Sever Acute Malnutrition (SAM) is a major health problem in developing countries especially among underprivileged and destitute life survivors population. It is more common among under-five children and responsible for accounting one-third deaths in worldwide. Information on SAM treatment outcome in therapeutic center at Benishangule Gumuze region is scarce. We assessed SAM treatment cure rate and associated factors among 6-59-month children at Pawe General Hospitals from February1, April 2, 2020.
Methods: We conducted institution based retrospective cohort study from January 2015 to December 2019 and collected data from February 1 April 02, 2020. Totally 454 SAM 6-59-month under-five children assessed with their known final treatment outcomes. The collected data were coded and entered in to Epi-Data version 3.1; then exported to STATA/se-14/R. Survival analysis used to check proportional hazard assumption for each variable and no variable schoenfeld test < 0. 05. Variable with AHR at 95% CI at P-value less than 0.05 considered as significant predictors for treatment outcome.
Result: We reviewed 502 SAM admitted 6-59-month children individual file records, 454 individual cards were included for final analysis. Sixty-five percent of 65.4% (95% CI: 50.1-69.2) admitted SAM children were treated and declared as cured, whereas 16.52% of case defaulted & 11.5% of children were died after admission. The median age and median cure time of SAM children found 2.2 years and 13 days (± 7) respectively. Children diagnosed marasmus (AHR = 1.56: 95% CI 1.08--2.2), No nasal-gastric intubation (NGT) during admission (AHR = 1.31: 95% CI (1.04 --1.67) and taking F-100 milk (AHR = 5.42 95% CI (2.92-9.85) were independently associated with treatment cure rate.
Conclusions: The overall treatment cure rate of this study was remaining low 65.4% as compared to sphere standard sets of reference humanitarian recommendation (i.e., > 75-77.9%), with previous studies done in Ethiopia. Based on this study finding starting formula F-100 milk, no NGT during SAM admission independently associated with treatment cure rate.
SAM, Under-five children, Treatment cure rate, Ethiopia
Childhood malnutrition is still a major global health problem, contributing to morbidity, mortality and risk for disability [1]. It refers to a combination of nutritional disorders that include underweight (mixed), wasting (acute), stunting (chronic) and micronutrient deficiency [2,3]. Wasting (weight for height) is an acute malnutrition due to a recent failure to receive adequate nutrition and may be affected by recent episodes of diarrhea and other acute illnesses [2] and chronic malnutrition might due to immune-compromisizations from complex, adaptive physiologic and metabolic processes secondary to insufficient nutrients [2]. Around 45%-60% of deaths for children less than 5 years of age were linked to under nutrition, while this is mostly occur in low- and middle-income countries makes most difficulty [1,4].
The current burden of malnutrition globally is unacceptably and every country in the world is affected by malnutrition since 2018 stunted children (aged 0-59 month (22.2%) 150.8 million wasted children 50.5 million (7.5%) & 38.6 (5.6%) million were over nutrition. Across the globe, SAM is responsible for the death of 3.6 million under five children and 140.5 million Disability Adjusted Life Years (DALYs) of children with estimated 2.3% loss in national gross domestic product [1]. Sever acute malnutrition is the top 3 killer for under five children 8.1% next to pneumonia and neonatal sepsis 15.3% with 20% of pediatric hospital admissions in Ethiopia and it is a reason for 25%-30% death in many poor country [5,6]. The problem of SAM is not only medical disorder rather it is also social disorder. Therefore, Successful management of severely malnourished patients requires both medical and social efforts [6]. Nationally in Ethiopia SAM treatment outcome at therapeutic center has good progressed i.e., 88.4% [5]. However cure rate report form different regions has still insufficient, Gonder referral hospitals 69.2% [2], in Bahir Dare referral Hospital 58.4% [6], North Gondar zone, 65.3% [7], Nekemte Referral Hospital 66.8% [8], South west Ethiopia 67.7% [9], Yekatitie 12 Hospitals in Ethiopia 81.3% [10], SNN of Ethiopia 87% [11] in Debre Markos and Finote selam Hospitals 77.9% [12]. Over the past fifteen year in Ethiopia's, the trend of malnutrition revealed that there is a reduction in stunting by 31% and underweight by 39% [6], by combination effort of Health center with hospitals treatment of Health center MAM by OTP &SAM by inpatient TFU [5]. However, in Benishangule gumuz there was only a small decline since 2000-2016 prevalence of stunting (from 50% to 38%), underweight (34% to 24%) and wasting reached (12% to 10%) [13]. Recovery from SAM treatment is remain challenging [2] and insufficient, and little is known about treatment cure rate and its associated factors in Ethiopia from SAM. Therefore, SAM continued being one of commonest hospital admission for pediatrics. The main aims of this study is to determine treatment cure rate and its associated factor among 6-59 months SAM children treated in stabilization center in Pawe general hospitals admitted since 2013-2018.
