The primary objective was to explore falls risk associated with hearing impairment (HI), vision impairment (VI), and hearing aid use among older adults.
Participants (4,414) were categorized into six groups: no HI or VI, aided and unaided dual sensory impairment (DSI), aided and unaided HI only, and VI only. Falls risk included falling, being unsteady, and worried about falling.
Individuals with DSI had the highest falls risk, generally followed by VI only and then HI only. The use of hearing aids changed only one interpretation: Only those with aided HI were at increased risk for having fallen or nearly fallen in the last six months.
Those with DSI generally had the highest falls risk, followed by VI only and then HI only. Hearing aids did not appreciably alter the associations between falls risk and combinations of hearing impairment and vision impairment.
Hearing impairment, Vision impairment, Hearing aids, Falls, Older adults
ED: Emergency Department; VI: Vision Impairment; HI: Hearing Impairment; DSI: Dual Sensory Impairment; NHANES: National Health and Nutrition Examination Survey; CDC: Centers for Disease Control and Prevention; STEADI: Stopping Elderly Accidents, Deaths, & Injuries; HCC: Hierarchical Condition Category; EBM: Evidence-Based Medicine; COPD: Chronic Obstructive Pulmonary Disease; CHF: Congestive Heart Failure; CAD: Coronary Artery Disease; CKD: Chronic Kidney Disease; OR: Adjusted Odds Ratio; CI: Confidence Interval
In the United States, falls are the leading cause of injury among older adults, with about 25% falling per year [1]. These falls lead to 3 million emergency department (ED) visits and over 800,000 hospitalizations each year [2]. Financially, total medical costs associated with falling totaled more than $50 billion in 2015 [3]. Unfortunately, those age 65 and older who have fallen often become more fearful of falling and tend to become less physically active, leading to decreased physical fitness, which subsequently is associated with an increased risk of falling [4].
Vision impairment (VI), hearing impairment (HI), and both combined (i.e., dual sensory impairment (DSI)) have been associated with falling, although the evidence is inconsistent. Recently, a nationally representative study of over 11,000 older U.S. adults found a 70% increase in adjusted odds for falling among those with self-reported VI [5]. A meta-analysis of falls studies among older adults reported that those with HI were roughly 70% more likely to fall [6]. Using prospective data from over 3,000 adults age 70-79 years, those with moderate or greater HI had more than double the rate of falls; hearing aid use did not alter these findings [7]. Elsewhere, a five-year longitudinal study including roughly 1,500 Australians age 55 and older observed a two-fold increased risk of incident falls among those with severe hearing handicap [8]. In this study, DSI was not associated with falling after adjusting for cognitive impairment, and those with hearing aid use had a 75% increased risk for an incident fall. Separate studies using the Finnish Twin Study on Aging [9] found no association between HI and falls after adjusting for postural stability [10], while another study that used those with good vision as the reference category found that individuals with DSI were over four times more likely to fall in the following year; those with VI only had no increased falls risk [11]. Thus the evidence for an association between falls and HI, VI, and DSI is inconsistent, possibly due to differences in ways of assessing and/or categorizing vision, hearing, and falls, but remains worthy of further research.
It is also noteworthy that these referenced studies, incorporating hearing aids into the analyses, found no decreased risk of falls with their use. In fact, one study [8] reported an increased risk of falling with hearing aid use. Meanwhile, at least three studies have examined the association between hearing aid use and balance with mixed results. Two studies suggest a reduced risk of falls among hearing aid users through improved balance [12,13] while another found no improvement in balance [14].
The purpose of this study was three-fold. The first was to identify personal, health, and psychosocial characteristics associated with having DSI, HI only, or VI only. The second was to explore how DSI, HI only, or VI only was associated with falls risk, and the third was to determine how hearing aid use influenced any falls risk associations observed.
This study included individuals covered under an AARP® Medicare Supplement plan insured by United Healthcare Insurance Company (for New York certificate holders, United Healthcare Insurance Company of New York). These plans are offered in all 50 states, Washington DC, and various U.S. territories. Among all plan holders, 16,000 were randomly chosen to complete a mailed survey, of which 4,696 (29%) responded. The survey was conducted in May 2018, and excluded a priori those who were less than 65 years of age and did not have a minimum of 12 months of continuous plan coverage prior to the invitation. Survey respondents were excluded for incomplete information for the falls, VI, or HI questions, or for answering that they did not having hearing difficulty or hearing limitation despite reporting hearing aid use.
