The Dietary Approach to Stopping Hypertension (DASH) is considered first-line therapy for hypertension, yet clinical practice implementation remains suboptimal.
We designed a survey to assess four domains: (1) Provider beliefs/knowledge of DASH benefits, (2) Patient characteristics influencing likelihood of recommendation, (3) Practice barriers to provision of DASH diet advice, and (4) Resources of perceived value. The survey was sent to University of Colorado School of medicine primary care providers practicing in the Denver metro area.
The survey was sent electronically to 149 providers, with 49 (33%) responders. Most (65%) believed DASH diet is as effective at lowering blood pressure as adding a medication. The most common patient and practice barriers influencing the decision to provide DASH dietary advice included perceived low patient motivation (90%) or ability (86%) to implement DASH diet, lack of provider time (71%), and lack of patient-directed educational resources (67%). Resources providers identified as useful included resources accessible through the electronic medical record, (88%), a dietician (83%), and printed patient-education materials (59%).
Interventions to increase provision of DASH dietary advice should focus on identifying eligible patients, accessible and well-disseminated educational materials, and expanded access to evidence-based interventions involving dieticians.
Hypertension, Pre-hypertension, Physicians, Dietary approaches to stop hypertension, Attitude of health personnel, Delivery of health care, Implementation science, Health education
Hypertension contributes to 25% of cardiovascular-related morbidity and mortality, affects 29% of the US population [1], and is an area of focus for many healthcare systems, especially given it's prominence in many value-based programs. Lifestyle modification is first-line therapy for patients with elevated blood pressure (BP) (SBP 120-129 and DBP < 80), or stage 1 hypertension (SBP 130-139 or DBP 80-89) with an ASCVD 10-year risk of < 10% [1]. The Dietary Approach to Stopping Hypertension (DASH), first published in 1997, is proven to lower systolic and diastolic blood pressures by 4.5 to 7.8 mmHg and 2.6 to 3.7 mmHg, respectively, compared to usual diet controls in treated and untreated hypertensive patients [2]. This is comparable to the lowering of 6-9/4-5 mmHg with blood pressure medications such as lisinopril, amlodipine, or chlorthalidone [3].
Despite the DASH Diet's effectiveness, DASH diet education implementation into clinical practice is suboptimal. Less than 1% of U.S population consumes a diet consistent with DASH [4,5]. An NHANES study examined an individual's degree of adherence to target for the nine food categories outlined within the DASH regimen (total fat, saturated fat, protein, fiber, cholesterol, calcium, magnesium, potassium, and sodium) by using a DASH accordance score. Americans with diagnosed and undiagnosed hypertension met less than 3 out of 9 of these targets [6]. Amanual chart review of outpatient visits where blood pressures were in the elevated stage 1 hypertensive range at an internal medicine clinic in our own system found documentation of DASH diet counseling in only 2 out of 330 visits over a one-month period.
Multiple factors contribute to the low level of DASH diet implementation, including the US food environment, socioeconomic factors, clinical factors, and patient knowledge. The first step to a patient making lifestyle changes to reduce blood pressure is often advice from their physician. However, a host of barriers prevent physicians from recommending dietary and other lifestyle changes [7]. Physicians cite lack of time to provide proper counseling on general nutrition, perception that patients lack interest and motivation in making lifestyle changes, and lack of training in nutritional counseling as barriers to consistent provision of life-style advice to patients, though data specific to DASH diet is lacking [4,7]. One observational study showed provision of each additional lifestyle counseling point (e.g. smoking cessation, low-sodium diet) was associated with 2.05 min increase in visit length [8].
Regular provision of lifestyle advice, including DASH diet, could positively impact a large number of patients, and provider advice is a potentially influential, perhaps critical first step. Understanding of the most important provider perceived barriers to providing this advice could facilitate development of more effective resources. This study aimed to identify provider-identified barriers to provision of DASH diet to patients who may benefit for lowering of blood pressure.
This cross-sectional study was conducted from December 2019 to January 2020 at the University of Colorado Anschutz Medical Campus with General Internal Medicine, Family Medicine, and geriatrics providers. This study was reviewed by the Colorado Multiple Institution Review Board and granted exempt status.
The University of Colorado School of Medicine faculty providers who care for patients at 149 different family medicine, general internal medicine, and geriatric clinics across the Denver/Boulder metro area. The system uses Epicas an electronic medical record. Within this platform, patient educational materials related to hypertension, low sodium diet, DASH diet, and anti-hypertensive medication are available through a third-party vendor.
