Intestinal helminth infections are among the most common infections worldwide and tend to be higher in school children than in other members of the community. The present study was aimed at determining the prevalence and intensity of gastrointestinal helminth infections among children and youth in Kouoptamo.
A cross-sectional study was carried out in the months of May and June, 2017 on 403 children and youth 3-20 years in six schools. Quality and number of eggs defaecated were determined using the simple flotation and McMaster techniques respectively.
Four soil-transmitted helminth (STH) species were observed with an overall prevalence of 13.9%, amongst which were Ascaris lumbricoides (8.4%), Hookworms (4.7%), Trichuris trichiura (3.2%) and Strongyloides stercoralis (0.5%). Prevalence of infection was relatively higher in females (15.3%) than males (12.5%) (P > 0.05), and polyparasitism was shown by 2.5% bi-parasitism and 0.2% triple-parasitism. The highest number of eggs excreted was shown by Ascaris lumbricoides (1295.59 ± 2165.37 sent out eggs per gram of faeces - epg), and the lowest by Trichuris trichiura (538.46 ± 540.51 epg). Based on the classes of infection intensity, 97% of infections were light.
This study shows that based on prevalence, Kouoptamo can be classified as a low risk zone, though intervention programs and education of the general public on personal and environmental hygiene should be implemented for prevention and control of these helminthic infections as well as individualized treatment.
Intestinal helminths, Prevalence, Children and youth, Kouoptamo, Noun, Cameroon
EPG: Egg Per Gram of Faeces; STHs: Soil Transmitted Helminths; PNLSHI: National Programme for the Control of Schistosomiasis and Intestinal Helminthiasis; GBNSK: Government Bilingual Nursery School Kouoptamo; CBCNSK: Cameroon Baptist Convention Nursery School Kouoptamo; GBPSKC: Government Bilingual Primary School Kouoptamo Centre; EPK: Government Primary School Kouoptamo; GBHSK: Government Bilingual High School Kouoptamo; COLAMI: Collège Bilingue Polyvalent de l'Amitié de Kouoptamo
Intestinal helminth infections are one of the most common infections world-wide causing major public health problems in developing countries with children being the principal victims. Infection rates are highest in children living in Sub-Saharan Africa (SSA), followed by Asia, then Latin America and the Caribbean (LAC) [1]. This is aggravated by the hot and humid climate, poverty, malnutrition, high population density, and poor health. Several factors can influence infection with these worms like socio-economic, cultural, physiological and behavioral with illiteracy, poor hygiene and sanitation.
Multiple socio-economic, cultural, physiological and behavioral parameters with illiteracy, poor hygiene and sanitation and above all bad governance influence infection with these worms [2]. For reasons not well understood, compared with any other age group, preschool and school-aged children (including adolescents) tend to harbour the greatest number of intestinal worms and, as a result, experience stunting growth, diminished physical fitness as well as impaired memory and cognition [2]. Even mild to moderate-intensity helminth infections during childhood have been associated with under nutrition and reduced physical fitness [3]. Common infections are caused by soil-transmitted helminths (STH) including Ascaris lumbricoides, hookworms, Trichuris trichiura and Strongyloides stercoralis. An estimated 4.5 billion individuals are at risk of infection with STHs world-wide [4]. Epidemiological studies have shown that poor sanitary conditions such as open field defecation and fecal contamination of water bodies are important factors leading to infection with intestinal worms, while spread is due to lack of personal hygiene [5].
In Cameroon, STH are widely distributed all over the country which infect about more than 10 million people [6]. As a result, it is considered a major public health problem by the Ministry of Public Health ranking only second to malaria [7]. This motivated Cameroon to launch the National Programme for the Control of Schistosomiasis and Intestinal Helminthiasis (PNLSHI) in 2003 [8]. However, intestinal helminth infections still remain a major public health burden in many parts of the country. Therefore, the primary objective of this study was to survey the prevalence of intestinal helminth infections among school-aged children in Kouoptamo, Noun Division.
