After 5 weeks of lock-down during the COVID-19 pandemic in Belgium, the government considered reopening schools in the beginning of May 2020. Decisions were merely made, based on advices from epidemiologists and virologists. This study shows that by using routine data in primary care decisions can easily be supported and infections can be monitored in a valid way. In this manuscript we made a descriptive analysis of the respiratory and COVID-19 related illness burden in children aged 0 up to 19-years-old. Based on routine data from out-of-hours primary care services, which are available on a daily basis, we found only small differences between the number of patient contacts for respiratory complaints in 2019 compared to 2020. The largest differences are seen in adults aged 25 years and older, with a 18% increase in respiratory diagnoses. Also, in small children an increase is found but limited to 8.3% in the age group between 12 and 19-years-old. Over time, during the 5 weeks period of measurements, we found a striking decrease in patient contacts for small children and younger adults in 2020 which is not seen in 2019. This might be a direct result of lock-down measurements.
We can conclude that routine data in primary care can be of great help in monitoring populations on a local level in the spreading of infectious diseases and enable decision makers to anticipate on new flare-ups on a daily basis.
As a response to the COVID-19 pandemic most countries have closed their schools impacting almost 70% of the world's student population and leading to a total of 1.2 billion of children not attending school [1]. European countries currently consider opening schools again. In Belgium, where a partial lock-down started on 13/3/2020, decisions are being made for a careful exit of lock-down measures starting with schools to reopen in May. Epidemiologists and policy makers base their decisions on the fact that children mostly have mild symptoms and their involvement in the spread of COVID-19 is probably limited [2-5]. Children have been at home, with limited contacts for about 6 weeks. An important question to consider is whether or not those children have had (suspected) COVID-19 during the lockdown period. Using the Out-of-Hours (OOH) research database of iCAREdata, we are able to measure and describe the Reasons for Encounter (RFE) with primary care OOH services and clinical diagnoses registered by the General Practitioner (GP) on call [6,7]. Obviously it is not possible to distinguish respiratory Covid symptoms from symptoms due to other respiratory infections; however, monitoring "respiratory illness" and comparing the current data with identical data from last year, can give an indication of the respiratory illness burden in children. These data are able to offer the evidence base for decision makers and monitor the disease after reopening of schools.
By comparing data of two similar periods in two consecutive years, differences in patient characteristics and primary care OOH services use were measured.
In Belgium OOH primary care is organized in General Practice Cooperatives (GPCs) which are available during weekends and bank holidays. These GPCs routinely register all patient contacts and send them daily to the iCAREdata database. This enables researchers to follow closely the evolution in several pathologies such as viral infectious diseases. The GPCs included in iCAREdata at this moment, cover a population of 2 million inhabitants (one fifth of the entire population of Belgium). iCARE data uses the pseudonymised Belgian national number as a unique identifier making it possible to link several consultations to one patient [7].
For this study we used data of 9 GPCs delivering reliable patient data over the period of 5 consecutive weekends, starting on 15/3/2019 and 5 weekends in the same period in 2020. To distinguish between 'respiratory' and 'non-respiratory' RFE or diagnoses, we separated data based on the International Classification of Primary Care 2 (ICPC-2) chapter 'R (respiratory)' or 'else'. For the definition of 'Covid-related RFE/diagnosis' or 'non-Covid related RFE/diagnosis' we defined Covid-related items as ICPC2 codes A77, R80, R27, based on underlying thesaurus terminology of respectively 'proven Covid-19 infection', 'suspected case of Covid-19 infection', 'recent contact with proven Covid-19 positive tested patient' and 'anxiety for Covid-19 infection'. As Covid-related RFEs or diagnoses were not relevant in 2019, we only analysed these data for the year 2020 as a descriptive analysis of frequencies in the different age-categories.
We divided the population in 'children' and 'adults'. For children we used the following age categories: Babies until kindergarten (0-5), primary school (6-12), high school (13-18).
This study was approved by the Ethics Committee of the Antwerp University Hospital (reference 13/34/330).
In 2019 the total number of contacts was 11811 by 11144 unique patients, with a mean age of 38.2 years (SD 27.8). In 2020 we counted 16917 contacts of 13726 unique patients, with a mean age of 42.6 years (SD 25.4).
In 2020 we see a factor 1.43 increase in the total of patient contacts, compared to 2019. Limiting the comparison to patients aged 18 years or younger shows a decrease with factor 0.90.
The mean number of contacts per patient indicates that patients have more contacts with OOH care in 2020 than in 2019 (1.03 contacts per patient in 2019 versus 1.23 in 2020). This is also the case in the younger age groups, although less pronounced. In the age groups of 18 years and younger, we find 1.03 contacts per patient in 2019 versus 1.21 in 2020. These findings illustrate the reorganization of primary care which took place in the OOH care setting as well as in regular care. Patients, during the COVID-19 pandemic are obliged to initially take telephone contact with the OOH service. Only patients with respiratory problems receive a first telephone consult with a general practitioner and possibly receive an appointment for physical examination if necessary. In normal circumstances, Belgian patients can seek immediate access to primary care during OOH, without any preceding contact by telephone or referral by a professional health care worker.
