The number of very old patients with cardiac disease is increasing due to the longer life expectancy. There are few data on incidence and outcome of percutaneous cardiac procedures in patients ≥ 90-years-old (nonagenarians).
To retrospectively analyse the spectrum and outcome of percutaneous cardiac procedures in nonagenarians at our center.
The database at our center from 2005-2014 was searched for all percutaneous cardiac procedures, including coronary angiography with or without percutaneous coronary intervention (PCI), transcatheter aortic valve replacement (TAVR), percutaneous mitral valve repair by MitraClip (PMVR), balloon valvuloplasty of the aortic valve (ABVP) and radiofrequency ablation (RFA). Age at procedure, clinical data, type and findings at procedure, in-hospital outcome, survival and predictors for survival were analyzed.
Among 25,860 percutaneous cardiac procedures, 130 (0.5%) were performed in 93 nonagenarians including 48 women (mean age 91.7 ± 1.8 years at first procedure). Procedures included 85 coronary angiographies (45 including PCI), 25 TAVR, 11 ABVP, 6 PMVR (including one combined with TAVR), and 3 RFA. Overall survival after first procedure (n = 93) was 95% after 1 month, 78% after 1 year and 64% after 2 years. Left ventricular ejection fraction (LVEF) < 40%, history of heart failure, dyspnea NYHA III or IV, mitral valve insufficiency and history of atrial fibrillation were statistically significantly associated with worse estimated survival (p < 0.05, log-rank). These factors showed a strong collinearity in a multivariate survival analysis.
Percutaneous cardiac procedures in nonagenarians represent 0.5% of our procedures and have an acceptable survival rate considering the overall life expectancy in this age group. Further studies are required to delineate optimal patient selection in this age group for an acceptable ratio of procedural risk and benefit regarding survival and quality of life.
The number of very old patients with cardiac disease has been increasing over recent years due to population growth and longer life expectancy [1]. In Switzerland, the estimated life expectancy for patients being 90-years-old (nonagenarians) in 2015 was is 4.11 years for men and 4.75 years for women [2]. In 2015, there was an estimate of more than 70,000 nonagenarians living in Switzerland, of which 72% were females [3]. According to the Federal Department for Statistics in Switzerland, the population of people over 90 years of age will increase to 140,000 and 215,000 in 2025 and 2035 respectively [4]. The aging heart may be affected by coronary artery disease [5], valvular heart disease [6], diastolic dysfunction [7] and arrhythmias [8]. Therefore, management of these cardiovascular degenerative changes in the very old poses an increasing health problem and there are few data on optimal patient selection and on incidence and outcome of diagnostic and therapeutic cardiac procedures in the very old [9,10]. Many nonagenarians still enjoy a good quality of life, they and their relatives often demand an intervention to maintain this quality. Therefore, analysis of these data is important. Additionally, there are economic discussions how to quantify the benefit.
This study analyses the spectrum and outcome of percutaneous cardiac procedures in nonagenarians at our center including predictors of survival.
This retrospective study included all invasive diagnostic and/or therapeutic percutaneous cardiac procedures in patients 90 years of age or greater from January 2005 to December 2014 at our center. The procedures were coronary angiography with or without percutaneous coronary intervention (PCI), transcatheter aortic valve replacement (TAVR), percutaneous mitral valve repair by MitraClip (PMVR), balloon valvuloplasty of the aortic valve (ABVP) and radiofrequency ablation (RFA). Patients with pacemaker implantation or cardiac surgery were not included. We analysed the baseline characteristics and cardiac findings prior to the procedure, the in-hospital outcome and survival where available. These data were assessed retrospectively from internal charts and reports from the referring physicians and/or other hospitals. This study was approved by the local ethics committee (KEK-ZH-Nr. 2015-0379).
A procedure was considered elective or urgent by reported indication in the procedural report. BMI was considered low when < 20 kg/m2. Significant weight-loss was defined as reported weight-loss ≥ 10% of total body weight over the last 6 months. The living situation at the time of the procedure was assessed using the patients living address and/or medical reports, dividing into three groups: Own apartment, senior residency or nursing home. Pulmonary artery hypertension was defined as estimated or directly measured pulmonary mean artery pressure > 35 mmHg. Peri-procedural bleeding complications were considered significant if resulting in hemodynamic compromise, requiring blood transfusions or surgical intervention, or being located intracerebral (moderate or severe bleeding according to the Global Use of Strategies to Open Occluded Arteries definition, [11]).
All patients were referred either by their primary physician or their cardiologist to our center. Indication assessment and peri-procedural decision making were performed individually by our experienced interventional cardiologists and/or by the "Heart Team" where appropriate, always in consent with the patient and their families.