This study was carried out in the town of Kouoptamo in Kouoptamo Sub Division as seen on Figure 1. Kouoptamo Sub Division, one of the 360 Sub Divisions of Cameroon is found in Noun Division, in the West Region of Cameroon. Its geographical coordinates are 5°39' 0'' North and 10° 36' 0'' East. Kouoptamo is located at about 1201 m in altitude, and counts over 8,000 inhabitants. The indigenous people are the Bamouns, and a majority are Muslims. About 90% of the people depend on agriculture for living due to presence of fertile volcanic soils. Kouoptamo has two main seasons with 8 months of rainfall, and the average annual rainfall is 1987 mm, while the average annual temperature is 21.9 ℃. The climate here is tropical, while vegetation is transition between savanna and forest.
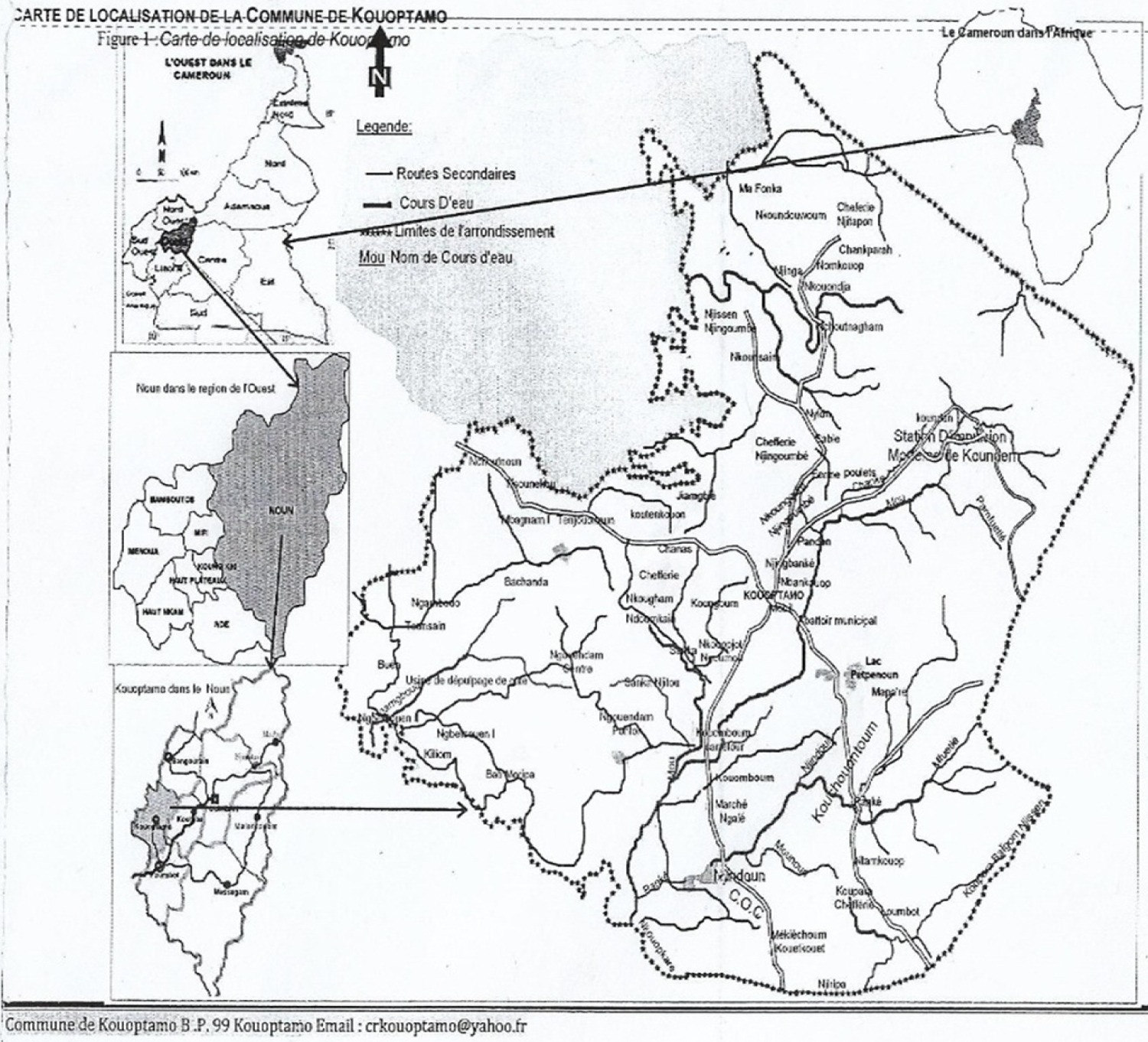 Figure 1: Map of the study area.