Hospital based retrospective cohort study was employed among 502 SAM 6-59-month children at Pawe general hospitals in Benishangule Gumuz regions in North West Ethiopia. Pawe general hospital was found in Metekel zone Pawe woreda distance of 565 km from Addis Ababa. This hospital gives medical treatment service for six woreda in Metekel zone & catchment area of Amhara regions. It has 221 beds; more than 31 beds shared by pediatrics wards; in pediatrics ward half of beds are reserved for treatment of SAM children [14]. In this, Hospitals there were totally 502 children started SAM treatment since 2015-2019. Those five consecutive years were purpo¬sively selected for SAM case's, give most recent information about the problem in under investiga¬tion malnutrition case [15,16].
The source populations were all SAM under-five children admitted to TFC for treatment since January 2015 to December 2019. 6-59-month SAM registered from January 2015 to December 2019 was study subject for this study. Data including socio-demographic information comorbidities; routine medications, individual files outcome not registered (i.e., cure, death, not recovered and defaulter) were excluded. Data were collected from February 1, April 02, 2020.
The sample size of this study was calculated based on survival sample size calculations from STAT/R 14 using the following parameter and formula [17]:
By using the following statics parameter α = 5%, Za/2 = Z value at 95% confidence interval = 1.96, Power (B) 80% = 0.84 Treatment cure rate (P1) = 79.2% [18] AHR = 0.32 [12].
Probability of event for those cured patient from sever acute malnutrition groups was with time specific since the study was last 5 years (2015-2019), exp (-ʎt) = exp(-0.5) = 0.6 [17] Similarly, the probability of the event for second group was calculated using exp. ( ʎt *AHR) [17,19]. By using AHR = 0.32. Thus, the probability of the event for the two groups becomes P (event) = 1- (0.32 + 0.5)/2 = 0.59 Thus, the final sample size was calculated 295. However, in Pawe general hospital since 2015-2019 totally treated SAM registered 6-59-month children were found 502.Since, we included all available and eligible recorded 502 data and no sampling procedure used.
Event (cured): Is computed as a number of SAM children discharged after cured or free from medical complication, ede¬ma and achieved sufficient MUAC (≥ 12.5 cm) and WFH (≥ 85%); these children were described as cured or recovered on their medical charts divided by the total number of SAM children admitted in TFC [2,20].
Kwashiorkor: Is severe under nutrition or malnutrition in children resulting from a diet excessively high in carbohydrates and low proteins.
Marasmus: Is under nutrition or malnutrition and emaciated that from inadequate taking of carbohydrate food or metabolic disorders.
Marasmus-kwashiorkor: Is the mixture of both kwashiorkor and marasmus. It is a problem of both carbohydrate and protein containing food deficiency.
A structured data abstraction tools was used for data collection purpose. The data abstraction tools were adopted from the Ethiopian federal ministry of health (FMOH) updated SAM management guideline in 2013 with medical history sheet & published study. Three diploma nurses and one-degree public health officer supervisor were recruited and full two-day training was given before data collection processes. All data collectors had taken updated SAM management training and currently working pawe general hospitals. For quality of data collection process, the principal investigator and one supervisor were followed data over all data collection process.
Data entered into the computer using EPI-DATA version 3.1 & exported to STATA 14.1 for cleaning and analysis. Descriptive analysis, such as tables, graphs, Kaplan Meier survival curve and log rank test was done. Hazard ratio with 95% CI & P ≤ 0.05 was used to measure association with independent variable. The overall survival graph and hazard failure estimated curve was used to show survival and hazed probability of risk group. Cox-regression model was fitted to identify associated factors. All associated with treatment cure rate in bivariable analysis at a hazard ratio of P-value < 0.25 included in multi variable Cox-regression. Variables with adjusted hazard ratio (AHR) in multivariable Cox-regression with their corresponding 95% confidence interval (CI) with P-value < 0.05 was considered as significant predictors. Cox-proportional hazard assumption was checked by (log-log plot) & expected versus observed Kaplan Meier graph test for each variable with schoenfield residuals test for each variable. No variables less than < 0.05. After multivariable cox regression was built by transforming from bivariable P < 0.25, for finally model selection was selected by AIC & BIC criteria [21]. Finally, Nelson Alana che and Cox Snell residual combination used for checking final model adequacy.