Follow-up data were assessed until May 2015, using the internal or external reported patient contacts in our clinic-database. For in-hospital outcome, the primary endpoint was all-cause-death. Secondary endpoints for in-hospital outcome where significant bleeding, stroke and other vascular complications. Regarding follow-up after hospital discharge, we chose all-cause-death as the only endpoint. A patient without reported patient contact after 1st of February 2015 was considered as lost to follow-up. As some patients had two or more percutaneous cardiac procedures, we chose to analyse the outcome of the procedure per procedure (descriptive statistics only) as well as per patient (descriptive and comparative statistics). Data for calculating the expected survival of an age and sex matched Swiss population was acquired by online-resources of the Swiss Federal Statistical Office [12].
Continuous variables were described using mean ± standard deviation (SD) or median and range. Categorical variables were presented as numbers and percentages. Estimated survival was assessed using the Kaplan-Meier method. Expected survival of an age and sex matched Swiss population was computed using the R package survival. Predictors for survival were compared using univariate (log-rank test) and multivariate (Cox-regression) survival analysis, considering a p value of < 0.05 as statistically significant.
There were 131 percutaneous cardiac procedures in 94 nonagenarians from 2005 to 2014 at our center, which represent 0.5% of a total of 25,860 percutaneous cardiac procedures conducted in the same time period. One patient withdrew consent leaving 130 procedures in 93 nonagenarians to be further analysed. From 2005 to 2009, 43 (0.37% of totally 11,747) percutaneous cardiac procedures were performed in nonagenarians with an increase to 87 (0.62% of totally 14,113) procedures from 2010 to 2014. Table 1 shows the summary of the conducted procedures per year from 2005 to 2014. There were 45 coronary angiographies performed with PCI and 40 coronary angiographies without PCI. Sixty-two coronary angiographies were elective, 23 were urgent. One patient had a TAVR and PMVR during the same procedural session, which was counted only once (as TAVR) for the total count, but included in both groups for respective survival analysis (hence the plus one in brackets for PMVR).
Table 1: Number and spectrum of percutaneous cardiac procedures in nonagenarians per year from 2005 to 2014 at our center. View Table 1
The indication for elective coronary angiography, TAVR, ABVP and PMVR was based on a reduction of quality of life by an underlying valvular pathology and/or suspicion of coronary artery disease. The indications for the three RFA in our study population was symptomatic atrial flutter, atrial fibrillation respectively atrioventricular node re-entry tachycardia. The indication for urgent cardiac procedures was acute coronary syndrome in coronary angiography and severe cardiac decompensation with severe aortic stenosis or severe mitral regurgitation in ABVP and PMVR. The indication was evaluated individually and in consent with the patient and their families.
Baseline characteristics, cardiac and laboratory findings were assessed per procedure (n = 130) and per patient (n = 93, at first procedure) and are shown in Table 2. Mean age at time of procedure was 91.9 years. Approximately half of all procedures (51%) were performed in male patients. No procedures were performed in patients living in a nursing home. Thirty-three patients had two procedures at the age of ≥ 90 years. There were two patients who underwent 3 procedures: One patient had diagnostic coronary angiography and two consecutive ABVP, the other one had diagnostic coronary angiography with two consecutive sessions of PCI. Baseline characteristics at first procedure showed very similar results between genders, except a higher frequency of arterial hypertension and higher mean left ventricular ejection fraction in women.
Table 2: Clinical characteristics, cardiac and laboratory findings per procedure (n = 130) and per patient (n = 93). View Table 2
Median length of hospitalisation was 2.5 days, with a range of one to 50 days. The patient with 50 days of hospitalisation underwent combined TAVR and PVMR and had a prolonged recovery time without stroke or another vascular complication, but with prolonged mobilisation. There was one single procedure related death during TAVR, where the device repeatedly embolized into the left ventricle with decision against surgical intervention. Overall, in-hospital mortality was 5% and was mostly caused by progression of pre-procedural cardiac decompensation despite successful procedure and/or non-procedure related complications such as pneumonia. Only one case of gastrointestinal bleeding after AVBP contributed to in-hospital death. There were two cases of coronary artery perforation, of which one required pericardiocentesis. Femoral bleeding requiring surgical intervention occurred in one case of coronary angiography and PMVR. The other two bleeding complications requiring blood transfusion included the gastrointestinal bleeding mentioned above and one case of unspecific peri-procedural blood loss during TAVR. All peri-procedural characteristics are listed in Table 3.
Table 3: Peri-procedural characteristics, all procedures (n = 130). View Table 3
We performed further comparison regarding the estimated survival of our 93 patients after their first percutaneous cardiac procedure at age ≥ 90 years. Survival rates after first procedure in general and after first specific procedure are shown in Table 4. Survival after the first procedure was 95% after 1 month, 78% after 1 year and 64% after 2 years. Mean survival of an age and gender matched Swiss population was 80% at 1 year and 62% at 2 years. The Kaplan-Meier curve of the survival after first procedure as well as the mean survival of an age and gender matched Swiss population are shown in Figure 1.