View Figure 1
Figure 1: Map of the study area.
View Figure 1
This was a cross-sectional study carried out in May and June, 2017. During the study, stool samples were collected, preserved and transported to the research unit of Biology and Applied Ecology in the University of Dschang for qualitative and quantitative analyses.
The study population consisted of 403 children and youth, 3-20 years, consisting of 203 girls and 200 boys from six schools; two nurseries (Government Bilingual Nursery School Kouoptamo (GBNSK) and Cameroon Baptist Convention Nursery School Kouoptamo (CBCNSK)), two primary schools (Government Bilingual Primary School Kouoptamo Centre (GBPSKC) and Ecole Publique de Kouoptamo (EPK)), and two secondary schools (Government Bilingual High School Kouoptamo (GBHSK) and Collège Bilingue Polyvalent de l'Amitié de Kouoptamo (COLAMI)).
The research proposal for this study was submitted to the Cameroon Bio-ethics Initiative (CAMBIN) for an ethical clearance under registration number 1127. Authorizations were obtained from Administrative, Public health, and School authorities. Participation in the study was justified by acceptance through informed consent forms from the parents or legal guardians, and oral acceptance were received from the children, after letting them know that participation is free and wilful.
Stool samples were collected from the participants in labelled plastic screw-cap vials with confidential information, and preserved by adding 10% Formalin, after which they were transported to the research unit of Biology and Applied Ecology in the University of Dschang for processing and examination.
The sample size was determined using the Lorentz's formula. Since the overall prevalence rate (P) of the helminthic infections was not known in the study area, the estimated prevalence P was taken as 50%. The calculation was done at 95% confidence interval (t) and a 5% margin of error (m) with n being the required sample size [n = t2. P(1-p)/m2] [9]. This gave a sample size of 384 and 5% of this value was added to it giving 403 in order to increase its sensitivity.
The 403 stool samples were analysed qualitatively using the Willis' simple flotation technique of saturated NaCl [10], while quantitative analysis was done using the McMaster counting technique in order to estimate the number of eggs per gram of faeces.
Approximately 2 g of faecal sample were put into a beaker containing 20 ml of floatation fluid and stirred thoroughly. The resulting faecal suspension was strained into another beaker and then poured into a labelled test tube arranged in a rack, ensuring that it was filled to the brim forming a convex meniscus, a cover slip was then carefully placed on it and allowed for about 15 min, then lifted and immediately placed on a glass slide, after which it was examined under a microscope with objectives 10X and 40X. Identification of eggs was aided by photos and dimension ranges prepared by the Bench Aid for the Diagnosis of Intestinal Parasites [11], and that of Thienpont, et al. [12].
The mean number of eggs/gram (epg) of stool obtained using the McMaster technique was used as the quantitative measure of infection status, based on the average egg count for each specimen. World Health Organization (WHO) criteria were used to classify each infected sample as being of light, moderate or heavy-intensity infection. For A. lumbricoides infection, light = 1 - 4999 epg, moderate = 5000 - 9999 epg, and heavy ≥ 10 000 epg. For hookworm infection, light = 1 - 1999 epg, moderate = 2000 - 3999 epg, and heavy ≥ 4000 epg. For Trichuris trichiura, 1 - 1999 epg represented light, 2000 - 3999 epg moderate and ≥ 4000 epg heavy worm burden [13].