The survey included 53 questions about hearing impairment, hearing aid use, falls, vision, psychosocial outcomes (i.e., loneliness, resilience, social network index, optimism), health literacy, financial stress, functional status, and sleep, among others.
The hearing difficulty question asked: "Would you say that you have any difficulty hearing?" [15]. The second hearing question asked "Do you feel that any difficulty with your hearing limits or hampers your personal or social life?" [16]. Both had possible responses of "Yes", "Sometimes", or "No". Meanwhile, the hearing aid use question was taken from the National Health and Nutrition Examination Survey (NHANES), asking: "In the past 12 months, have you worn a hearing aid at least 5 hours a week?" with possible responses of "Yes" or "No". For this study, those who answered "Yes" or "Sometimes" to either the hearing difficulty or hearing limitation question were coded as having HI. Vision impairment was gathered using a single question from the Wisconsin Department of Health Services Functional Vision Screener: "Do you ever feel that problems with your vision make it difficult for you to do the things you would like to do?". Based upon responses to the HI and VI questions, categories for DSI, HI only, VI only, and neither were established. The DSI and HI categories were further divided into aided and unaided depending upon the participant's response to the hearing aid use question.
A "falls risk" variable was created for a positive response to any of the four falls questions included in the questionnaire (fallen or nearly fallen in the last six months, fallen in the last year, worried about falling, or being unsteady). The questions about having fallen in the last year, worried about falling, and being unsteady originated from the Centers for Disease Control and Prevention (CDC) Stopping Elderly Accidents, Deaths, & Injuries (STEADI) program, with a "Yes" response to any of the three questions indicating an increased risk for falls [17]. For this study, having fallen or nearly fallen in the last six months was also used to indicate an increased falls risk.
Demographic variables included age and gender. For race/ethnicity and income, zip code-level correlates were assigned based on the zip code of residence. Using data from the 2010 U.S. Census, we coded for the percentage of minority individuals living in each zip code [18]. A binary indicator was created based on this ratio to account for the impact of living in low (below 15%) or medium-high (> 15%) minority areas. Similarly, an income variable was created to denote low, medium, and high income levels based on whether the median household income in the individual's zip code was among the bottom 30%, middle 40%, or highest 30% of all U.S. zip code ranks.
Health status was additionally characterized using several variables from administrative databases, including the Hierarchical Condition Category (HCC) score, which is obtained from a standard risk adjustment tool that includes age, gender, and medical conditions [19]. The average Medicare insured has an HCC score of 1.0. Meanwhile, scores less than 1.0 predict future healthcare costs to be lower than average, suggesting better health, while scores greater than 1.0 predict future healthcare costs to be higher than average, suggesting poorer health. Variables were created for several disease conditions in the medical claims database. Optum™ Symmetry® EBM Connect® grouper software [20], incorporating principles of evidence-based medicine (EBM) [21], was used to identify individuals with asthma, chronic obstructive pulmonary disease (COPD), depression, diabetes, congestive heart failure (CHF), coronary artery disease (CAD), atrial fibrillation, hypertension, hyperlipidemia, osteoporosis, being overweight or obese, or having chronic kidney disease (CKD).
Although survey respondents were more likely to live in a metropolitan area and less likely to have been hospitalized in the past six months compared with non-respondents, these differences were not sufficient to warrant statistical adjustment for survey non-response bias. Based upon this decision, descriptive analyses were performed for unweighted DSI, HI only, VI only, and neither. In preparation for further regression analyses, variables with correlation or collinearity issues were identified and resolved. A multinomial logistic regression model was then performed to describe characteristics associated with DSI, HI only, and VI only using the neither category as the reference group. To explore the correlations between DSI, HI only, and VI only with falls, five logistic regression models were conducted using the five falls variables as the binary outcome and with DSI, HI only, and VI only as the primary explanatory variable, also adjusting for a number of the variables previously mentioned. Variables included age, gender, first-dollar coverage Medicare supplement plan, HCC score, population density, region, zip-coded income, zip-coded minority status, dementia, CHF, atrial fibrillation, diabetes, asthma, hypertension, CAD, COPD, hyperlipidemia, depression, osteoporosis, CKD, obesity, functional status, financial stress, loneliness, optimism, social network, resilience, sleep quality, and limited health literacy.