Ethical clearance was obtained from Ethical review Committee of College of medicine and Health Sciences department of public health in Debre Markos University. Pawe general Hospital also rechecked for ethical compatibility and permitted the data access. As the study conducted through a review of records, no consent was obtained from the mothers or caregivers of the study subjects.
From the total 502 SAM admitted 6-59-month children in TFC, 454 data were included for final analysis. 48 (9.6%) children files were discarded due to individual file incompleteness. The median age of children was 26.1 months (SD ± 17 month). From the total SAM children, 250 (55.07%) were female, majority 151 (33.26%) children were found in the age group of 6-11 month. More than two-third 348 (76.65%) of the study participant were from rural and pastoralist community. Nearly two third of 281 (62.9%) study participant were on breast-feeding when they admitted. Among the total study participant 369 (81.28%) were admitted as new case of SAM children with 348 (76.65%) diagnosed at hospitals.
Descriptive baseline result of SAM 6-59 moth children has at admission time, mean weight and MUAC of children during admission 8.08 kg (SD ± 3.48) and 11.5 (SD ± 6.98) respectively. From the total 454 included SAM children identified based malnutrition type, 251 (55.76%) were marasmus, Marasmus-Kwashiorkor 133 (29.3%) and kwashiorkor 70 (15.6%).
Among the total 251(55.26%) marasmus diagnosed SAM children in TFC, 9.9% cases were died, 64.9% cases were cured, 17.18% cases were defaulted and 8.1% cases were not cured and transferred out. Among the total 133 (29.3%) diagnosed Marasmus-kwashiorkor cases, 72.4% Cured, 12.9% died, 12.9% default and 4.3% not cured/recovered. From the total, 70 (15.86%) diagnosed Kwashiorkor cases, 15.3% died, 56.9% cured, 19.4% default, 8.4% were not cured.
Among 454 admitted SAM cases, 297 (65.4%) 95% CI (50.12-69.24) children declared as treatment cured in malnutrition registration log books, whereas 75 (16.52%) SAM cases were defaulted from therapeutic feeding center, 52 (11.45%) case were died during treatment, 31 (6.83%) SAM children not responded for SAM treatment Table 1.
Table 1: Performance indicator for TFU of Pawe General Hospitals as compared with sphere project based on 2016 standard (N = 454). View Table 1
Three hundred six (54.35%) under-five SAM admitted children in therapeutic feeding unit (TFC) has at least one form of co morbidity. Among diagnosed comorbidity, 67.3% cases of marasmus-kwashiorkor, 49.89% cases of marasmic & 45.4% cases of kwashiorkor has comorbidity during admission time. The most commonly diagnosed comorbidity were pneumonia 226 (48.8%), diarrhea 228 (50.1%), anemia 144 (31.8%), from the total 38 (8.71%) children were HIV positive, and all these case in the above described were prevalent comorbidity among admitted under-five SAM children in TFC at paw general hospital. During admission 371 (81.72%) SAM children has altered body temperature (≥ 37.5 °C) while, 211(46.48%) children has vomiting.
Management of admitted cases with severe acute malnutrition in the therapeutic feeding unit (TFC) was done in accordance with the national guidelines. From the finding of this study, 357 (78.43%) had given routing medication during inpatient treatment. Out of 228 (50.22%) diarrhea case, 220 (96.6%) case received zinc acetate. In addition to this the most frequently administered special medication was identified, amoxicillin 367 (80.84%), gentamycin-ampicillin 357 (78.47%), however 97 (21.06%) SAM children did not take any medication during admission time. From 454 admitted SAM children, 431 (94.93%), 404 (88.99%) and 381 (83.92%) were took formula F-75, dilute F-100 & F-100 milk respectively during inpatient waiting time. On the other hand, 96 (21.15%) from the total children has received/donated blood during inpatient treatment, similarly 105 (23.13%) children had resuscitate IV fluid during inpatient waiting time. Nearly half of 203 (45.1%) SAM children have NGT during treatment time. While 193 (42.51%) children has got deworming after admission Table 2.
Table 2: Medication distribution for 6-59-month age SAM under-five children in Pawe General Hospitals North-west Ethiopia (n = 454) 2020. View Table 2
Totally 454 SAM under-five children produce 5044 days of observation time in TFC obtained and the median cure time of SAM children in TFC was 13 days with (± 7) with minimum and maximum 2 & 29 days respectively. The median survival rate was found 55.84% (51.1-60.7). There is statically treatment cure rate difference between marasmic SAM under-five children and other malnutrition (P < 0.005), children taking F-100 milk with no taking and having nasal-gastric tube (NGT) during admission and no during admission Table 3.