A self-administered questionnaire was developed based on qualitative interviews with five primary care providers that included open-ended questions covering four domains: (1) Provider beliefs/knowledge of DASH diet benefits, (2) Patient characteristics influencing the likelihood of recommendation, (3) Practice barriers to provision of DASH diet advice/education, (4) Resources that are or would be useful (Supplementary material). Interviews were conducted until data saturation was reached and no new information or themes were reported. Provider responses to the qualitative survey were compiled and used to inform a 7-item Likert-scale based self-administered questionnaire.
The survey link was sent via email to all eligible primary care providers in December, 2019, with a second request sent 10 days later. Survey data were collected electronically and anonymously. Descriptive statistics were used to describe provider-identified barriers to the provision of lifestyle advice, including the DASH diet.
Among 149 primary care providers who received the email, 49 (33%) responded to the survey (Table 1). Two thirds (n = 32, 65%) of providers believe that the DASH diet is at least as effective at lowering BP in adherent patients as adding medication. The most commonly identified patient-related barriers reported were low perceived patient motivation (90%) and low patient ability to implement the DASH diet (86%), while the most commonly identified practice setting barriers were lack of time and lack of patient-directed educational resources, with 71% and 66%, respectively, reporting these as somewhat or very significant factors.
Table 1: Survey questions and responses [n (%)]. View Table 1
Methods or resources providers reported using to educate patients about DASH diet included verbal education (39%) and electronic resources available through the EMR (27%). The resources they reported would be most useful were electronic materials accessible through the EMR (88%), dieticians (82%), and printed materials (59%).
The workflow providers deemed most appropriate for DASH diet education was having patients with hypertension or pre-hypertension and interest in making lifestyle changes attend a dietician-led class (86%); the majority of providers (57%) also approved of a process where hypertension and pre-hypertension patients receive DASH diet written materials during a hypertension or preventative visit.
Finally, 88% of providers believe that DASH diet advice should be provided to patients who might benefit from the DASH diet because they may only learn about DASH diet education through a healthcare provider (Figure 1).
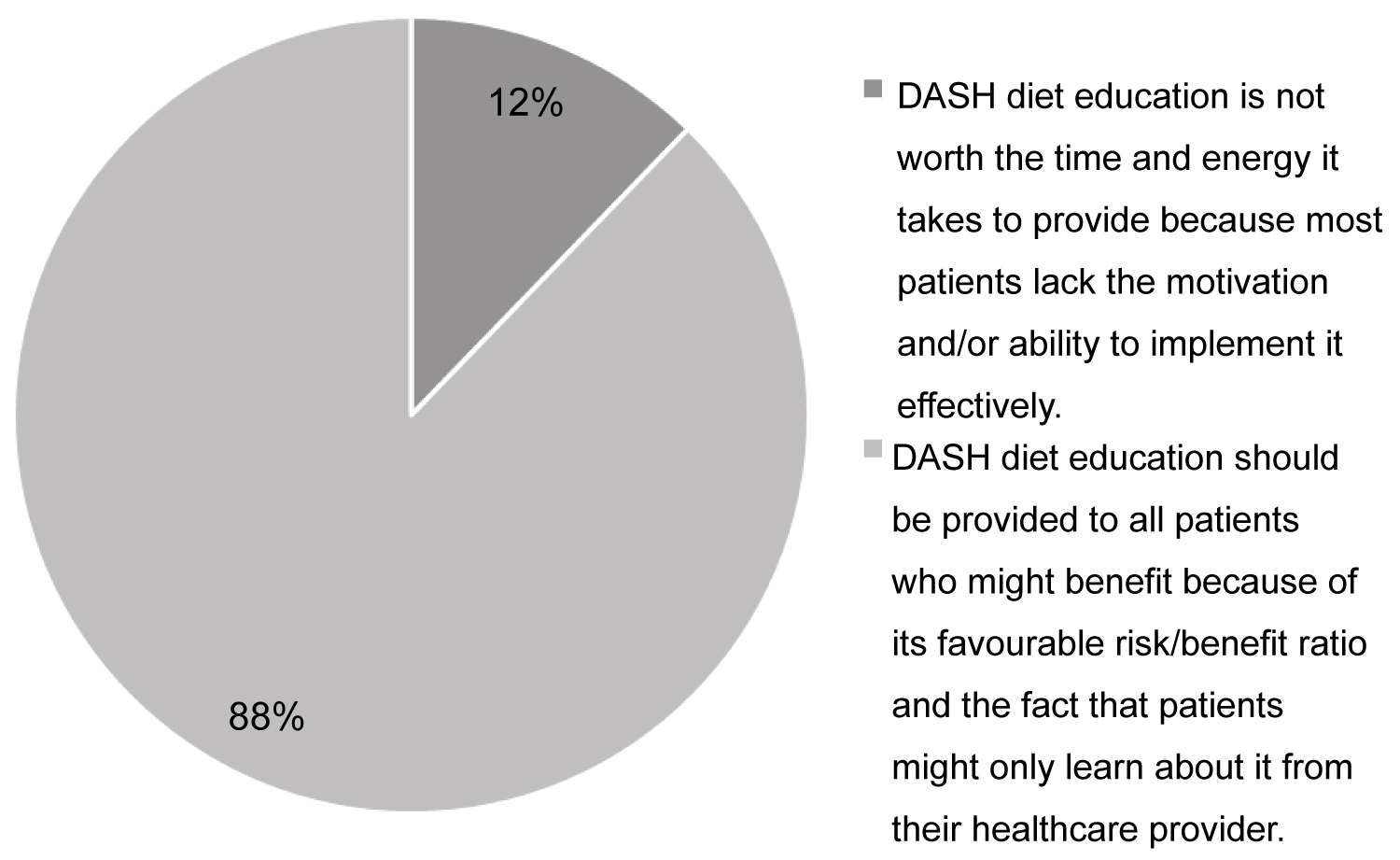 Figure 1: Provider survey: Please indicate which statement most closely resembles your opinion on providing DASH diet advice.
View Figure 1
Figure 1: Provider survey: Please indicate which statement most closely resembles your opinion on providing DASH diet advice.
View Figure 1
This study demonstrates that most primary care providers believe the DASH diet effectively reduces blood pressure. However, provider-perceived patient-characteristics, time, and lack or perceived lack of accessible patient education materials limit the provision of DASH diet counseling in pre-hypertension and hypertension patients likely to benefit.
