Background: In 2020, the rise in COVID-19 infections swept the United States in an unprecedented wave that has widely affected communities, particularly for older adults. Individuals with frailty syndrome have increased adverse outcomes from COVID-19, and conversely, individuals following post-infection are at greater risk of developing frailty. Data from the 2020 CDC National Health Interview Survey for those 65 years and older assessed prevalence of functional, behavioral and affective limitations associated with frailty risk factors.
Methods: Retrospective analysis of data collected by the CDC as part of their 2020 annual National Health Interview Survey using prospective sampling methods. Participants of study consisted of 1478 responses (5% of total responses collected). A nonparametric analysis was conducted using Kruskal Wallis (p < 0.05) and post hoc comparisons with Bonferroni's adjustment was performed for three cohorts over the age of 65, those who: Tested negative for COVID-19; tested positive for COVID-19 with zero to mild symptoms; and tested positive for COVID-19 with moderate to severe symptoms.
Results: Older adults with moderate to severe symptoms of COVID-19 demonstrated significant limitations associated with frailty risk, including feelings of tiredness, self-care limitations, and anxiety/depression compared to those negative for COVID-19. Having COVID-19 also resulted in a significantly greater need for walking assistance.
Conclusions: Prevalence for limitations associated with frailty factors is greater in the community-dwelling older adult following COVID-19 infection, with symptom severity as a risk indicator. An effective follow-up screening performed at post-acute care discharge may help identify the occurrence and prevent the progression of frailty syndrome in the older adults compromised by COVID-19.
Geriatric medicine, Pandemic, Covid-19, Frailty factors, Community-dwelling outcomes
Frailty among the older population has long been identified as a significant contributing risk factor for morbidity and mortality outcomes [1]. This is of clinical consequence because the older adult, "Baby-boomers", defined as those born between 1946 and 1964, is increasing rapidly within the U.S. population [2]. In addition, frailty has also been suggested to increase the propensity for vulnerability in older adults who have been affected by COVID-19 [3,4], even if not present prior to infection.
Frailty is a phenomenon known as a type of geriatric syndrome characterized by a functional decline across multi-organ systems that can result in increased vulnerability for adverse prognostic outcomes [5,6]. A commonly used construct to define this phenomenon known as Fried's frailty phenotype has proposed five key domains contributing to the frailty status: self-reported exhaustion, slow walking speed, weakness (grip strength), weight loss (defined as 10 pounds in the past year), and decreased physical activity. If three or more of these criteria were present, frailty as a clinical syndrome is considered to be met [7]. If two of these criteria are met, then the pre-frailty condition is presented according to Fried's model [8]. In a separate study, chronic pain has also been suggested to predict frailty in older adults compared to those reporting no pain [9].
Chronological age is not a pre-determinant for becoming frail and can exist in young, middle-aged [10], and older adults. In addition, the prevalence of pre-frailty has been reported to exist in 35% to 50% of individuals over the age of 60. Pre-frailty was reported to be more common in women, but age and number of comorbidities were comparable between frail and pre-frail individuals overall [11]. Unfortunately, signs of frailty are often missed due to their overlapping yet physiologically distinct processes [12], particularly in community-dwelling older adults [13].
The development of frailty syndrome has also been closely linked to affective behavior, particularly depression [14]. Reciprocal interaction has been reported to exist between depression and frailty noted in older adults [15]. When anxiety existed as a comorbidity to depression in older adults, higher odds of being pre-frail and frail were higher than those without those symptoms [16]. These psychosocial behaviors can lead to self-isolation or removal of oneself in a socially isolated manner, thus further exacerbating the risk towards the development of frailty [6,17,18].
Concerns for risk of frailty due to long-term effects of post-acute COVID-19 infection are significant since recovery from the infection is often followed by longer-term recovery of clinical symptoms, sometimes referred to as "long haul" COVID-19 presentation. For example, extended hospitalizations of older adults due to severe COVID-19 infection have been reported to result in a negative change in health-related quality of life (HR-QoL) six months following hospitalizations, with one out of three experiencing impaired mobility, poor self-care ADL abilities, and a negative change in cognitive function [19]. The potential benefit of this study is to identify if physical therapists are utilizing best practice when evaluating individuals that may be suffering from frailty or pre-frailty syndrome. As part of a standard physical therapy evaluation, all patients, should be screened for risk factors. Appropriate patient management will improve various health outcomes including those related to quality of life and reduce overall healthcare costs.