The collected data was entered into Excel spread sheet and transported into SPSS version 20 for analysis. The prevalence of helminth infections were compared using the Chi-square test (χ2). The threshold for statistical significance was at p < 0.05, and 95% confidence interval (CI).
Four species of geo-helminths were observed after scrupulously examining the stool samples. The species together with their infection prevalence were A. lumbricoides 8.4%, T. trichiura 3.2%, hookworm 4.7%, and S. stercoralis 0.5% (Table 1).
Table 1: Stratified specific prevalence of helminth infections in Kouoptamo. View Table 1
The 403 children and youth, aged 3-20 years, were broken into 3 age groups (Table 2). The highest prevalence (18.8%) was recorded in children aged 3-8 years and the lowest (14.8%) in those 15-20 years. Ascaris lumbricoides, T. trichiura, and hookworm were present in all the age groups, while Strongyloides stercoralis was not confirmed in the age group 15-20 years. Ascaris lumbricoides showed the highest frequency in children of the age group 3-8 years, hookworm in the age group 9-14 years, Trichuris trichiura in the age group 3-8 years. Strongyloides stercoralis had equal frequencies in the age groups 3-8 years and 9-14 years (P > 0.05).
Table 2: Age stratified prevalence of helminth infections among children and youth in Kouoptamo. View Table 2
Of the 403 participants, 200 were boys and 203 girls, 56 of them were infected with at least one nematode species giving an overall prevalence of 13.9%. The females showed prevalence of infection with at least one nematode species slightly higher than the males that is 15.3% against 12.5%, respectively (P > 0.05). It was observed that among the 56 positive cases, 11 (2.7%) showed mixed infections amongst whom 10 (2.5%) had infections with two species and 1 (0.2%) infection with three species of intestinal nematodes. The highest prevalence of association was shown between A. lumbricoides + hookworm with 1.5%, and the lowest was A. lumbricoides + T. trichiura + hookworm with 0.2% (Table 3).
Table 3: Prevalence of mixed soil-transmitted helminth infections according to gender. View Table 3
The overall mean egg per gram (EPG) was 1295.59, 631.58, and 538.46, for A. lumbricoides, hookworm, and T. trichiura, respectively. It can be seen that A. lumbricoides showed the highest mean epg, while the lowest was shown by T. trichiura (Table 4). Based on the classes of the number of eggs excreted, 97.0% cases were light (Table 5).
Table 4: Mean epg of helminth infections among school aged children and youth in Kouoptamo. View Table 4
Table 5: Stratification of the major soil transmitted helminths according to classes of infection. View Table 5
The present study which having as objective to provide base line information on the status of gastrointestinal helminthes among the school children and youth of Kouoptamo in Kouoptamo Subdivision, the following information was obtained.
Based on overall prevalence (13.9%) observed, this community can be classified as a low risk zone according to the WHO disease specific thresholds [14]. This prevalence is lower than that of a previous study conducted by Tchouyabe [15] in Njimom a neighbouring Sub Division of the same Noun Division who found a 77.5% prevalence of helminth infection. It was also found to be lower than that observed by Ngangnang and Payne, [16] in Nkondjock (Cameroon), Baraket and Zewdneh, [17] in Southern Ethiopia, who found an overall helminth prevalence of 24.5% and 59.9% respectively. Contrarily, this prevalence was higher than that observed by Adou-Bryn, et al. [18] in Ivory Coast and Sammy, et al. [19] in the Ashanti region of Ghana who had prevalence of 10.4%, and 11.2% respectively. These variations in prevalence might be due to differences in altitude, climatic conditions, environmental sanitation, socio-economic and educational status of parents and study subjects, and previous control efforts.