The study included 4,414 individuals who completed the survey and met inclusion criteria. Forty-one percent were categorized with HI only, 31% neither, 19% DSI, and 9% VI only. Among those with HI and DSI, 31% and 29%, respectively, used hearing aids. With respect to the falls questions, 56% answered "Yes" to at least one, and 14% answered "Yes" to all four. Other combinations of responses for having fallen in the last year, being unsteady or worried about falling are shown in Figure 1.
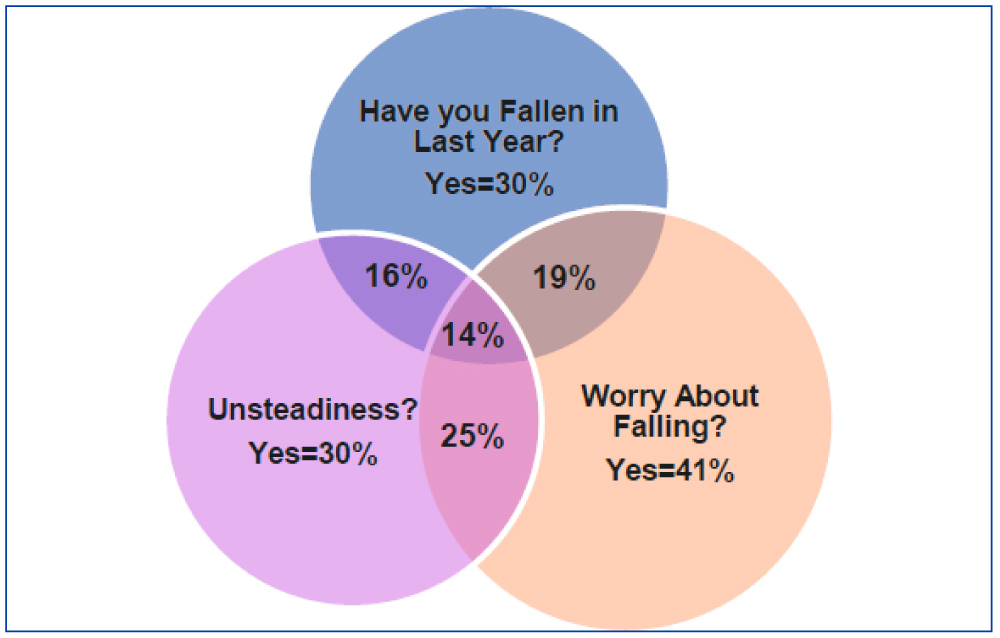 Figure 1: CT - angiography, CT - perfusion and cerebral angiography before endovascular treatment. A) CT - angiogram showing AVM and aneurism localization; B) CT - prefusion showing hyperperfusion zone in AVM and high-flow drainage vein; C) Cerebral angiography showing AVM of the right fronto-parietal region and the proximal flow - related aneurysm on the right terminal ACA afferent.
View Figure 1
Figure 1: CT - angiography, CT - perfusion and cerebral angiography before endovascular treatment. A) CT - angiogram showing AVM and aneurism localization; B) CT - prefusion showing hyperperfusion zone in AVM and high-flow drainage vein; C) Cerebral angiography showing AVM of the right fronto-parietal region and the proximal flow - related aneurysm on the right terminal ACA afferent.
View Figure 1
Descriptively, many differences were observed between those with DSI, HI only, VI only, or neither (Table 1). However, fewer of these associations remained statistically significant in the multinomial logistic regression model that utilized HI, VI, and DSI categories as the dependent variable (with the neither category as the reference), and most of the variables listed in (Table 1) as the independent variables (Table 2). Dual sensory impairment, HI only, and VI only were positively associated with high loneliness and increased falls risk. Increasing age, living in rural areas, and being overweight or obese were positively associated with DSI and HI only, but not VI only. Conversely, women and those living in the Northeast were associated with lower odds for DSI or HI only. Moderate loneliness and limited health literacy were positively associated with DSI and VI only; while good sleep was negatively associated with DSI (adjusted odds ratio (OR) = 0.74, 95% confidence interval (CI) = [0.56, 0.98]) and VI only (OR = 0.71, 95% CI = [0.51, 0.98]). Other associations observed for DSI included that individuals living in suburban areas, who had severely limited functional status or financial stress, were more likely to have DSI. Finally, HI was negatively associated with osteoporosis (OR = 0.74, 95% CI = [0.56, 0.97]).
