We present a case of incomplete Kawasaki disease (KD) in a 10-year-old child treated for bacterial cervical adenitis and retropharyngeal abscess. The child's older age and the lack of laboratory or signifying features contributed to the long delay in the diagnosis of KD on day 40 of illness.
Kawasaki Disease, Lymphadenitis, Node-first Kawasaki, Fever
A 10-year-old male was admitted to our hospital after worsening right-sided neck lymphadenitis and fever of 39.8 ℃ (103.6 ℉) of 7 days duration. He had been admitted to an outside facility and treated for 3 days with intravenous (IV) ampicillin/sulbactam and clindamycin, where a computed tomography (CT) revealed right sided lymphadenitis with no abscess formation. Blood and throat cultures showed no growth. Upon admission to our hospital, he had right neck swelling with tenderness and erythema. History was significant for no immunizations. Laboratory findings are summarized in the Table 1; serology for mumps, cat-scratch disease, Epstein-Barr virus, and cytomegalovirus infection were all negative. Fever resolved, the neck tenderness and size of cervical adenopathy improved, and he was discharged on IV clindamycin and ceftriaxone.
Table 1: Summary of laboratory results & treatment for case report. View Table 1
Five days later, day #17 of illness, the patient was readmitted with return of fever with worsening right and some left neck swelling, pharyngitis, and a transient macular rash on his face. CT revealed a right retropharyngeal abscess with bilateral cervical lymphadenitis (See Figure 1). Considerations for the etiology of the inflammatory neck mass included reactive lymphadenopathy, such as seen with Epstein Barr virus, cytomegalovirus, primary HIV, toxoplasmosis, and malignancy, as well as bacterial causes from S aureus, Streptococcus species, Lemierre's syndrome (Fusobacterium necrophorum), plague, tularemia, mycobacterial infection, and cat-scratch disease. Serology for Bartonella henselae (cat-scratch disease), Epstein-Barr virus, and cytomegalovirus infection in this patient were negative. He underwent incision and drainage of the abscess, as well as tonsillectomy and adenoidectomy. Tonsil and pharyngeal exudate grew coagulase negative Staphylococcus which was felt to be a contaminant; urine and blood cultures were negative. Family refused lymph node biopsy. As a result of severe airway swelling, he received a 5 day course of corticosteroids and remained on mechanical ventilation for 7 days. He was treated with 14 days of vancomycin, gentamicin, and ertapenem; neck swelling and fever resolved and was discharged home.
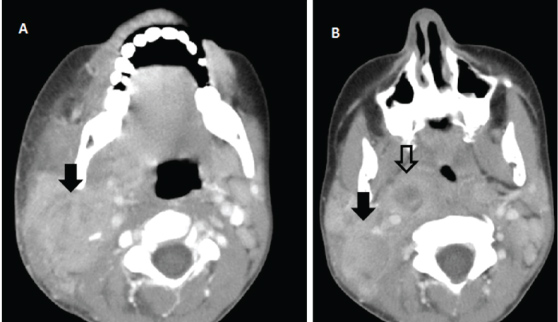 Figure 1: Computerized Tomography of the neck. A) Day #7 of illness with large right-sided cervical lymphadenitis (solid arrow); B) Day #17 of illness with continued right-sided lymphadenitis (solid arrow) and retropharyngeal abscess (open arrow). View Figure 1
Figure 1: Computerized Tomography of the neck. A) Day #7 of illness with large right-sided cervical lymphadenitis (solid arrow); B) Day #17 of illness with continued right-sided lymphadenitis (solid arrow) and retropharyngeal abscess (open arrow). View Figure 1
Nine days after stopping the antibiotics, on day #40 of illness, fever returned to 39.7 ℃ (103.5 ℉). Examination was significant for pallor and bilateral small cervical lymphadenopathy. Patient was readmitted to our hospital for a third time. Echocardiogram revealed aneurysmal enlargement of the coronary arteries: Left main coronary artery 10 mm (Z-score 31.04), left anterior descending (LAD) 10.4 mm (Z-score 26.13), and right coronary artery 12.5 mm (Z-score 25.11). American Heart Association (AHA) guidelines describe coronary artery aneurysms (CAA) as small (< 5 mm internal diameter), medium (5-8 mm), and giant (> 8 mm) [1]; Z-score in the LAD or RCA of 2.5 or greater are diagnostic of CAA [2].
Based on the presence of CAA, our patient was diagnosed with Kawasaki disease (KD) [3]. He was treated with aspirin and intravenous immunoglobulin (IGIV), solumedrol, heparin, and metoprolol. The diagnosis of KD is based on clinical criteria, including fever and ≥ 4 of the following: Non-exudative conjunctivitis, oral mucosa/lips/strawberry tongue erythema, maculopapular rash, cervical adenopathy, and changes in the extremities with desquamation; laboratory evaluation includes: Elevated acute-phase reactants, complete blood count (CBC), sterile pyuria, elevated serum alanine aminotransferase (ALT) level, and low serum albumin. Leukocytosis is common, with 50% of patients having WBC > 15.0 × 103/mm3. Thrombocytosis appears in 2-3 weeks of illness with platelet counts ranging 500-1,000 × 103/mm3. Risk factors for developing CAA include: Age < 1 year, long duration of fever, and low serum albumin [1,4,5].
Twenty percent of cases are classified as incomplete KD [1], which lacks of a common clinical phenotype; AHA guidelines suggest > 3 of the following criteria: Serum albumin < 3 g/dL, anemia for age, elevated ALT, platelet count > 450 × 103/mm3 after 7 days, WBC > 15.0 × 103/mm3, or urine WBC > 10/HPF. Incomplete KD is associated with a higher incidence of CAA and mortality as high as 41% [2,6].
Cervical adenopathy is the least common diagnostic criteria, noted in 50%-75% of Japanese, 42% to 52% of US, and 24% of Chinese cases [7]. Cervical adenopathy and fever may occur before other clinical signs, called node-first KD; in others, adenopathy dominates the presentation even in the absence of other signs until echocardiogram demonstrates characteristic coronary artery changes. Retropharyngeal edema and lymphadenitis have been recognized as occurring in patients with node-first KD, with overall frequency unknown [7].
A recent prospective study of node-first KD identified older age, elevated markers of systemic and hepatobiliary inflammation, and anemia for age as variables to help recognize the correct diagnosis, with mean age of children presenting with KD-cervical lymphadenopathy to be 4.9 years (range 2-9 years) compared to 2.2 years (range 0.2-3.7 years) without cervical lymphadenopathy [8]. In a multivariable analysis comparing children with bacterial cervical adenitis to children with node-first KD, smaller nodes, lower WBC, higher absolute band count, and a higher CRP were independently associated with node-first KD [9].
Patients presenting with fever and node-first KD are often mistakenly treated with antibiotics delaying the ultimate diagnosis of KD. Older age and lack of laboratory or signifying features of KD may contribute to delay in the diagnosis of KD. Clues to redirect thinking toward a diagnosis of KD are: A trial of empiric antibiotics without improvement, needle aspirates that showed negative cultures, and progression of lymph node swelling from unilateral to bilateral. The transient improvements and response to antibiotics in our patient suggested that bacterial infection was present; in addition corticosteroids ameliorated his clinical response, albeit transiently. Thus a high index of suspicion for Kawasaki disease must be maintained when high grade, remitting fever despite antibiotic treatment, is present in the setting of lymphadenitis [10].