In Table 1 we show patient OOH contacts during 5 consecutive weekends in 2019 and 2020, the latter being in full lock-down period. The numbers indicate the differences in the proportions of 'respiratory-related' RFEs and diagnoses. We see an overall absolute as well as a relative increase of respiratory related contacts, more pronounced in the older patient categories. The highest percentage in 2020 was found in the age category between 18 and 26-years-old, which is also the case in 2019. The largest increase however is seen in the ages of 26 years and older. Concerning the respiratory diagnoses, the largest proportion of respiratory diseases in 2019 is found in the very small children up to and including the 5-years-old. In 2020 however, again, the largest increases are found in the age categories above 18-years-old, while staying quite stable for the younger ones.
Table 1: Proportions of contacts in ICPC2-chapter 'R' (respiratory) for different age categories in 2019 and 2020 (N = number of contacts). View Table 1
Looking at the course of the absolute number of patient contacts over both periods in 2019 and 2020 for the children aged up to and including 18 years in Figure 1, we find that in 2019 the figures are relatively stable during the whole period (fluctuating between 628 and 772 contacts per weekend). In 2020, the first weekend starts with a peak (964 contacts) and drops very fast towards 425 contacts in the 5th weekend. This finally results in a total number of patient contacts in this age group in 2020 ending up lower than in the same period in 2019 (resp. 3167 versus 3534). Although the reorganization of OOH care in 2020 results in more patient contacts per patient, due to the obligation to have a former telephone contact, the absolute number of patient contacts (including the telephone contacts) is lower.
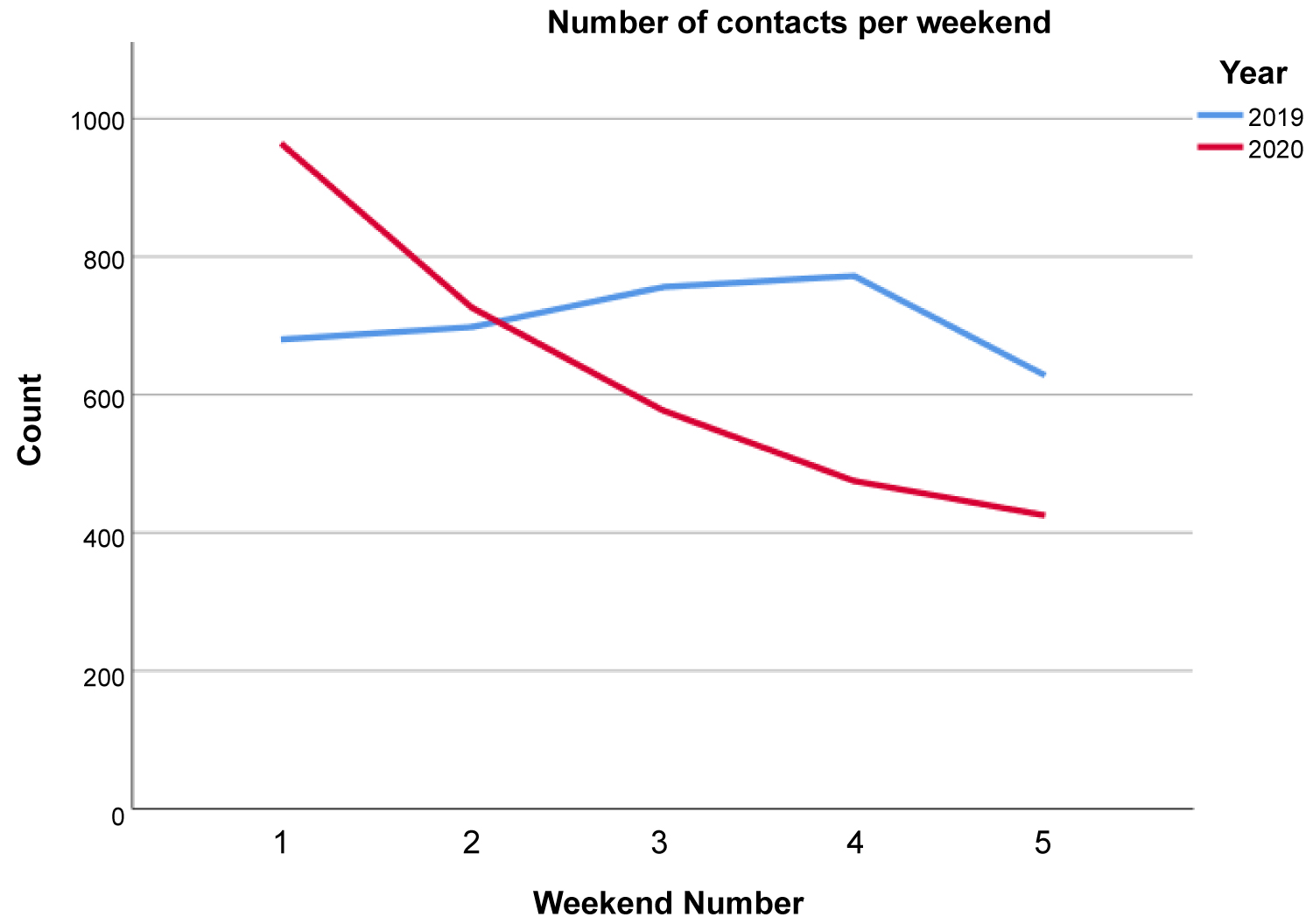 Figure 1: Evolution of the total number of patient contacts in the age category from 0 to 18-years-old, by calendar year.