Because of the ongoing pandemic crisis due to COVID-19, several studies have supported the use of frailty assessment measures, such as the Clinical Frailty Scale, to determine the optimal allocation of resources and care [20]. Adding this type of vulnerability as part of the triage process in the acute care setting can provide more accurate estimates for the prognosis in acutely affected older patients, serving as an independent predictor for mortality in these individuals [21]. Whether any screen is more appropriate than another is dependent upon which clinical presentations are most prevalent in these vulnerable populations.
With the recent release of the 2020 CDC National Health Interview Survey [22], it is now possible to relate functional community outcomes data for older adults following post-COVID infection to factors associated with frailty and pre-frailty syndrome. Understanding the relationship between these two phenomena may provide insight as to the potential functional limitations that can a rise post-COVID necessitating more timely screening, referral, and follow-up for older adults, particularly regarding the identification frailty syndrome.
Data for the present study were drawn from the Center for Disease Control and Prevention (CDC), using the recently released 2020 annual National Health Interview Survey (NHIS) on the health of the community dwelling, non-institutionalized population in the United States. A total of 31,569 respondents comprised of all ages participated in the survey. From this total, 1478 were over the age of 65, reported to have taken the COVID-19 test and reported receiving test results. From the total who received test results, the sample size consisted of 80 individuals who reported receiving a positive test result for COVID-19. Data was analyzed for three cohort groups: (G1) Tested negative for COVID-19, (G2) tested positive for COVID-19 with zero to mild symptoms, and (G3) tested positive for COVID-19 with moderate to severe symptoms. Although this national survey has historically been collected via in-person interviews and follow-up, the NHIS shifted to all-telephone interviewing in March 2020 because of the COVID-19 pandemic. According to their website, in July 2020, the "NHIS was able to resume in-person interviewing but continued to conduct the survey mostly by telephone through December 2020". Because of this transition in the data collection method, the overall number of respondents decreased from previous years.
In addition, the survey data were collected and analyzed according to their individual alignment with characteristics that most closely reflected Fried's phenotypes for frailty/pre-frailty or for other factors that have been associated with contributing towards frailty or pre-frailty syndrome (i.e., depression, anxiety, chronic pain, and ability to self-care) (Table 1).
Table 1: Analyses of NHIS responses as related to "risks of frailty" domains. Older adults over the age of 65 years of age were compared in their responses to questions related to factors for frailty risks using NHIS survey questions. G1= Respondents who had tested negative for COVID-19; G2= Respondents who had tested positive for COVID-19 with zero to mild symptoms. G3= Respondents who had tested positive for COVID-19 with moderate to severe symptoms. View Table 1
Those survey questions were as follows:
A) In the past 3 months, how often did you feel very tired or exhausted? Would you say never, some days, most days, or every day? (Answers: Never (1), Some days (2), Most days (3), Every day (4), Refused (7), Not ascertained (8), Don't know(9))
B) Thinking about the last time you felt very tired or exhausted, how long did it last? Would you say some of the day (1), most of the day (2), or all of the day (3)?
C) Do you have difficulty walking or climbing steps? Would you say no difficulty (1), some difficulty (2), a lot of difficulty (3), or you cannot do this at all (4)?
D) Do you use any equipment or receive help for getting around? Yes (1), No (2)
E) How often do you do moderate-intensity leisure time physical activities?
F) Frequency of moderate physical activity (times per week)?
G) How often do you feel depressed? Would you say daily (1), weekly (2), monthly (3), a few times a year (4), or never (5)?
H) Thinking about the last time you felt depressed, how depressed did you feel?
I) How often do you feel worried, nervous or anxious? Would you say daily (1), weekly (2), monthly (3), a few times a year (4), or never (5)?
J) Thinking about the last time you felt worried, nervous or anxious, how would you describe the level of these feeling? Would you say a little (1), a lot (2), or somewhere in between (3)?