Table 1: Unweighted Descriptive Comparisons by Hearing and Vision Impairment Status. View Table 1
Table 2: Adjusted Characteristics of Those with Dual Sensory Impairment, Hearing Impairment Only, and Vision Impairment Only. View Table 2
In this study, many instances of positive and statistically significant associations were observed between aided or unaided DSI, aided or unaided HI only, and VI only with falls risk. Individuals with aided or unaided DSI, aided or unaided HI only, and VI only were at increased odds of falling compared to those with no HI or VI (Table 3). More specifically, all five sensory impairment conditions were at increased odds for reporting unsteadiness or being worried about falling, with those who had aided and unaided DSI reporting the highest odds for both, followed by VI only, and then aided and unaided HI only. Only those with aided or unaided DSI or aided HI were more likely to have fallen or nearly fallen in the last six months, while only those with aided or unaided DSI were more likely to have fallen in the last year. Lastly, hearing aid use changed the interpretation in only one instance, in which individuals with aided HI were 48% more likely to have fallen in the last six months (OR = 1.48, 95% CI = [1.12, 1.96]), while there was no association for those with unaided HI (OR = 1.25, 95% CI = [0.99, 1.58]).
Table 3: Adjusted Odds Ratios for Falls Risk Variables Based Upon Hearing, Vision, and Hearing Aid Use Status. View Table 3
This study is one of a few studies to explore the association between falls risk and sensory impairment using a population-based survey of adults age 65 and older, also incorporating hearing aid use. Sixty percent of study participants reported HI, consistent with national estimates [22]. Meanwhile, our estimate of 28% with VI is higher than estimates published by the National Eye Institute of 1.5% for those age 65-69 to 26% for those age 80 and older [23], but aligns with the 25% observed using National Health Interview Survey data [24]. Among study participants, 30% had reported falling in the last year, which is about five percentage points higher than national estimates of 25% [1].
The first study objective was to describe personal, health, and psychosocial characteristics associated with DSI, HI only, and VI only. Individuals with DSI and HI only had similar personal characteristics, including a propensity to be older, men, living in rural areas or in the Northeast. Meanwhile, one of the personal characteristics shared between DSI and VI only was a positive association with limited health literacy. This most likely is a function of the health literacy question asking about how comfortable participants were filling out medical forms, which requires the ability to correctly read the forms. Meanwhile, only DSI was positively correlated with financial stress. Previously reported personal characteristics shared by those with HI and VI include that they are more likely to be older, male, with less education, and lower incomes [25,26]. We are uncertain why DSI and HI only were common among rural inhabitants, but a previous study reported that living in poverty, having lower education, and working as a manual laborer were all characteristics of rural environments, and positively correlated with HI [27]. This may also be the reason that living in the Northeast was associated with a decreased risk of DSI and HI, as this portion of the country has the highest population density [28] perhaps suggesting that the Northeast has higher wealth compared to other regions.
We also observed that individuals with several health and psychosocial characteristics were more likely to have DSI, HI or VI. For example, being overweight or obese was associated with DSI and HI, while poor sleep was associated with DSI and VI. Above normal weight has been previously associated with decreased hearing ability [29], and the association between vision impairment and poor sleep has also recently been described [30,31]. In contrast, having severely limited functional status was associated with DSI only, and those with osteoporosis were less likely to have only HI. At least one other study found a relationship between DSI and activity limitations [32]. Meanwhile, finding a lower risk of HI among those with osteoporosis likely reflects the strong association between this condition and older women [33] who are less likely to have HI. Finally, loneliness was associated with DSI, HI, and VI, which was also reported by a recent cross-sectional population-based study of over 21,241 Canadians between the ages of 45 and 89 years of age [34].
