Background and aim: COVID-19 could be a fatal illness especially among older adults. The study aims to determine predictors of in-hospital mortality in older patients with COVID-19.
Methods: A retrospective cohort study including 138 older adults (age ≥ 60 years) with confirmed infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) by the real-time reverse-transcriptase polymerase chain reaction (RT-PCR). These patients were newly admitted to Geriatrics hospital for isolation from December 25, 2020, to April 2, 2021. Demographic, clinical and laboratory data were extracted from medical records. The primary outcome was in-hospital mortality. Logistic regression analysis was done to test the association between in-hospital mortality and potential predictors including age, gender, clinical presentations, comorbidities and laboratory data on admission including serum C-reactive protein (CRP), ferritin, D-dimer, basic biochemistry and complete blood count (CBC) to derive a predictive model. The discriminative ability of the model was evaluated by using the Receiver operating characteristic (ROC) curve.
Results: Overall in-hospital mortality was 54.3%. Multivariate regression analysis revealed independent predictors of mortality including blood urea nitrogen (BUN) with an odds ratio (OR) of 1.080; 95% CI: 1.028-1.134; P 0.002 and CRP with an OR of 1.012; 95% CI: 1.003-1.021; P 0.010. They were combined into a prognostic model with an area under the ROC curve of 0.842; 95% CI: 0.758-0.925; P 0.000).
Conclusion: Serum BUN and CRP on admission were predictors of in-hospital mortality in older patients with COVID-19. It provides a predictive model which needs validation in other multicenter prospective studies.
Mortality, Predictive model, Geriatric patients, COVID-19
SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; RT-PCR: Real-Time Reverse-Transcriptase Polymerase Chain Reaction; CRP: C-Reactive Protein; CBC: Complete Blood Count; ROC: Receiver Operating Characteristic; OR: Odds Ratio; LOS: Length Of Stay; CCI: Charlson Comorbidity Index; BUN: Blood Urea Nitrogen; AST: Aspartate Transaminase; ALT: Alanine Aminotransferase; TLC: Total Leucocyte Count; NLR: Neutrophil-Lymphocyte Ratio; LDH: Lactate Dehydrogenase; DM: Diabetes Mellitus; CVA: Cerebrovascular Accidents; CKD: Chronic Kidney Disease; CLD: Chronic Liver Disease; GI: Gastrointestinal; 95% CI: 95% Confidence Interval; AUC: Area Under the Curve
As of 28 May 2021, there have been 168,599,045 confirmed cases of COVID-19, including 3,507,477 deaths, according to World Health Organization [1]. Unfortunately, there is a deficiency of data regarding predictors of mortality in Geriatric patients with SARS-CoV-2 infection [2]. COVID-19 is characterized by poor outcomes especially among older patients [3]. Older age has been identified as an important risk factor for the severity of the disease, with increasing rates of death across every decade of life [4]. The higher mortality in older adults could be explained by the presence of comorbidities and the presence of certain presentations such as functional decline and delirium [5,6].
There are several reported predictors of in-hospital mortality in older Patients with COVID-19 such as certain laboratory indicators such as serum albumin level, altered renal functions and haemoglobin levels [5,7]. Also, a higher concentration of inflammatory markers such as serum LDH level and CRP were predictors of mortality in older adults [5].
This study aims to identify predictors of in-hospital mortality among older patients with COVID-19 through investigating the potential prognostic role of age, gender, COVID-19 related symptoms, comorbidities and certain laboratory markers on admission.
A retrospective observational study including older patients who were admitted to Geriatrics hospital for isolation from December 25, 2020, to April 2, 2021. Geriatrics Hospital is a tertiary care University hospital, designated for medical care and isolation of Covid-19 cases. Inclusion criteria include older adults (aged ≥ 60 years) with a confirmed infection by SARS-CoV-2 by RT-PCR. Exclusion criteria include patients with a missing outcome and those discharged against medical advice.
Checking of medical files was done to extract demographic and clinical data including age, sex, reported symptoms of COVID-19 and medical history of chronic diseases. Charlson comorbidity index (CCI) was used to assess the burden of comorbidities [8]. A review of the reported COVID-19 symptoms was done including dyspnea, fever, fatigue, altered mental status, gastrointestinal symptoms, also the onset of these symptoms in days before admission and the received medications during hospitalization were recorded. Altered mental status was defined as the presence of any of the following: confusion, depressed level of consciousness and altered behaviour/agitation.
