Although both traditional and medical male circumcision are now being promoted as part of strategies for HIV prevention in Africa, particularly in countries with low circumcision prevalence, there are debates on the efficacy of male circumcision in the prevention of HIV at both individual and population levels.
In light of debates on the validity of male circumcision as the panacea for HIV prevention, the objective of this paper is to systematically review evidence on the association between male circumcision and acquisition of HIV infection in sub-Saharan Africa.
Thirty-six articles addressing the association between male circumcision and HIV transmission in sub-Saharan Africa were included in our assessment. Consistent evidence was found showing the protective effect of male circumcision on HIV infection for males at both individual and population level. In particular, evidence from three randomised control trials comparing the risk of HIV infection between circumcised and uncircumcised males in Sub-Sahara Africa suggest that male circumcision is significantly associated with risk reduction of HIV acquisition from female to male by approximately 50-60%. However, evidence of the protective effect of male circumcision for females shows mixed patterns and is inconclusive. Risky sexual behaviours post circumcision (ie., inconsistent condom use, having multiple sexual partnership); age at circumcision, surgical safety, type of circumcision (medical versus traditional), resuming sexual intercourse before the healing of the wound have been shown to modify the efficiency of male circumcision in protecting males against acquisition of HIV.
Although evidence from existing research supports promotion and scaled up of male circumcision in countries where the practice is not common, the concern that male circumcision might substitute other efforts such as condom use and behavioural modification interventions must be addressed alongside ethical concerns such as conflict with traditional values. A purely biomedical approach to the HIV/AIDS epidemic is unlikely to be sufficient in addressing the continued spread of HIV in sub-Saharan Africa.
Male circumcision, HIV infection, Systematic literature review, Sub-Saharan Africa, Medical circumcision
Male circumcision (MC) and female genital mutilation are believed to be the oldest surgical procedures introduced over 65 million years ago [1-4]. Worldwide, appropriately 30-38% of males are circumcised [5]. In the literature, male circumcision is understood to have been started as a religious rite among Jews and Muslims [2,6]. Other motives for circumcision included rites of passage, blood sacrifices, cultural markings, enhancement of masculine fearlessness and fecundity, preparation for marriage and adult sexuality, and the hardening of boys for warfare [2]. Today, circumcision is near universal in the North and West African countries, while it is not commonly practiced in Southern African countries. Male circumcision is being medicalised in countries of sub-Saharan Africa where circumcision is not commonly practiced and it has joined existing HIV interventions programs such as HIV testing, Antiretroviral drug (ARV), condom use and abstinence programs [7,8] following the successful randomised control trials [9-11] showing the efficacy of voluntary male circumcision in controlling the spread of HIV. For men who are not part of traditionally circumcising communities, voluntary medical MC presents an option as a HIV preventative measure. It is also presented, however, as a way to introduce more sterile practices to those men who would already be set to undergo circumcision. Debates around medical male circumcision and traditional initiation practices often situate these two practices as binaries [12]. Often, however, there is very little discussion about the ideological underpinnings of these two options. Campaigns promoting voluntary medical male circumcision seem to position it as a safe alternative to traditional circumcision without paying much attention to the socio-cultural nuances attached to the larger concept of the initiation process.
A scan on the literature on medical circumcision reveals ethical questions regarding the implementation of medical male circumcision, and rolling out this program without adequately addressing the ethical concerns could be counterproductive. Male circumcision has long been perceived to promote health, but traditionalist and cultural activities in Africa have not yet claimed that they practice circumcision in order to reduce HIV infection [13]. To them it is done to promote a cultural sense of manhood and sexual enhancement. In fact, communities practising traditional male circumcision were until recently discourage from practising circumcision and warned that their traditional practises fuel the spread of HIV [14]. The irony now in research is that circumcision is reported to have contributed to the reduction of HIV among ethnic groups that practice traditional male circumcision [13]. Evidence that societies that practice circumcision are less at risk of HIV epidemic is now being used as a basis to launch large scale male circumcision initiatives. The evidence should be disseminated with caution to avoid creating a false sense of security among traditionally circumcised men who may believe that they are not vulnerable to HIV infection.