Table 3: Treatment outcome based on indicators under-five children admitted by SAM in TFC, at Pawe general Hospitals since 2015-2019, North-West Ethiopia (N = 454). View Table 3
Among 454 admitted SAM children 297 (65.42%) cases declared as treatment cured in logbook whereas 157 (34.58%) cases were censored and had took 1727 person day risk time observation (Figure 1, Figure 2, Figure 3, Figure 4 and Figure 5).
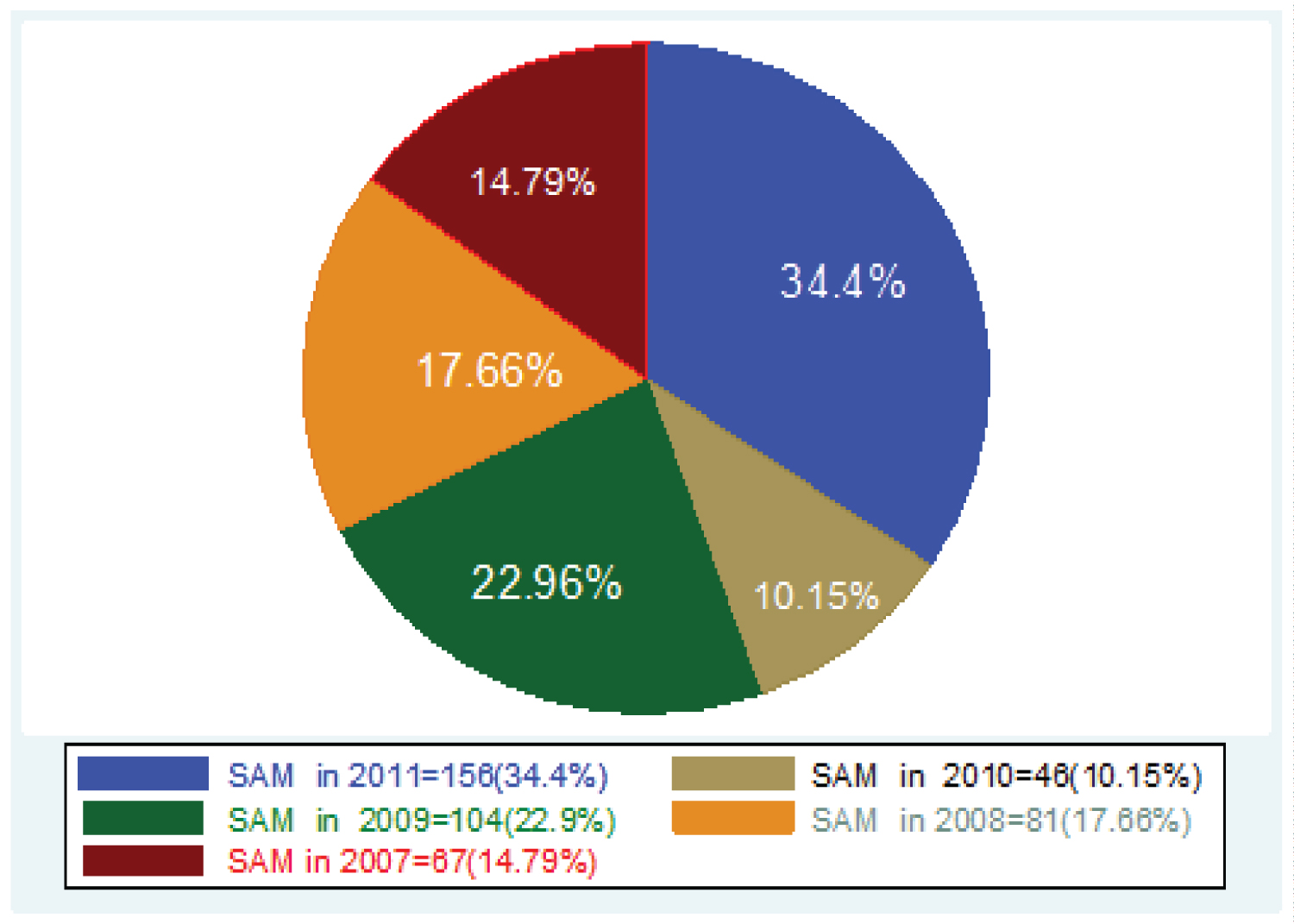 Figure 1: SAM 0-59-month children admission of based on year at TFU in Pawe general Hospitals since 2015-2019.
View Figure 1
Figure 1: SAM 0-59-month children admission of based on year at TFU in Pawe general Hospitals since 2015-2019.