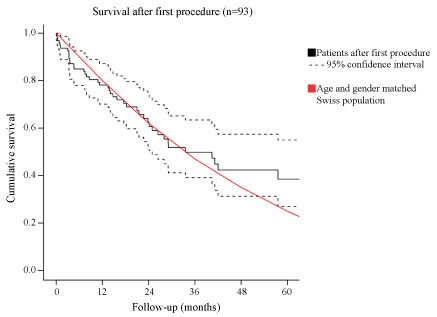 Figure 1: Estimated survival after first procedure (n = 93) with 95% confidence interval and mean survival of an age and gender matched Swiss population.
Figure 1: Estimated survival after first procedure (n = 93) with 95% confidence interval and mean survival of an age and gender matched Swiss population.
n = number of patients.
View Figure 1
Table 4: Estimated survival after first procedure (n = 93). View Table 4
Survival after first coronary angiography (74 patients) was practically identical to the overall survival, being the biggest subgroup. There was no statistically significant difference in survival after first coronary angiography with PCI (n = 36) or without PCI (n = 38, p = 0.19, log-rank). There was also no statistically significant difference in survival after urgent vs. elective coronary angiographies in general (p = 0.6, log-rank) or within the subgroup with PCI (n = 36, p = 0.5, log-rank), which is shown in the supplemental Table S1.
Table S1: Estimated survival after first coronary angiography (n = 74) and after first coronary angiography with PCI (n = 41). View Table 1
The Kaplan-Meier curves of the estimated survival after first coronary angiography and TAVR as well as the mean survival of an age and gender matched Swiss population are shown in supplemental Figure S1 and Figure S2.
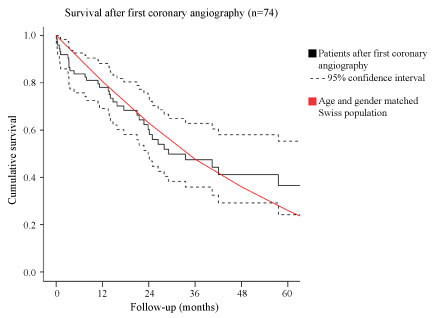 Figure S1: Estimated survival after first coronary angiography (n = 74) with 95% confidence interval and mean survival of an age and gender matched Swiss population.
Figure S1: Estimated survival after first coronary angiography (n = 74) with 95% confidence interval and mean survival of an age and gender matched Swiss population.
n = Number of patients.
View Supplemental Figure 1
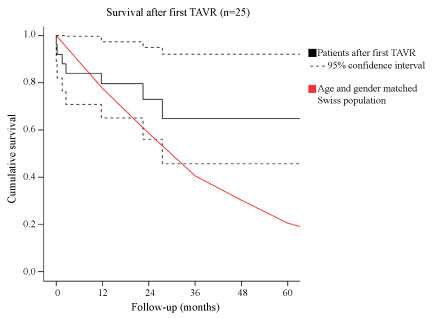 Figure S2: Estimated survival after first TAVR (n = 25) with 95% confidence interval and mean survival of an age and gender matched Swiss population.
Figure S2: Estimated survival after first TAVR (n = 25) with 95% confidence interval and mean survival of an age and gender matched Swiss population.
n= Number of patients; TAVR: Transcatheter aortic valve replacement.
View Supplemental Figure 2
In a univariate survival analysis, the following factors were associated with a lower survival rate after first procedure (n = 93, 46 deaths): history of heart failure (p = 0.02, log-rank), NYHA functional class III or IV (p = 0.045, log-rank), NYHA functional class IV (p = 0.016, log-rank), LVEF < 40% (p = 0.01, log-rank), mild to severe mitral valve insufficiency (p = 0.38, log-rank) and history of atrial fibrillation (p = 0.038, log-rank). None of these six factors remained statistical significant when adjusted for each other in a multivariate survival analysis. This underlines collinearity between these factors.
Regarding survival after first coronary angiography (n = 74, 39 deaths), univariate survival analysis showed similar factors as associated with a lower survival rate: History of heart failure (p = 0.006, log-rank), NYHA functional class IV (p = 0.006, log-rank), peripheral edema (p = 0.023, log-rank), LVEF < 50% (p = 0.01, log-rank), LVEF < 40% (p < 0.001, log-rank) and history of atrial fibrillation (p = 0.016, log-rank). None of these six factors remained statistical significant when adjusted for each other in a multivariate survival analysis. This again underlines collinearity between these factors.
No specific factor was significantly predictive of survival after TAVR. We did not perform any further survival analysis in the remaining treatment groups ABVP, PMVR and RFA due to their small patient numbers.