The second objective was to explore how DSI, HI only, or VI only were associated with falls risk. In this study, individuals with aided and unaided DSI were consistently at increased odds for falling, being unsteady, or worried about falling. These associations were always stronger than those observed for aided and unaided HI only or VI only. In addition, VI only was generally more strongly associated with those who were unsteady and worried about falling than those with aided and unaided HI only. The primary exception was that individuals with aided HI only were about 50% more likely to have fallen, or nearly fallen, in the last six months. However, no statistically significant association existed for those with unaided HI only and VI only. Our positive findings for DSI support those by Kulmala, et al. [11], who studied 428 women between 63-76 years of age, finding over a four-fold increased risk in one-year prospective falls for those with DSI compared to those with normal vision [11]. Kulmala, et al. also observed a 50% increased risk for incident falls among those with VI only, but it was not significant. Although a five-year prospective study of roughly 1,500 adults age 55 and older found that those with DSI were over twice as likely to have fallen two or more times, the association was not significant after removing those with cognitive impairment [8]. This study also found that those with self-perceived hearing handicap were about twice as likely to have fallen. In contrast to these studies, our study used several different falls risk criteria and utilized those age 65 and older. Another study of 1,662 NHANES participants between 40 and 85 years of age reported that HI was associated with over twice the risk for self-reported falling in the last year [35]. This study also reported that those with multiple sensory impairment, including HI, VI, and peripheral neuropathy, were over five times more likely to report falling in the last year. From a biologic plausibility perspective, it makes sense that those with DSI have the highest risk for falling compared to those with HI or VI only, as it has been previously demonstrated that both senses aid in balance [36,37]. Balance is known to be important for falls prevention, so decrements in both vision and hearing likely increase falls risk greater than having a decrement of vision or hearing alone. Our findings suggest that vision may be more important in determining falls risk than is hearing, but more research is needed to confirm this.
Finally, the third objective was to determine how hearing aid use influenced any falls risk associations observed. In this study, hearing aid use did not consistently lead to a decreased falls risk among hearing aid users compared to non-users, and there were four instances where hearing aid users had the higher falls risk. Finding an increased risk of falling among hearing aid users was also observed in a previously published prospective study [8]. As one explanation, research suggests that those most likely to use hearing aids are older and have more severe HI [38]. We also know that older individuals are also more likely to fall [1], so not finding a reduction in falls risk associated with hearing aid use may be due to some unmeasured differences correlated with age, even though we adjusted these models for age. Alternatively, it may be that a single question about hearing aid use does not sufficiently capture hearing aid effectiveness. For example, individuals who purchase over-the-counter hearing aids have less satisfaction with them compared to those who acquire them through an audiologist [39]. Perhaps the single question about hearing aid use, such as the one used in this study, should be replaced by a more thorough series of questions to better understand the relationship between hearing aid use and hearing aid effectiveness.
In this study, the survey data were cross-sectional in nature and did not provide evidence of the directionality of observed associations. As a result, we can make inferences about associations, but certainly not causality. Next, HI was self-reported, which may not accurately capture HI within the population [40]. However, 60% of our group reported HI, which is in alignment with current estimates of HI prevalence [22]. Falls were also self-reported and we do not know the causes of the falls. It is also worth mentioning that individuals do not wear their hearing aids and prescription glasses at all times, and it was not possible to determine if those who fell were using these devices when they fell. Meanwhile, study strengths included the relatively large random sample of 4,414 individuals age 65 and older. Another, strength was the inclusion of both VI, HI, and hearing aid use, as well as the adjustment for a number of potentially confounding variables derived from both self-report and medical claims.
Survey data from 4,414 adults age 65 and older were used to study the associations between falls risk with aided and unaided DSI, aided and unaided HI only, and VI only. Individuals with DSI had the highest falls risk, generally followed by VI only and then HI only. Hearing aid use did not appreciably alter the associations between falls risk and combinations of HI and VI. However, this finding should be interpreted with caution, given the likely limitations inherent in using a single question about hearing aid use. In summary, this study supports a positive association between having HI and/or VI and an increased risk for falling. However, it remains unclear how hearing aids impact these relationships.
We thank Stephanie J. MacLeod MS for her editorial assistance and critical review of this manuscript. Ms. MacLeod is also employed by UnitedHealth Group.
TSW, LDN, CSY developed the study proposal; TSW, LDN, JLK, GRB, conducted and interpreted the analyses; TSW, LDN, JLK, GRB, CSY wrote and reviewed the manuscript.
Timothy Wells, Jaycee Karl, Lorraine Nickels, and Gandhi Bhattariaare all employed by UnitedHealth Group and have stock with UnitedHealth Group. Charlotte Yeh is employed by AARP Services, Inc. However, their compensation was not dependent upon the results obtained in this research, and the investigators retained full independence in the conduct of this research.
This work was funded by the Medicare Supplement Health Insurance Program.
The conduct of this study has been approved by the New England Independent Review Board (NEIRB#: 16-093).