View Figure 1
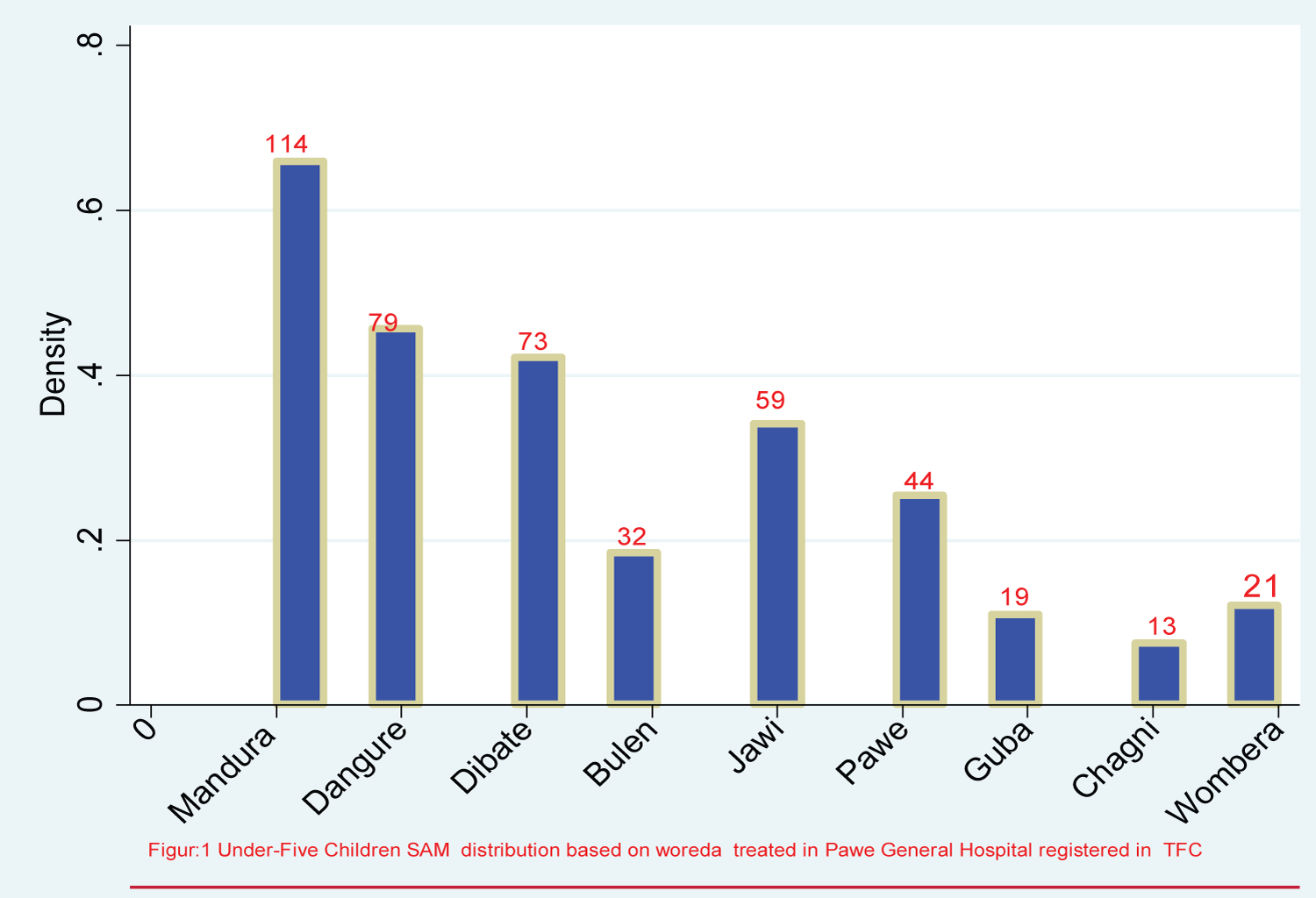 Figure 2: Under-five children SAM distribution based on woreda come for treatment in TFU Pawe General Hospitals since 2015-2019.
View Figure 2
Figure 2: Under-five children SAM distribution based on woreda come for treatment in TFU Pawe General Hospitals since 2015-2019.