Checking for laboratory results on admission includes serum CRP, ferritin, D-dimer, albumin, aspartate transaminase, alanine transaminase, total bilirubin, BUN, creatinine, sodium, haemoglobin, white blood cells and platelets. Neutrophil lymphocyte ratio (NLR) was calculated by dividing neutrophil by lymphocyte count [9].
The outcome was determined by checking the clinical status of each participant either discharged alive from hospital or dead at the hospital, accordingly patients were divided into survivors and deceased group.
Values were presented as means ± SD or as numbers and proportions, as appropriate. The relations between qualitative variables were evaluated by Chi-square test or Fisher's exact test, as indicated. Continuous variables were checked for normality by using Shapiro-Wilk test. As data were normally distributed, Unpaired t-test was used. Based on sample size, 7 variables with P values ≤ 0.05 in bivariate analysis were selected and introduced in a forward stepwise logistic regression model to detect independent predictors of mortality. ROC curve was used to assess the sensitivity, specificity and area under the curve of the model, CRP and BUN. All tests were bilateral and a P value of 5% was the limit of statistical significance. Analysis was performed by statistical package software IBM- SPSS version 21.
The study protocol was revised and approved by the Geriatrics hospital ethics review board and Research Ethics Committee of the faculty of Medicine at Ain Shams University, Approval code: FMASU R 108/2021. It conforms to the provisions of the Declaration of Helsinki and preserves participants' confidentiality. Giving the retrospective design of the study, written informed consents were waived.
A total of 138 Geriatric patients infected with SARS-CoV-2. In-hospital mortality occurred in 54.3%. The mean age of participants was 71.17 ± 7.98 years. Baseline characteristics of participants are described in Table 1 and Table 2.
Table 1: Association between in-hospital mortality and quantitative variables. View Table 1
Table 2: Association between in-hospital mortality and qualitative variables. View Table 2
Based on the bivariate analysis, the laboratory variables significantly associated with in-hospital mortality were serum creatinine, BUN, albumin, LDH and CRP besides TLC and Hemoglobin level. Significant comorbidities were hypertension and chronic kidney disease (CKD) besides the total number of comorbidities and CCI. Symptoms significantly associated with in-hospital mortality were fever, fatigue and altered mental status.
Based on sample size and clinical significance, the following variables were selected to enter into multivariate regression analysis: Serum creatinine, BUN, albumin, LDH, CRP, CCI, and altered mental status. Independent predictors of mortality were serum BUN (OR 1.080; 95% CI: 1.028-1.134; P 0.002) and CRP (OR 1.012; 95% CI: 1.003-1.021; P 0.010) (Table 3).
Table 3: Logistic regression analysis of risk factors for in-hospital mortality in older adults with COVID-19. View Table 3
These results showed that with each 1 mg/L increase in CRP, the odds of mortality would increase by 0.012 times. With each 1 mg/dL increase in BUN, the odds of mortality would increase by 0.08 times. The 95% CI means that by 95% we are confident that with each 1 mg/L increase in CRP, the odds of mortality would increase from 0.003 to 0.021 times. While 1 mg/dL increase in BUN would increase the mortality odds from 0.028 to 0.134 times.
A ROC curve was plotted for the two predictors of mortality. The AUC of serum CRP and BUN were 0.735 (95%CI: 0.636-0.834; P 0.000), and 0.819 (95%CI: 0.741-0.898; P 0.000), respectively. Using a cutoff value of 90.750 mg/L, CRP predicted in-hospital mortality with a sensitivity of 71.4% and a specificity of 68.6%. Using a cutoff value of 32.500 mg/dl, BUN predicted in-hospital mortality with a sensitivity of 77.4% and a specificity of 75.0% (Figure 1A and Figure 1B).