K) Do you take prescription medication for depression? Yes (1),No (2), Refused (7), Not ascertained (8), Don't know (9)
L) Do you take prescription medication for these feelings (worried/nervous/anxious feelings)? Yes (1),No (2), Refused (7), Not ascertained (8), Don't know (9)
M) In the past three months, how often did you have pain? Would you say never (1), some days (2), most days (3), or every day (4)?
N) Over the past three months, how often did your pain limit your life or work activities? Would you say never (1), some days (2), most days (3), or every day (4)?
O) Over the past three months, how often did your pain limit your family activities? Would you say never (1), some days (2), most days (3), or every day (4)?
P) Thinking about the last time you had pain, how much pain did you have? A little (1), A lot (2), Somewhere in between a little and a lot (3), Refused (7), Not ascertained (8), Don't know (9)
Q) Do you have difficulty with self-care, such as washing all over or dressing? Would you say no difficulty (1), some difficulty (2), a lot of difficulty (3), or you cannot do this at all (4)?
R) Over the past three months, did you use any of the following to manage your pain? Physical therapy, rehabilitative therapy, or occupational therapy? Yes (1), No (2)
S) Over the past 12 months, did you receive physical therapy, speech therapy, rehabilitative therapy or occupational therapy? Yes (1), No (2), Refused (7), Not Ascertained (8), Don't know (9)
Descriptive analyses were conducted for the sample demographic characteristics. In this study, nonparametric statistics were performed using Kruskal Wallis (p < 0.05) to rank and assess the differences between ordinal data responses for each aggregate group of those who tested positive for COVID-19 and had zero to mild symptoms; those who tested positive for COVID-19 and had moderate to severe symptoms; and those who did not test positive for COVID-19 after taking the test) for each of the survey questions (A-S) listed. When significant differences were identified using Kruskal Wallis, post hoc pair-wise comparisons were performed using Bonferroni's adjustment of significant values. All data analyses were conducted using SPSS v. 27.0 statistical software program.
For the 2020 NHIS survey, the aggregated total number of responses were comprised of 31,569 participants from non institutionalized communities who provided responses to the NHIS survey. Out of these, 10097 respondents reported their age to be 65 years or over.
Out of the total population of individuals who were 65 years old and older, 1478 respondents reported having taken the COVID-19 test and reported receiving test results. Out of those 1478 respondents, 80 individuals reported receiving a positive test result for COVID-19.
In this current study, the independent variables were determined by the COVID-19 status and symptom severity with three categories identified. The group that took the COVID-19 test and received a negative result was designated as Group 1 (n = 1398). Groups 2 and 3 were designated according to respondents' answers to the question of "How would you describe your coronavirus symptoms when they were at their worst?" Those respondents who reported having had no or mild symptoms were pooled together and designated as Group 2 (n = 36). Those respondents who reported having moderate to severe symptoms were designated as Group 3 (n = 44). (Table 1)
1398 reported having had no symptoms (Group 1), with 599 male and 799 females responding.
35 reported having mild symptoms (Group 2), with 20 male and 16 females responding.
44 reported having moderate symptoms (Group 3), with 20 male and 24 females responding.
The remainder of the responses available for individuals over the age of 65 were not considered in this analysis, since it was unclear as to what their status was with respect to having had COVID-19 infections since they did not take a COVID-19 test.
Each of the survey questions were analyzed to determine significant differences between the three groups (Table1). The findings from these analyses indicated that when considering each of the potential "risks of frailty" (Figure 1).