View Figure 2
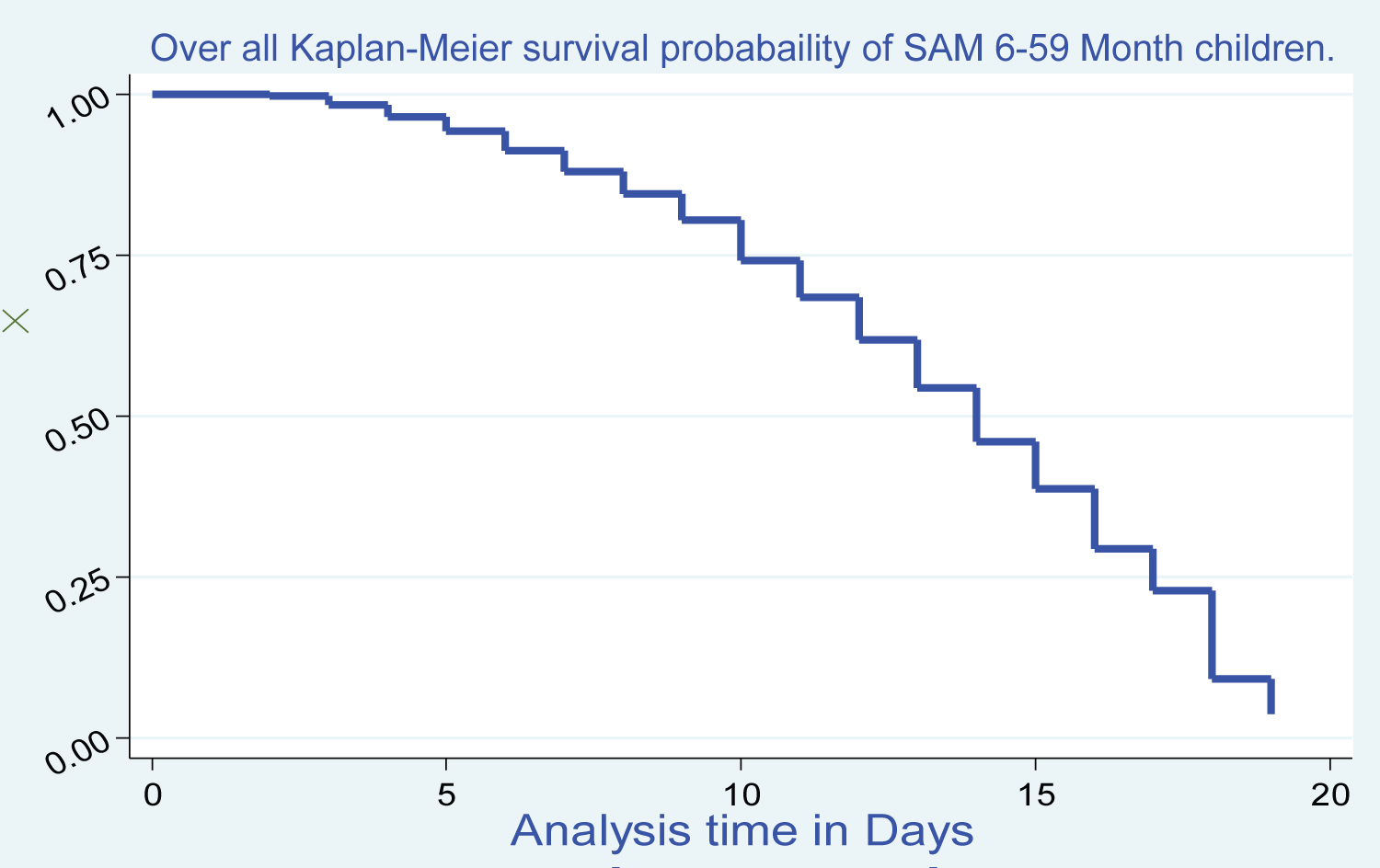 Figure 3: Overall Kaplan Meier survival probability of SAM 6-59-month children treated under TFU in Pawe general Hospitals North West Ethiopia; 2020.
View Figure 3
Figure 3: Overall Kaplan Meier survival probability of SAM 6-59-month children treated under TFU in Pawe general Hospitals North West Ethiopia; 2020.
View Figure 3
 Figure 4: Log rank survival estimations for treatment cure rate among SAM 6-59-month Children with NGT during admission at Pawe general hospital since 2015-2019.
View Figure 4
Figure 4: Log rank survival estimations for treatment cure rate among SAM 6-59-month Children with NGT during admission at Pawe general hospital since 2015-2019.