While medical male circumcision is increasingly being incorporated in comprehensive strategies for the prevention of HIV [15], there are reports suggestive of an increased risk of HIV infection due to modified sexual behaviour post-circumcision [16] and non-sexual activities such as circumcision using unhygienic procedures [17]. Surgical safety of male circumcision is of great concern, particularly in traditional male circumcision [4]. It was reported in Kenya that knives that are traditionally used to remove the foreskin, are sometimes blunt and can tear apart the male organ, leaving scars which exposes them to HIV and other sexually transmitted diseases [18]. Others have highlighted that the fragile foreskin is susceptible to scratches and tears and it contains specialized cells (e.g., Langerhans) that join readily with HIV and other pathogens [19-21].
There is also a concern that male circumcision might substitute other efforts such as condom use and behavioural modification [7,8,16,22-25] and no researcher has ever advocated male circumcision as a natural condom [7]. Not only are the debates on male circumcision and HIV ongoing within the Western medical community, Africans themselves are in discussions about male circumcision and HIV/AIDS [8]. Political and traditional leaders generally endorse the idea that male circumcision is protective against HIV [26]. The low prevalence of HIV among circumcised societies has given the practice a stronger rationale or justification in a modern day society than even traditional and religious demands can provide. However, based on studies published to date, recommending routine circumcision as a prophylactic measure to prevent HIV infection maybe a counterproductive and short-lived intervention, because there are some evidence from trials [9,24] of serious adverse events from the procedure and of behavioural risk compensation among circumcised men. Looking at the corpus of scientific literature concerning the relation of male circumcision and HIV may be helpful in developing recommendations for HIV prevention. The objective of this paper is therefore, to systematically review scientific literature on the association between HIV and male circumcision in SSA countries. The study will also evaluate whether the impact of male circumcision on HIV acquisition in women, surgical safety or risky sexual behaviours could explain the contradictory evidence in the association between HIV and circumcision.
The Academic Search Complete, CINAHL Complete, MEDLINE, PsycINFO and PubMed databases were searched for papers published up to April 2018 that included 'circumcision' and 'HIV' as keywords or text in the abstract. Eight hundred and nine (n = 809) original research studies were identified in this way. A further search was carried out using keywords to search for all published studies of HIV risk factors in men in sub-Saharan Africa using the search condition '(HIV-infections (epidemiology, transmission)' OR 'HIV-sero-prevalence' OR 'HIV sero-positivity (epidemiology, transmission)' AND 'sub-Saharan Africa' AND ('risk factors' or 'risk'). A total of hundred and seven (n = 107) articles remained after screening in this way. Of these, abstracts of fifty-nine (n = 59) papers focused on health economics of voluntary male circumcision and were excluded, yielding forty-eight (n = 48) potential and eligible studies. Finally, we removed thirteen (n = 13) papers that used a proxy for circumcision, such as Muslim religion and those focussing on new-born and infants circumcision living the final sample of 36 for analysis.
The studies included in the review are shown in Table 1, grouped by author/year of publication, study design and key findings of the study. The eligible studies were published between 1989 and 2017. Twenty studies used quantitative research methods to evaluate the relative risk of male circumcision on HIV infection. These quantitative studies included ten cross-sectional studies using DHS data [3,17,19,24,27-30], case-control studies [22,23], two cohort studies [18,31]; and six randomised control trials [8,9,11,31-33]. Eight studies used a systematic review approach [4,5,7,33-35]. The systematic review papers covered a period from 1989 to 2017. Another eight studies were qualitative studies using focus groups and in-depth interviews. The focus groups were predominantly focusing on the acceptability and attitude towards male circumcision among males and females [9,25,28,36], while others focused on risk factors associated with male circumcision such as lack of condom use post circumcision [16,22,23-25,33,37]. Four qualitative studies included reported complications after circumcision such as excessive bleeding, infection, redundant foreskin and amputation of glands [9,11,38,39]. Geographically, all studies included in the review were conducted in SSA with the majority coming from Kenya (n = 7), South Africa (n = 4), Uganda (n = 3), and no more than two from Zimbabwe, Zambia, Lesotho, Nigeria and Cameroon.