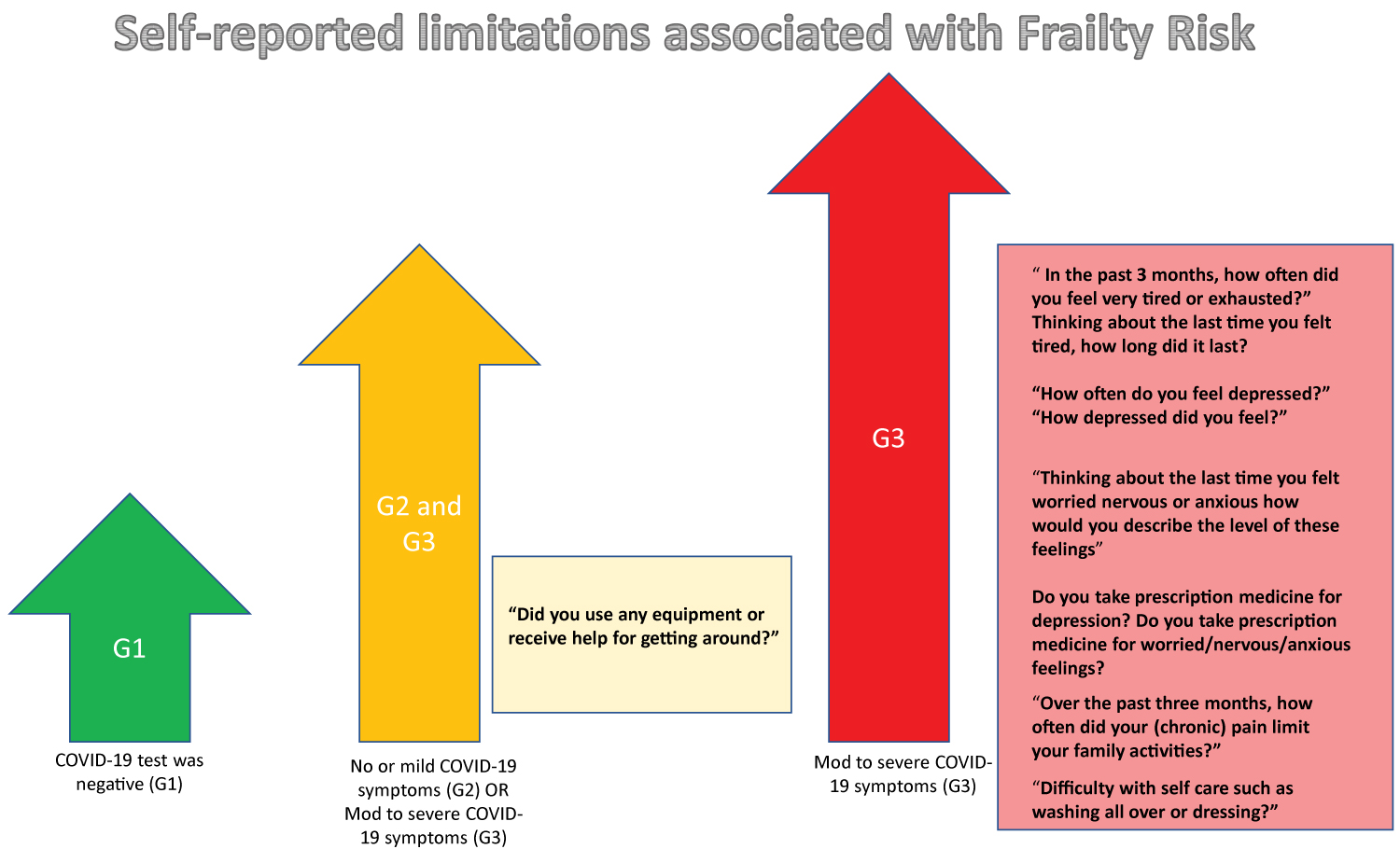 Figure 1: Self-reported limitations associated with Frailty Risk.
View Figure 1
Figure 1: Self-reported limitations associated with Frailty Risk.
View Figure 1
Respondents who had reported having moderate to severe symptoms of COVID were significantly more compromised compared to those who had experienced zero to mild symptoms of COVID infection or had not had COVID (nor reported experiencing any COVID-like symptoms).
1) For the question regarding "how often did you feel tired or exhausted?", respondents from Group 3 (moderate to severe symptoms during COVID-19 infection) were overall more significantly (p < 0.001) compromised compared to Group 1 (tested negative for COVID-19), whereas respondents from Group 2 (no or mild symptoms during COVID-19) were not significantly different from either group.
2) For the question stating: "Thinking about the last time you felt very tired or exhausted, how long did it last?" respondents from Group 3 were more affected longer than either Group 2 or Group 3.
Although respondents did not differ in their reports of having difficulty walking or climbing steps, those respondents who had reported moderate to severe symptoms of COVID did require more assistance in "getting around."