View Figure 4
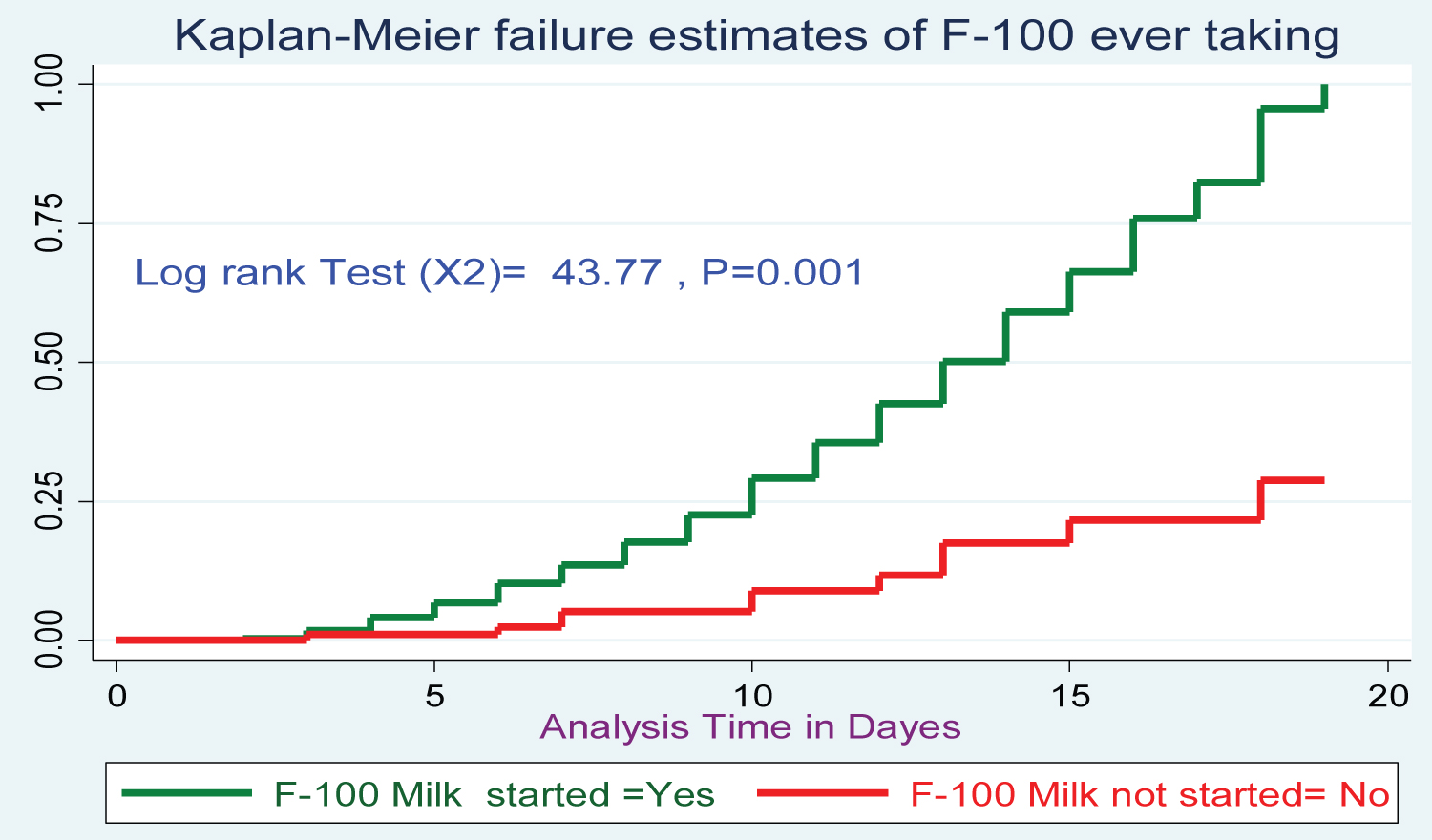 Figure 5: Log rank survival estimations for treatment cure rate among SAM 6-59-month Children with F-100 milk started after admission at Pawe general hospital since 2015-2019.
View Figure 5
Figure 5: Log rank survival estimations for treatment cure rate among SAM 6-59-month Children with F-100 milk started after admission at Pawe general hospital since 2015-2019.
View Figure 5
During bivariate analysis, 12 variables has P < 0.25 and transported in to multivariable Cox regression thus are, residence, sex, malnutrition types, vitamin A administration, comorbidity status, vomiting during admission, deworming, having anemia, having NGT during admission, diarrhea during admission, folic acids administration, routine antibiotic HIV status, were exported for multivariable Cox regression. After AIC and BIC mode comparison and checking by Nelson Alan and Cox Snell residual test of final model adequacy the following, variables found for final model Cox regression. However, after controlling for potential confounders in multivariable Cox regression analysis sex of children, residence of children, malnutrition types, Vitamin-A status, comorbidity status, NGT during admission, anemia during admission, F-100 after admission and deworming were found saturated for final model adequacy. There for SAM 6-59-month children being marasmic diagnosed were 1.56 times increased the probability of treatment cure as compared with counterpart (AHR = 1.56, 95%CI: (1.08, 2.27), P < 0.018. SAM under-five children with no NGT during admission had 1.31 times has higher probability of treatment cure than (AHR: 1.31(95% CI: 1.04 1.67 P ≤ 0.029) as compared children having NGT during inpatient. In addition, children taking F-100 milk after admission 5.42 time's higher probability of cure as compared to their counterparts SAM children or not taking F-100 milks (AHR:5.42 (95% CI: 5.42(2.92 9.85) P ≤ 0.001) Table 4.