Physician-perceived low patient motivation (90%) and ability to implement the DASH diet (86%) reflects previously-reported physician views towards nutritional advice in general [7]. Although physician perceptions don't necessarily reflect actual patient motivation or ability, there is evidence that cost, personal preferences, low availability of healthy foods, and cultural aspects are barriers to DASH diet adherence [9]. However, such barriers may be surmountable. An intervention involving multiple peer-group sessions involving shared DASH diet meal plans, grocery shopping ideas, and budget management increased fruit and vegetable intake compared to receiving only a DASH diet educational packet [10]. Thus, to improve the patient's ability to implement the DASH diet, a healthcare team and even supportive peer programs should be developed to provide individualized plans for patients to follow.
Lack of time for DASH counseling, reported by 71% of providers, is also comparable the 76-81% of providers reporting this as a barrier to any dietary counseling, despite the compelling evidence for DASH [8,11-13]. Thus, easily accessible educational resources that can be dispensed key, and were supported by survey respondents. Interestingly, DASH diet educational resources, already existed in our EHR, in Spanish and English, but were apparently unknown to survey respondents, given 66% reported their absence as a significant practice barrier. Thus an effective educational strategy must not just create resources, but also ensure providers are aware of and know how to use them.
Deficiency in nutrition training was identified as a barrier by just 38% of the physicians, though most medical students and educators consider current medical school nutrition education inadequate [12,13]. Providers universally endorsed access to dieticians to provide nutritional counseling, and outpatient DASH diet and exercise counseling by dieticians has demonstrated improved patient's cholesterol, blood pressure, and weight management [14]. More extensive interventions may be more effective, as evidenced by the PREMIER study, where multiple dietician-led group sessions improved DASH diet uptake and reduced blood pressure better than a 30-minute counseling session [15].
This study is limited by a relatively modest sample of university-based primary care practitioners. Second, this survey only examined the provider's perspective, limiting the view of patients. Third, the cross-sectional survey does not provide the relationship between the cause and effect of the response, limiting analysis of the result. However, this study has multiple supportive studies to mitigate this problem.
Providers identify perceived patient inability or unwillingness to implement DASH diet, lack of time, and real or perceived lack of accessible resources as significant barriers to advising patients to follow DASH. Interventions to increase provision of DASH dietary advice should focus on identifying eligible patients, accessible and well-disseminated educational materials, and expanded access to evidence-based interventions involving dieticians.
This research received no external funding.
All authors have contributed to the design and execution of this study, and the writing of this manuscript.