1) "Did you use any equipment or receive help for getting around?"
Although no significant differences were noted for respondents self-reporting difficulty walking or climbing steps, both groups that tested positive for Covid-19 (Groups 2 and 3) had overall greater reports requiring equipment or assistance in locomotor function than Group 1.
Respondents from all three groups were not significantly different from each other with respect to the amount of moderate-intensity physical activity engaged.
Respondents who had experienced moderate to severe symptoms of COVID-19 were noted to report significantly greater frequency of feeling depressed with greater intensity as well as a greater intensity of anxiety when compared to those who did not have COVID-19 or, in some cases compared to those who had reported zero to mild symptoms of COVID-19. In addition, this same group (Group 3) reported taking medication for depression and/or anxiety more often than those individuals who did not have COVID-19.
1) "How often do you feel depressed"
Group 3 (who had reported having moderate to severe symptoms of COVID-19) had significantly (p < 0.05) higher frequency of depression than those who did not have COVID-19.
2) "Thinking about the last time you felt worried nervous or anxious how would you describe the level of these feelings?"
Group 3 (who had reported having moderate to severe symptoms of COVID-19) had significantly more intense feelings of depression than Group 2 (with mild to moderate symptoms of COVID-19, p < 0.05) and Group 1 (no COVID-19, p < 0.05) respectively.
3) Although all three groups did not differ significantly in the frequency of experiencing anxiety-like symptoms ("How often do you feel worried, nervous or anxious?"), when asked to describe the intensity of these feelings, Group 3 (who had reported having moderate to severe symptoms of COVID-19) had significantly more intense feelings of these feelings than either Group 2 (those with zero to mild symptoms of COVID-19) or Group 1 (tested negative for COVID-19).
4) Group 3 (who had reported having moderate to severe symptoms of COVID-19) also reported taking prescription medication more than Group 1 (tested negative for COVID-19) for depression (p < 0.05) and worried/nervous/anxious feelings (p < 0.05), respectively.
Respondents between all three groups did not report a difference in the frequency of pain nor a difference in limiting life or work activities. However, Group 3 (who had reported having moderate to severe symptoms of COVID-19) stated their pain affected their family and significant others more than Group 1 (those who tested negative for COVID-19).
Respondents from Group 3 (who had reported having moderate to severe symptoms of COVID-19) reported having greater difficulty with at least 1-2 basic activities of daily living compared to those Group 1 respondents who had tested negative for COVID-19.
1) "Difficulty with self-care such as washing all over or dressing?"
Group 3 (who had reported having moderate to severe symptoms of COVID-19), (p < 0.05) was significantly more compromised in this domain from Group 1 (had tested negative for COVID-19).
Despite any differences in functional limitations noted in the domains assessed, respondents did not differ significantly from each other in reporting accessing allied health services.
The findings reported in this study suggest and corroborate the expectation that older adults who have been infected with COVID-19 may be at greater risk for developing clinical symptoms of pre-frailty or frailty, particularly if the clinical symptoms experienced were moderate to severe in presentation. Although limited by the wording provided within the NHIS survey questions, similar domains such as feelings of "tiredness," physical activity, and need for equipment or assistance in walking can be related to those given by Fried's frailty phenotype. Individuals who report, for example, a need for equipment or assistance in walking may be anticipated to have a "slower gait" than those who do not report a similar requirement.
In addition, co-morbidities of depression and anxiety have also been reported to increase the risk of developing frailty syndrome. In individuals who have had moderate to severe clinical symptoms of COVID-19, these emotions are more prevalent, as is the need for prescription medication to treat anxiety and depression. Additionally, the ability for self-care in these individuals is more compromised compared to individuals who had minimal or no clinical presentation of COVID-19. Whether this is due to physical or cognitive functional limitations is unclear. Other parameters noted to have been affected in older adults following COVID infection, such as the increased impact on family and significant others due to chronic pain, are problematic since this may lead to increased difficulty in social engagement.
These factors have been indicative of negative prognostic determinants of the frail condition [6,17,18] and may place older adults who experienced greater symptom severity during acute COVID-19 infections at greater risk. A still yet undetermined but important consideration is the effect prolonged or recurrent symptoms of COVID-19 may have on the older adult "long-hauler" population.