Table 4: Bivariable and multivariable Cox-regression analysis of factors associated for treatment cure rate for SAM under -five children in Pawe general Hospitals 2020. View Table 4
This study-analyzed treatment cure rate and its associated factors among children 6-59-month age admitted SAM case. The finding of this study indicated treatment cure found 65.4% (95%CI: 50.12-69.24). Which is unacceptable and lower than sphere standards reference (i.e. exceed > 75%) [20]. But this is in line with the study finding of seven health center in Gonder 65.3% [7]. But not comparable with Nekemte Referral Hospital 66.8% [8], South west Ethiopia 67.7% [9], Yekatitie 12 Hospitals in Ethiopia 81.3% [10], SNN of Ethiopia 87% [11] the difference might be due to in socio-economic status, quality of health care provided for Children, therapeutic foods and medications [12], birth interval status ,decision making ability of mother for sick children [3]. Despite low treatment cure rate in Benishangule gumuze region < 5-year children SAM prevalence progressive against with time (49% lowered to 43% since 2011-2016) [13]. Thus, to achieve a better cure rate, increasing commitment to addressing and treating malnutrition based on standard protocol needs to be implemented properly [22]. Strengthening out-patient treatment programmed should tackle barriers to access outpatient treatment, encourage early identification of SAM, reduce inpatient caseloads and decrease the risks of cross-infection [20,22]. In fact, mismanagement of SAM in treatment center [23]. Likewise, current study indicated the median treatment cure time was lower than (i.e., 13 days) from sphere project (i.e., < 28 days) [20]. Median treatment cure rate of this study is 12.7 days. This is consistent with Debre Markos hospitals and Gonder referral hospitals [2,12]. However there is wide range of treatment cure rate difference when compared with study done in [6,9,11,18]. In fact this is due to the difference quality of health care provision Large-scale fortification of foods as a means of addressing micronutrient deficiencies [24]. However, in this study finding there is higher mortality rate 11.45%, this is incomparable with sphere reference [20]. The difference may be due to delay in seeking health care [2] and medical complication [5]. This study revealed that having marasmus diagnosed for SAM children increase the probability of cure rate as compared with kwashikore diagnosed children. This might be due to free radical electron in edematous patient increase & killed physiological intracellular electrolyte in addition associated easily with infectious disease [25]. Taking F-100 milks for SAM children during waiting in therapeutic center significantly increase cure rate. This is agreed with the study finding in Hawassa hospitals [26]. In fact SAM children, who did not received F-100 formula milk had increase 50% mortality rate compared with taking it [26]. In fact, F-100 formula milk has higher calorie 100 kcal/100 ml, which increases the daily weight gain and improves the outcome of children [26,27]. On the other hand, SAM children have no NGT during SAM admission, associated with treatment cure rate. The fact that having NGT during admission might bring cause complications (like; diarrhea, vomiting, constipation, lung aspiration, tube dislodgement, hyperglycemia and electrolytic alterations, this will hinder treatment cure rate [28].
This retrospective cohort study of multi-chart record review revealed that treatment cure rate is remaining low as compared to SPHERE standards also comparison with previous studies in Ethiopia. According to this study finding ever started F-100 milk and having no NGT during admission was swiftly increase treatment cure rate from SAM.
Benishangul Gumuze region Health bureau should to increase intensified screening children MAM at health center by adjusting intervention modalities for family for economic and food security in the region before that would address the identified factor are highly recommended for better treatment cure rate. A prerequisite organized of health team must make in TFC to improve infant to stepwise starting F-100 milks efforts making to avoiding NGT for feeding and medications after admission.
No consent for publications.
All the datasets analyzed for this study available in the corresponding author& in reasonable request we will sent it.
The authors declare that there are no competing interests.
Both authors covered funding of this research.
We would like to thanks both data collectors and supervisors.
Fassikaw kebede (FKB), the main author of this research currently working in lecturer of Epidemiology department, faculty of public health, institute of health science, Jimma University P.O. Box: 378 Jimma Ethiopia. Nemera Eticha (NE) is currently working in position of chief manager of Pawe general hospital, Benishangule Gumuze region, Metekel Zone Pawe.