Table 1: Studies addressing the association between male circumcision and HIV transmission in SSA countries. View Table 1
The global prevalence of male circumcision is approximately 38% [5]. The general population prevalence of male circumcision in SSA has been reported by three studies [5,16,26]. The population estimates show that male circumcision is practised in many parts of Africa and there is a spatial variation of the practice as shown in Table 2. Twenty-eight African countries are categorized as having a high (> 80%) male circumcision prevalence, nine countries have an intermediate (20-80%); and the other nine are categorized as having a low (< 20%) prevalence. There is also a general correlation between areas where there is low circumcision and those with high HIV prevalence (see Appendix: Figure 1). However, this ecological association may mean little without looking at individuals within populations, and taking into account other factors associated with circumcision status. There may be other factors associated with HIV risk that may be more prevalent among non-circumcising than circumcising populations [34,41].
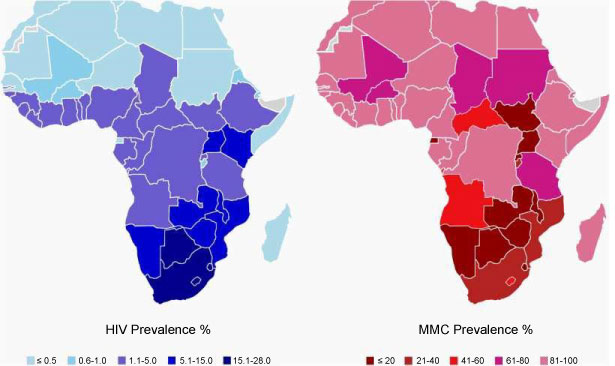 Figure 1: Map of HIV prevalence (left) and male circumcision prevalence in Africa. View Figure 1
Figure 1: Map of HIV prevalence (left) and male circumcision prevalence in Africa. View Figure 1
Table 2: Male circumcision prevalence in SSA countries. View Table 2
It has been pointed out that removal of a foreskin may reduce the risk of HIV transmission from women to men [47,48]. In a systematic review of 36 quantitative studies conducted in SSA countries among circumcised and uncircumcised males from 1989 to 2017, we found sufficient evidence from 26 studies showing the protective effect of male circumcision against HIV transmission. In the late 1980s, small-scale studies conducted in SSA countries suggested an association between having a foreskin and a greater risk of contracting HIV [3,43,46]. It was first reported by Bongaats, et al. [46] that in 5 countries where more than three-quarters of males were uncircumcised, the average HIV prevalence was 16.4% and that among the 20 countries where more than 90% of males were circumcised, the average sero-prevalence was 0.9%. Moses, et al. [3] examined the geographical patterns of male circumcision practices in Africa and HIV sero-prevalence and concluded that in locations where male circumcision was practised, HIV sero-prevalence was considerably lower than in areas where it was not practised. Conclusive evidence of the protective effect of male circumcision on HIV infection came from three randomised trial (RCTs) conducted in Uganda, Kenya and South Africa between 2000 and 2006. In total, 10,908 uncircumcised men were randomized to immediate circumcision (intervention group) or circumcision at the end of the trial (control group), and were followed up for up to 2 years [9-11]. The findings demonstrated that voluntary medical male circumcision reduced male HIV acquisition by 50-60%, a finding consistent with that of ten observational studies later [5,9,21,22,27,29,40,44,49]. Most recently, a systematic review of observational studies by Grund, et al. [7] confirmed these findings.
However, casting a doubt on the validity of the studies outlined above, eleven studies [8,16,18, 23,24,33,34,36,50,51] have noted that the RCT and observational studies might not have been adjusted effectively for confounding. These studies have argued that the impact of male circumcision on HIV acquisition in women, sexual behaviour after circumcision and surgical safety have not been controlled for, and therefore results are unreliable. However, the increase in HIV infections in Southern Africa where circumcision is less prevalent, has been faster than in all other parts of Africa, a suggestive of benefits accrued from male circumcision in reducing HIV cases, particular in the nations with near universal male circumcision rates in West Africa.
