Carcinoma, Squamous cell, Penile neoplasms
Penile cancer is the most rarely observed cancer among male urogenital system tumors and is observed at an annual rate of 1/100000 [1]. Penile cancer risk increases significantly with increasing age, poor hygiene, and the presence of a foreskin. The most frequently observed type is the squamous cell carcinoma (SCC). Clinical examination of the inguinal lymph nodes is critical, as nodal involvement is a poor prognostic feature. Patients with T2 or higher-grade tumors and lymphovascular invasion are at high risk of nodal involvement and probably should have a lymph node dissection. Penile lesions are often infected and cause significant surrounding inflammation. Despite this, 50% of palpable nodes will be malignant. Complications are relatively common after an inguinal lymph node dissection (ILD) and proper meticulous surgical technique is important to decrease postoperative morbidity [2]. Penile SCC most commonly presents between the ages of 50 and 70 years. The majority of lesions are found on the glans (48%), followed by the prepuce (21%), both glans and prepuce (15%), coronal sulcus (6%), and shaft (< 2%). Clinical presentation is variable. It may present as a small area of induration and erythema or a large ulcerating and infiltrative lesion. As the disease progresses, there may be associated itching, bleeding, discharge, foul odor, and pain. Presentation may be delayed secondary to psychological factors, with an estimated 15 to 60% of patients postponing presentation for at least one year. Despite this, most men (66%) initially present with localized disease. Assessment of lymphatic spread with palpation of inguinal lymph nodes is an essential component of the initial physical exam. Lymphatic spread usually occurs in a predictable course, first to the superficial and deep inguinal nodes, followed by the pelvic, and then periaortic nodes. Distant metastases are generally uncommon (1-10%) and occur late in the disease [3].
Penile SCC can be divided into several subtypes. The most common subtypes include usual SCC (48-65%), basaloid carcinoma (4-10%), warty carcinoma (7-10%), verrucous carcinoma (3-8%), papillary carcinoma (5-15%), and mixed carcinomas (9-10%). Each subtype has distinct histologic features. Histopathologic analysis is used to grade the tumor, which is then assigned on a spectrum based on cellular differentiation (Table 1) [3,4]. Staging is performed using the TNM penile cancer system developed by the American Joint Committee on Cancer (Table 2) [5]. Staging is based on depth of tumor invasion, nodal involvement, and distant metastases (Table 3) [3,5].
Table 1: Histopathological grading of penile SCC. View Table 1
Table 2: American joint committee on cancer TMN classification for penile cancer. View Table 2
Table 3: American joint committee on cancer penile cancer staging. View Table 3
Our case is a 59-year old male, he's been smoking for 20 years, no multiple sexual partners and no viral infection (such as HPV, HIV). Patient was circumcised. Patient and his complaints started 3 months ago. First a bulging lesion occurred on the surface of penile glans. However, the lesion grew further. The patient did not apply to an advanced center as he has low socio-cultural level. He applied to our clinic when the lesion grew further, and he started having difficulty in micturition. The penile glans was fully covered, and invasion was detected in the urethral meatus (Figure 1 and Figure 2). Biopsy was taken from the patient and the urethral meatus was opened. The biopsy result was SCC. Clinical stage was T3cN1M0. CT scan and PET (Positron emission tomography) was performed on the patient for staging. Spread was detected on the inguinal lymph nodes (Figure 3). Radical surgery (total penectomy, bilateral pelvic lymph node dissection) was recommended to the patient. However, the patient did not accept. Since the tumor was deep localized to the skin, topical treatment was not recommended. Despite successful topical treatments in the literature, we have not recommended to the patient [6]. Chemotherapy was recommended, he accepted. Urethral meatus surgically opened, and he underwent palliative chemotherapy. Treatment of the patient continues.
 Figure 1: Appearance of penile cancer (invasion of urethral meatus). View Figure 1
Figure 1: Appearance of penile cancer (invasion of urethral meatus). View Figure 1
 Figure 2: Appearance of penile cancer (invasion of glans penis). View Figure 2
Figure 2: Appearance of penile cancer (invasion of glans penis). View Figure 2
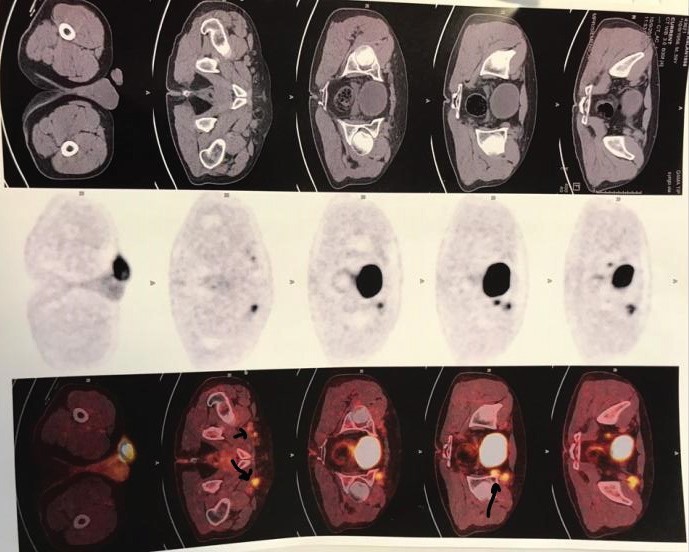 Figure 3: PET/CT scan (positive inguinal lymph nodes). View Figure 3
Figure 3: PET/CT scan (positive inguinal lymph nodes). View Figure 3
A logical and effective therapeutic approach to PC is possible despite the lack of randomized trials. For localized disease, there are sophisticated approaches beyond mere amputation, such as glans-sparing partial penectomy, brachytherapy and reconstructive surgery. For metastatic disease in LNs, a curative neoadjuvant multidisciplinary paradigm is feasible instead of a palliative approach. Nevertheless, despite excellent outcomes in localized disease, locoregional and metastatic disease portend poor outcomes. Important research questions remain, such as the role of chemoradiation, and opportunities for targeted therapy. Unfortunately, in view of the rarity of the disease and little interest among pharmaceutical companies, few clinical trials have been conducted. Prevention and early detection appear critical. In particular, neonatal circumcision, smoking cessation and HPV vaccination may substantially reduce the incidence of PC. Indeed, HPV vaccination is already approved in the USA for males aged 9-26 years for preventing genital warts and anal cancer. Global collaboration is urgently necessary to make advances [7].
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent for patient information and images to be published was provided.