Our results show that percutaneous cardiac procedures in nonagenarians are rare, however increasing representing 0.5% in our procedures. Most common procedures are coronary angiographies, PCI and TAVR. Two-year survival in our cohort was 64% and was negatively impacted by a decreased left ventricular ejection fraction, heart failure, mitral valve insufficiency and history of atrial fibrillation.
Our study showed an increasing number of percutaneous cardiac procedures performed in nonagenarians over time at our center. Most commonly performed procedures in this age group include coronary angiography and TAVR. There are only few studies about cardiac procedures in nonagenarians. Most of them analyse the outcome after PCI [13-21]. The number of nonagenarians undergoing TAVR was also comparable to previous studies [22,23]. The number of patients receiving ABVP, PMVR or RFA was small in our study.
All patients seemed to have a good quality of life before they were limited by progressive heart disease. The frequency and severity of frailty in our study population remains unclear since our retrospective analysis lacks data for an adequate evaluation. However, the fact that there were no patients living in nursing homes excluded severe frailty in our study population. We interprete these findings as result of patient selection. Except arterial hypertension, cardiovascular risk factors were rare in our study population. This may be due to natural selection.
The length of hospitalisation regarding procedures for valvular heart diseases in our study population where considerably longer than usually observed in younger age groups. The rate of peri-procedural complications is comparable to other studies that analysed peri-procedural complications in nonagenarians [13-15,17,18], except the rate of coronary artery perforation. The rate of coronary artery perforation in our study population is high, compared to the literature where these rates range from 0.27% to 0.84% [24]. However, the reported mean age of the investigated patients ranges between 60-71 years, and older age is commonly considered as a risk factor [24]. In contrast, only one case of pericardial tamponade (< 1%) was reported in one study [14]. The rate of peri-procedural complications during TAVR was comparable to the results of Noble [23]. The rate of peri-procedural complications of the other procedural groups is not reliable due to their small patient numbers.
Compared to an age and gender matched Swiss population, survival after first percutaneous cardiac procedure in all analysed groups was similar. Survival-rate in our study population after urgent and elective coronary angiography seems to be comparable to previous study results [13,16-21]. However, the 1-month mortality of 5% after first procedure shows potential for better patient selection. The selection process whether (or not) to perform percutaneous cardiac procedures in our study population can not be assessed by our retrospective non-controlled study design.
It seems plausible that there is a strong collinearity between the 6 risk factors history of heart failure, NYHA functional class III or IV, LVEF < 40%, mild to severe mitral valve insufficiency and history of atrial fibrillation. However, the reliability of a multivariate survival analysis adjusting for 6 factors with a total of 46 deaths remains unclear. Similarly, the reliability of a multivariate survival analysis in the subpopulation after first coronary angiography is also unclear. Amazingly, renal impairment was not associated with a worse survival in our study population.
The practical consequence for patient selection regarding the risk factors mentioned above should be further evaluated by also assessing post-procedural symptom relief, which was not possible in our retrospective study.
The low amount of elective percutaneous cardiac procedures in the literature in this age group can be interpreted as result of overall low patient numbers, which are possibly further lowered by restrictive patient selection since there is yet little evidence about risk and benefit. The resulting number of nonagenarians not getting an appropriate interventional therapy remains unclear. We think that our retrospective single center study can not answer the important question about the individual benefit, but shows an acceptable estimated survival after percutaneous cardiac procedure in this age group. In this age group, improvement of survival is not the main focus but better quality of life. Regarding the yet small number of nonagenarians undergoing cardiac procedures, multi-center and prospective studies are required to get better knowledge about factors concerning risks and benefits in this age group, allowing general recommendations for these patients.
This was a single-center, retrospective study about a population being referred for percutaneous cardiac procedures. Therefore, there is certainly a significant referral and selection bias. Due to the retrospective design, data acquisition was limited, e.g. there was no prospective use of a frailty score. Considering the small number of patients and events, the reliability of a multivariate survival analysis is limited.
Nonagenarians undergoing elective and urgent percutaneous cardiac procedures at our center showed an acceptable survival considering the overall life expectancy in this age group. Length of hospitalisation for procedures regarding valvular heart disease are considerably longer than usually observed in younger age groups. In our study population, predictors of worse estimated survival after percutaneous cardiac procedure are history of heart failure, NYHA functional class III or IV, LVEF < 40%, mild to severe mitral valve insufficiency and history of atrial fibrillation. Further studies in this age group are required to delineate optimal patient selection for an acceptable ratio of procedural risk and benefit regarding survival and quality of life.
This research was funded by the HerzGefässStiftung but otherwise received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Two co-authors declare a potential conflict of interest: Christoph Scharf MD is stockholder of Acutus Medical Inc. and Olaf Franzen MD is a consultant of Edwards.
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content.