Seven studies reported on the impact of male circumcision on HIV acquisition in women [7,15,31,32,52] and they have all reported higher proportion of partners of circumcised men becoming HIV infected during the trials. Four randomised trials studies confirm similar results [15,31,49,52]. A RCT was conducted in Rakai, Uganda, to evaluate the impact of male circumcision on HIV acquisition in women [32]. In total, 922 HIV-infected men aged 15-49 years with high CD4 counts (≥ 350 cells/microlitres) were randomized to immediate or delayed circumcision and 163 uninfected female partners were enrolled and followed for up to 24 months. A higher proportion of partners of circumcised men became HIV infected during the trial with a hazard ratio of 1.58 (95%CI: 0.68, 3.66). Conversely, three studies reported that male circumcision, by reducing HIV prevalence in heterosexual men, will help reduce HIV prevalence and other sexual transmitted diseases that exacerbate HIV risk in women and children [31,53,54]. One recent study, after adjustment for the male partner's viral load, the risk of HIV transmission was lower in female partners of circumcised men than in partners of uncircumcised men [52]. One possible reason for the contrasting results between observational studies and the RCTs is that males in the observational study were likely to have been circumcised in childhood, which would have allowed for complete wound healing which have reduced their risk of exposure to HIV infection. Although it is possible that no direct impact of circumcision on male-to-female transmission exists, there will be an indirect benefit to women since HIV prevalence is likely to fall in male partners as circumcision services are expanded [29].
One of the major concerns about the male circumcision is the surgical safety and procedures of the skin removal which can exacerbate the risk of HIV infection through blood-sharing. Analysis of DHS data from Kenya, Lesotho and Tanzania revealed that circumcised male virgins were more likely to be HIV infected than uncircumcised virgins, suggesting that HIV transmission may occur through circumcision-related blood exposures [17]. Ten studies reported common surgical complications associated with male circumcision which included bleeding, infection, pain and swelling [9-11,34,38,41,55]. It has been revealed that complications are likely to be higher outside clinical settings, where the quality and quantity of training, supervision and resources vary [41]. However, in three randomised control trials, approximately 3-8% of surgeries were associated with an adverse event and most were mild [10,11,55]. While there are reports suggesting that complications are likely to be higher outside clinical settings, a systematic review of complications associated with male circumcision in sub-Saharan Africa revealed low prevalence of complications [34] for both medical and traditional circumcision.
Another major concern of being circumcised is that unsafe sex may occur if men believe they are completely protected from HIV infection following circumcision. Different patterns of sexual behaviour may be expected during the scale-up of male circumcision programs. Seven out of thirteen observational studies reported sexual behavioural changes involving multiple sexual partners, resuming sex early; and non-condom use after circumcision [7,8,10,22-25,55] and six studies reported no behavioural risk compensation after circumcision [9-11,18,33,37].
The timing of male circumcision is crucial. Medical practitioners point to the neonatal period as the ideal time [10]. Failure to circumcise early in infancy means loss of the benefit of protection against diseases and later circumcision at adult age is a more substantial, more expensive operation, and carries a higher risk of complications, and longer healing time [10,55]. If an adolescent or adult male normally engages in sexual activity, temporary sexual abstinence for 6 weeks is required, which some males and their sexual partners find challenging, putting themselves at risk of HIV transmission. Four studies revealed that circumcised men resume sexual intercourse before the wound is completely healed [55]. Another claim is that male circumcision diminishes sexual function, sensitivity and pleasure [56]. However, medical male circumcision does not adversely affect sexual function as shown by a detailed systematic review and meta-analysis of common forms of sexual dysfunction [5,57].
