict of interest.
Sincere appreciations to study participants, supervisors Dr. Clara Chamba and Neema Budodi and all the staff at MUHAS, Muhimbili National Hospital (MNH) department of hematology and blood transfusion, Central Pathology Laboratory (CPL) blood donation unit and National Blood and Transfusion Services (NBTS) for the valuable support during all stages of this study.