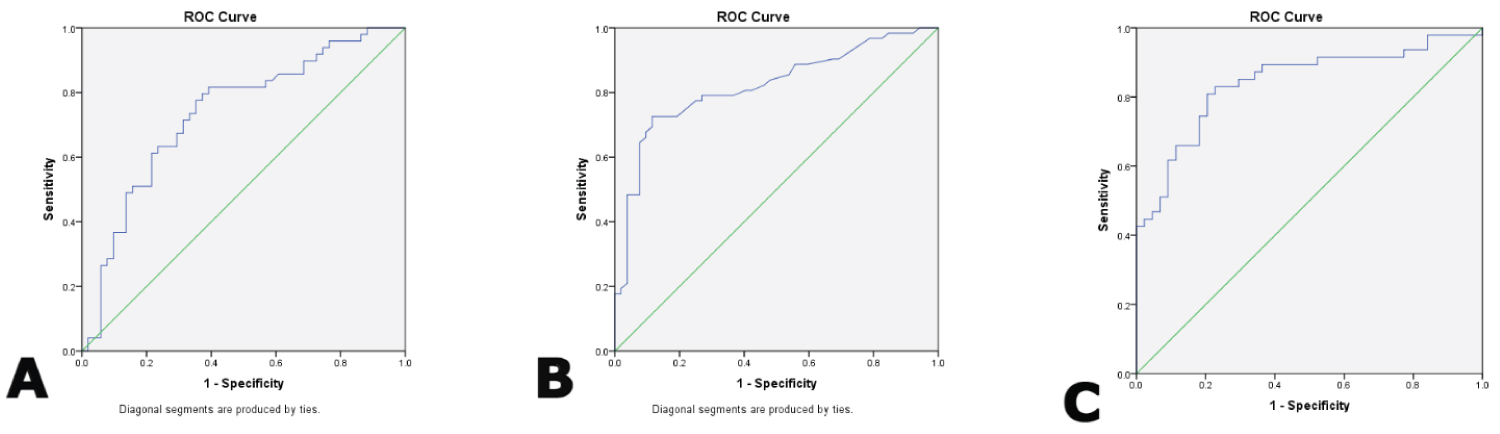 Figure 1: Receiver operating characteristic curve of the significant predictors and the predictive model for In-hospital mortality in older adults with COVID-19 A) Area Under the Curve of serum CRP is 0.735; 95% Confidence Interval: 0.636-0.834; P 0.000; B) Area Under the Curve of serum BUN is 0.819; 95% Confidence Interval: 0.741-0.898; P 0.000; C) Area Under the Curve of the predictive model is 0.842; 95% Confidence Interval is 0.758-0.925; P value 0.000. View Figure 1
Figure 1: Receiver operating characteristic curve of the significant predictors and the predictive model for In-hospital mortality in older adults with COVID-19 A) Area Under the Curve of serum CRP is 0.735; 95% Confidence Interval: 0.636-0.834; P 0.000; B) Area Under the Curve of serum BUN is 0.819; 95% Confidence Interval: 0.741-0.898; P 0.000; C) Area Under the Curve of the predictive model is 0.842; 95% Confidence Interval is 0.758-0.925; P value 0.000. View Figure 1
A predictive model was constructed; it was able to correctly predict mortality by 85% and was able to explain 58% of the variability of mortality as indicated by Nagelkerke R Square value. At a cutoff score of 0.469, this model predicted in-hospital mortality with a sensitivity of 80.9% and a specificity of 79.5%, with an area under the ROC curve of 0.842 (95% CI: 0.758-0.925; P 0.000) (Figure 1C).
The mortality rate within hospitalized older patients with COVID-19 was 54.3%. Serum CRP and BUN levels on admission were predictors of in-hospital mortality. A combination of these 2 laboratory markers was done to formulate a predictive model with an AUC of 0.842 with a good discriminative ability for predicting in-hospital mortality in older patients. The current study highlights the need for early prediction of in-hospital mortality among these vulnerable patients with the provision of a predictive model.
The reported high mortality rate is consistent with various studies involving older adults [5, 10]. It could be attributed to the poor immune response in older adults, making them more vulnerable to acute respiratory distress syndrome and respiratory failure [11].
The association between in-hospital mortality and the other variables was assessed by logistic regression analysis. Chronological age was not a significant risk factor for mortality as frailty, functional status and comorbidity have a significant prognostic role in older adults. This finding is supported by another retrospective study involving hospitalized Geriatric patients with COVID-19 [6]. Also, gender was not found to be a predictor of mortality, coinciding with other retrospective cohort study of hospitalized older adults [5]. These results are contradicting the reported higher mortality rates in males in another study [6].
The burden of comorbidities was assessed by CCI and it was significantly associated with mortality, coinciding with another study showing comorbidities as a significant risk factor for death [5]. The history of CKD was significantly associated with mortality. It is consistent with previous studies reporting the significance of CKD in mortality prediction among the aged [5,12]. Whether mortality is associated with hypertension in older patients remains uncertain as there are contradicting results about this association [12]. In this study, hypertension was significantly associated with mortality.
This study investigated the prognostic value of certain COVID-19 related symptoms among older patients at the time of admission. Dyspnea was the most prevalent reported symptom among participants (69.7%), followed by fever (62.8%), and cough (57.4%). The presence of altered mental status and fatigue were significantly associated with mortality coinciding with another retrospective cohort study including Geriatric patients hospitalized for a diagnosis of COVID-19 [6]. Our study showed that only 13.2% of patients presented with altered mental status survived to discharge from the hospital. This highlights the prognostic value of delirium and the significance of screening of Geriatric patients for its presence on admission. Delirium correlates with disease severity and could predict in-hospital mortality [6,13]. Also, the study showed that 69.7% of patients reporting fever in the clinical history were in the non-survivors group. It supports the results of a multi-center study reporting the presence of fever during hospitalization as a risk factor of poor outcomes including severe pneumonia and mortality in older adults with COVID-19 [14].