Conflict between the custodian of traditional culture and medical practitioner in relation to transforming traditional circumcision into medical circumcision may act as a barrier. Medical male circumcision may be perceived as a replacement for traditional male practice under the excuse of HIV prevention [14]. This could be worsened by the perception of some political figures, traditional and religious leaders that medical professionals are sceptical to traditional practices, authority and values [7]. Traditionalist argue that the medical circumcision model to HIV prevention has long condemned traditional circumcision and has been urging governments to ban the traditional practice because it is regarded as retrogressive and prevent the achievement of health goals. The perceived replacement of traditional authority and values could result in community resistance to the use of medical circumcision in HIV prevention. Community defensiveness can ethically be justified in the context of freedom of choice and right to practice what they believe in. In traditional sense, medicalisation of male circumcision tends to alienate people from their traditional practices. Program managers should emphasise that even though people have a right to their traditional practices, the risk of HIV infection should be reduced by practising safer sex. In the context of HIV, both traditional and medical circumcision does not protect 100% individuals against HIV infection. Medical research has demonstrated that male circumcision reduces risk of HIV transmission by up to 60%. However, we argue that the remaining 40% is still high risk. Medical male circumcision as a new HIV prevention strategy can be made more effective by the use of condoms in order to offer full protection against HIV.
Data from randomised control trials, meta-analyses, large observational studies in SSA countries and high quality systematic reviews were compiled and examined in order to determine the HIV risk reduction conferred by male circumcision. Overall, there is strong evidence of an association between male circumcision and risk reduction in HIV transmission from female to male. Although male circumcision is not as effective as other HIV interventions such as condom use and abstinence, its immediate and lifelong protection against HIV could be greater than these interventions. For instance, condoms are 80% protective against HIV infection, but they must be used consistently and correctly [7]. Unlike condoms, male circumcision is a one-off procedure that does not require future voluntary compliance each time a man has sexual intercourse. Nevertheless both male circumcision and condom use should be advocated. While critics of male circumcision argue against undue reliance on findings from randomised trials conducted in Kenya, Uganda and South Africa concerning male circumcision and HIV, current data and most recent country-specific figures (UNAIDS, 2016) show strong correlation between low male circumcision prevalence and higher HIV prevalence in other countries. Therefore, there is strong support for the conclusion conferred by the randomised control trials that male circumcision is protective against HIV infection at least in males. However, the timing of circumcision is crucial [30]. It has been shown that the cumulative lifeline benefits is greatest if male circumcision is performed early in infancy since early infant circumcision is simpler, more convenient and less risky than male circumcision performed later at adult age; and it confers immediate protection against urinary infections. Male circumcision also protects the female partners indirectly through reduced risk for male partners, as confirmed in randomised control trials [8,32].
Disputing the value of male circumcision's protection against HIV, some studies argue that less invasive HIV prevention strategies should instead be promoted, such as encouraging safe sex practices [24]. We argue that public health messages should include all effective measures for protection against HIV, and that male circumcision should therefore complement current safe sex messages. The effectiveness of each approach should, moreover, be considered in real-world settings. The benefits of medical procedures should always, of course, be weighed against the potential risks. Other studies question whether the potential benefits of male circumcision are worth the risk [12,58] pointing to potential risks of surgical accidents and supposed adverse psychological or sexual effects. The risk of major surgical mishaps with MC, however, seven out of ten studies reviewed indicated that the risk is extremely low and the benefits gained from male circumcision far outweigh the risks. Although some studies argue against downplaying the procedural pain that can occur during circumcision, the evidence cited by Morris, et al. [5] suggest that with the use of local anaesthesia, pain is negligible and three studies revealed that the procedure is well tolerated when performed by trained professionals under sterile conditions with appropriate pain management. Complications are infrequent, most are minor; and severe complications are rare.
Although health benefits are not great enough to recommend routine circumcision for all males, the benefits of circumcision are sufficient to justify access to this procedure for males choosing it. It is important that clinicians routinely inform individuals on the health benefits and risks of male circumcision in an unbiased and accurate manner. Individuals ultimately should decide whether circumcision is in their best interests. They will weigh medical information in the context of their own religious, ethical and cultural beliefs and practices. The medical benefits alone may not outweigh these and other considerations for individuals in specific societies. Various socio-political and cultural meanings attached to traditional circumcision practices and how biomedical approaches to circumcision are read through traditional understandings of circumcision as a ritual passage must also be taken into consideration. There is a greater need to understand how traditionally circumcised societies understand and introduce aspects of biomedicine into the process of traditional circumcision and how such pluralities could aid an understanding of the relationship between the cultural repertoires and HIV-interventions
The authors declare that they have no competing interests.