In 2020, the literature reported that older adults 65 years of age and older accounted for 16% of the US population but represented 80% of COVID-19 deaths in the US as well as the most at risk of becoming seriously ill. Hewitt, et al. (2020) [23] reported that in-hospital screening of frailty in patients who had been admitted with COVID-19 was a better predictor of disease outcomes than either age or comorbidity alone. In-hospital screening for frailty at time of acute infection may not be sufficient to identify the older adult who may still be at risk at the time points later than the acute episode. Clinical sequelae for "long-hauler" presentation have been induced in 10% of older adults who experienced mild symptoms [24].
The advantages of using self-reported questionnaires include rapid delivery of survey instruments to large communities; in the case of the current NHIS survey, the overall sample size included over 31,568 respondents who were interviewed in-person and via telephone. However, self-reported data is sometimes associated with response bias, as is the case for interventional studies where people may feel inclined to respond in a "per the norm" of what they expect their responses to be. Adjusting strategies to offset inherent bias associated with self-reported data can be helpful, including the use of repeated trials [25]. At this time, the 2020 NHIS survey yielded a limited available dataset coinciding with the increased incidence of COVID-19 cases in the United States. Further analysis with increased aggregated responses will be possible when the 2021 CDC NHIS dataset is available.
In addition, self-reported responses are not necessarily accurate assessments of clinical impairments since diagnostic criteria for medical conditions (e.g., for affective disorders such as depression) can only be accomplished through careful clinical evaluation by qualified practitioners. For this reason, the study findings support the recommendation for clinical follow-up and appropriate medical referral in older adults after post-COVID-19 infection, particularly in those who have experienced moderate to severe clinical presentation rather than to suggest direct links to frailty and pre-frailty syndrome following COVID-19 infection in this population.
Timely and effective screening tools for measuring parameters related to frailty may decrease the risks associated with this clinical syndrome. For instance, the Cardiovascular Health Study (CHS) indicator proposed by Linda Fried in 2008 covers the five domains- grip strength, gait speed, level of tiredness, physical activity and unintentional weight loss [7] and has shown to bean effective screening tool when combined with other assessments [26]. In addition, psychosocial screens for anxiety and depression, such as the Geriatric Depression Scale [27] and State-Trait Anxiety Inventory [28], should also be implemented to identify psychological morbidity in the older adult acute post-COVID recovery. Health related quality of life (HRQOL) is of paramount importance to promote healthy aging. When appropriate, a comprehensive geriatric assessment should be completed that includes a multidimensional and multidisciplinary approach, involving various health care professionals in the assessment of frailty and pre-frailty in the elderly. It falls within the scope of physical therapy practice to evaluate the functional limitations of an older adult and address them with a coordinated plan with members of the health team providing care to the patient to optimize overall health with aging [29].
Since many older adults do not have adequate family or social support to deal with the stress of COVID-19, follow-up care following discharge from hospitalizations is critical for these individuals, including from nurse practitioners who may be able to identify early signs of post-COVID morbidities, including cardiovascular and neurological complications [30]. Therefore, resources to determine the underlying support constructs are necessary for the older adult following discharge from acute medical care following COVID-19 infection, with appropriate referrals for follow-up through social services to avoid the development of self-isolation and possible development of pre-frailty/frailty conditions. The potential benefit of this study is to identify if physical therapists are utilizing best practice when evaluating individuals that may be suffering from frailty or pre-frailty syndrome. As part of a standard physical therapy evaluation, all patients, should be screened for risk factors. Appropriate patient management will improve various health outcomes including those related to quality of life and reduce overall healthcare costs.
The content of this manuscript was developed without funding or sponsorship.
The authors confirm contribution to the paper as follows: Developed the concept, study design, and data analyses: Kume. Acquired the data and validated the statistical analyses: Luo. Provided refinement of concepts, contributing content relevant to expertise in epidemiological research: Jumbo. Validated and refined underlying clinical concepts relevant to patient care management of older adult population: Voltmer. All authors reviewed the results and approved the final version of the manuscript.
The authors have no conflicts.