Regarding laboratory markers on admission, our results showed that non-survivors had statistically significant lower serum albumin than in survivors 2.90 ± 0.60 versus 3.34 ± 0.43 (P 0.000). It supports the prognostic value of serum albumin among older patients with and without COVID-19 [5,15]. Also, non-survivors had statistically significant lower haemoglobin 10.41 ± 2.29 versus 12.13 ± 2.25 (P 0.000), a finding supported by a previous prospective study showing the significant association between anaemia and mortality in hospitalized patients with COVID-19 [7]. It enhances the practical value to monitor haemoglobin levels during admission [7] as there is a causative association between COVID-19 and inflammation-induced iron dyshomeostasis [16].
Study results showed that non-survivors had statistically significantly higher serum BUN than in survivors as previously reported among older adults [5]. In this study, serum BUN level on admission was a predictor of in-hospital mortality where AUC was 0.819 (95% CI: 0.741-0.898, P 0.000). At a cutoff value of 32.500 mg/dL, serum BUN predicted in-hospital mortality with a sensitivity of 77.4% and a specificity of 75.0%. These data coincide with the results of another retrospective study in China where AUC was 0.769, the optimal Cutoff was 6.1 Mmol/L (110 mg/dl) with a sensitivity of 66.0% and specificity of 82.0% [5]. Besides the significantly higher BUN among the deceased group, serum creatinine levels on admission were also significantly associated with mortality. It could be related to COVID-19 induced acute kidney injury as SARS-CoV-2 has a cytopathic effect on proximal straight tubule cells and podocytes [17].
The study estimated the prognostic value of various inflammatory markers representing the risk of cytokine storm on admission. First, higher serum CRP levels were significantly associated with mortality in bivariate analysis. Serum CRP has been remained as an independent predictor of in-hospital mortality in the multivariate regression model with an AUC of 0.735 (95%CI: 0.636-0.834, P 0.000). In this study, a cutoff value of 90.750 mg/L was suggested with a sensitivity of 71.4% and a specificity of 68.6%. These findings support the reported prognostic role of CRP in another retrospective study including 210 hospitalized Geriatric patients with COVID-19 where AUC was 0.857, the optimal cutoff value was 63 mg/L with a sensitivity of 74.0% and specificity of 85.0% [5]. Second, the concentration of serum LDH level on admission was significantly higher in the non-survivors group than those in the survivors' group coinciding with a previous analysis [5]. Third, the study did not demonstrate the significance of NLR despite the reported significance between increased NLR and mortality among hospitalized older adults with COVID-19 [5]. This finding could be related to the small sample size for this variable in the study and it needs further assessment. Fourth, the study didn't reveal a significant association between D-dimer and ferritin levels with in-hospital mortality. It is inconsistent with another study demonstrating their significant prognostic roles in COVID-19 [18]. Qeadan et al. provided optimal cutoffs including 714 ng/mL (ferritin) and 2.1 mg/L (D-dimer) with AUCs ≥ 0.99 for in-hospital mortality [18].
Major Strengths of this study are the inclusion of Geriatric patients and investigating important risk factors with the provision of an age-specific, predictive model including two easily obtainable laboratory markers on admission. Also the study provided a suggested cutoff value of each predictor separately. However, this study has some limitations: First, it is a retrospective study in a single institute with the inclusion of a relatively small sample size especially for some variables such as NLR. Second, the reported clinical data including COVID-19 symptoms and medications were based on clinical histories obtained from different physicians and could be affected by the deficient documentation system and recall bias of participants. Third, patients with don't resuscitate orders couldn't be identified. Finally, the study lacks a validation sample.
Serum CRP and BUN on admission are predictors of in-hospital mortality in older adults with COVID-19. Alterations of these parameters during hospitalization must be considered. The combination of these two predictors formulates a predictive model with good discriminative abilities. It should not replace guidelines of management and needs to be elucidated in other prospective multicenter studies.
Authors thank physicians and workers in the administrative data section at Geriatrics hospital for their assistance in data collection.
All authors have made substantial contributions to the study through data collection and analysis. Khalid E. Elsorady has also contributed to the conception of the study and final manuscript write up besides coordinating investigators' roles.
The authors declare no conflicts of interest for this article.
None.