The four parasitic nematode species A. lumbricoides, hookworm, T. trichiura and S. stercoralis identified during this study were similar to that observed in Guinea among school children [20] though with varying prevalence of, 35.7%, 18.9%, 12.2% and 10.1% for Hookworms, A. lumbricoides, T. trichiura, and S. stercoralis respectively. Ngangnang and Payne [16] had higher prevalence for A. lumbricoides (12.0%), and hookworm (9.4%), but agreed with the present study on the prevalence of T. trichiura (4.1%). Al-Meckhalafi, et al. [21] observed a prevalence of 8.5% for A. lumbricoides which strictly agrees with that of this study (8.4%) and a much lower rate of T. trichiura (0.5%) disagreeing with that of the present study. The high prevalence of Ascaris infection could be attributed to the fact that the eggs can survive prolonged periods under warm, shady and moist environmental condition which could be a reason for their long constant infection [22]. The lower prevalence observed for S. stercoralis could be due to the fact that the corprological technic used is not well adapted for diagnosing it. The specific differences in species prevalence would be due to different climatic conditions and risk factors which favoured and influence development and distribution of the eggs and larva of the helminths. A striking observation from this study is that all the helminth species observed are STHs and since the population of this area rely so much on farming, infection chances tended to be high.
Generally in this study, females showed an overall higher infection with at least one worm species than males, 15.3% against 12.3% respectively though not significant. This disagrees with studies carried out in Kenya [23], but agreed with the studies in Ethiopia [17]. The difference in infection between gender could be due to the very high involvement of females in farming activities carried out in this area exposing them to STHs. Multiple infections co-existed in the study subjects. Polyparasitism was shown precisely by bi-parasitism (2.5%) and triple-parasitism (0.2%). Alamneh and Endalkachew [24] in Ethiopia had similar observations, but Mengistu, et al. [25] had a contrasting view. The highest mixed infection was between Ascaris lumbricoides and hookworm, while the lowest was between Ascaris lumbricoides, T. trichiura and hookworm. Multiple infections may have far reaching effects on the health of such individuals as they may suffer from multiple morbidities [7], and this may also result in poor academic performance.
The mean parasitic loads were generally low. These observations corroborate earlier reports of Ngangnang and Payne [16]. This indicates that specific number of eggs excreted per child was low resulting to degrees of infection with 97% light infections. Only A. lumbricoides infection showed the highest mean epg. The overall light degrees of infection could be explained by the fact that all the head teachers reported that their schools were beneficiaries of the free donations of Mebendazole by PNLSHI in Cameroon. This occasional deworming could possibly be responsible for the low worm burdens. Re-infections could still occur as a result of the children not involved in such campaigns, or those not attending schools, who will tend to act as sources, introducing these parasites to the environment assisting in the spread.
This study reveals an overall comparatively low prevalence and light burden of infection indicating that the deworming campaign is proving effective. It was also observed that the prevalence of infection may not be influenced by age and gender. All the helminth species identified were linked to the soil therefore, there is need for an integrated control program while continuing the periodic deworming programs, enhancing the socio-economic status, supplying safe water for drinking and promoting health education in order to bring lasting impact on transmission of intestinal helminthic infections. Furthermore, the existing health education being delivered to the community through Health Extension Workers should be strengthened and its implementation should be regularly monitored by a health monitoring team.
Data and material are available to other researchers upon request.
The authors declared that they have no competing interest.
No funding.
We would like to thank the University of Dschang hosting Institution and more specifically to the research unit of Biology and Applied Ecology. We are also thankful to all the Head Teachers and Principals who gave authorizations, and parents who accepted the participation of their children. Finally much gratitude goes to the school children of Kouoptamo for providing stool samples and necessary information for this research work.
NNB, VKP, YC and NACN contributed to the design of the study, data collection, led the analysis and drafting of the manuscript. All authors read and approved the final manuscript.
The research proposal for this study was submitted to the Cameroon Bio-ethics Initiative (CAMBIN) for an ethical clearance under registration number 1127.
Not applicable.