View Figure 1
Figure 1: Evolution of the total number of patient contacts in the age category from 0 to 18-years-old, by calendar year.
View Figure 1
Table 2 and Table 3 illustrate the proportion of patient contacts based on COVID-19 related REFs or diagnosis in the different age-categories under study. This reveals that the majority of COVID-19 related contacts are found in the adults of 25 years and older. Kids of school-age up to 19-years-old, consult in 131 because of a COVID-19 related RFE in a total amount of 3167 contacts (4.1%). They receive COVID-19 related diagnoses in 515 contacts, representing 16.3% of all the contacts in these age-categories. For the population of 19-years-old and older we find percentages of RFEs and diagnoses related to COVID-19 respectively of 6% and 23%.
Table 2: Proportions of contacts with COVID-19 related Reason for Encounter (RFE) in 2020. View Table 2
Table 3: Proportions of contacts with COVID-19 related diagnosis in 2020. View Table 3
This study is the first to compare the impact of the COVID-19 pandemic on patient contacts during OOH care and the differences between age categories and RFEs and diagnosis. We used data of 5 consecutive weekends in March and April in 2019 and 2020, the latter being in the lock-down period in Belgium. During this period, which started on Friday March 13th, schools, shops, restaurants, and most businesses where closed. Children were not allowed to go to school. Patients were encouraged to call their GP before heading for an emergency department or GP-practice. Testing was only available for healthcare workers and hospitalised patients.
After six weeks of lock down, the government considered reopening the schools in a well-considered, phased procedure, assuming that kids were not at risk and have not been ill. Using the results of this study, we support this decision.
We used the number of patient contacts as a measure for the extra burden on OOH care, caused by the COVID-19 pandemic. Since in this epidemic telephone contacts are the standard and a number of telephone consults result in a physical consult afterwards, this may distort comparisons with 2019 [8,9]. However the structure of our database allowed us to identify unique patients as well as the number of contacts for each patient. We found out that in the age categories, subject to this study (ages up to and including 18-years-old), a decrease is found in the number of unique patients, contacting the OOH care (from 3425 in 2019 to 2619 in 2020), resulting in a similar decrease in patient contacts from 3534 in 2019 to 3167 in 2020. In the overall population seeking help at the GPC however, we find an increase in the number of unique patients (11469 in 2019 versus 13726 in 2020) and an increase in the number of patient contacts as well (11811 in 2019 versus 16917 in 2020).
For this reason, we conclude that patients aged between 0 and 19-years-old did not seek more medical care during COVID-19 pandemic than before. Considering the RFEs and diagnoses in this population, we see that children did not experience a large burden of respiratory diseases and in comparison with the year 2019 rather a small increase, where adults have had the largest number of respiratory and COVID-19 related consultations. We see similar results when looking at COVID-19 related RFEs and diagnosis.
Whether the absence of an increase in respiratory complaints is due to the lockdown measures or to a different transmission/infection/symptomatology in children, cannot be deduced from our data. The spread of all respiratory viruses has mostly likely been reduced by the lock-down [10].
However, lock-down measures seem to have a different influence in children and in adults. Furthermore, many factors may have an influence on whether people seek health care and advice besides the symptoms actually experienced. The threshold for seeking help may be lower or on the contrary higher in lockdown times. However, our data show 1) There is no increase in respiratory illness burden and 2) That there is a marked difference in consultation patterns between children and adults; the observed increase in adults is not at all seen in children.
During the study period, testing capacity for SARS-CoV-2 was very limited. Should there be a second peak in the same region, the recommendation to test all symptomatic patients will inevitably lead to a certain increase in consultations.
Several explanations can be found to explain the higher use of OOH care by adults. One of them being the fact that the COVID-19 pandemic certainly provoked concerns and therefore resulted in extra telephone contacts with health care services [8]. Another cause could be that the reason to contact medical care is to receive a certificate for sick leave, which is obliged in Belgium when staying at home from work because of illness. However, the odds ratio to receive a sick leave certificate in 2019, compared to 2020 was 1.249 (95% CI 1.175-1.328). Probably the fact that we only cover the OOH medical care context explains why the influence of this is rather limited.
Obviously, our observations must be interpreted with caution, however our data seem to offer one out of many arguments to support the idea to reopen schools. Furthermore, our database will allow to see almost in real time the possible effect of reopening schools on respiratory consults in children.
Although this study has its limits, it shows that there was no increase in respiratory illness burden in children during the lockdown period. Only 14% of the consultations related to COVID-19 during April 2020 outbreak in Belgium concerned minors. This is a careful argument to support the decision to reopen schools. Besides safely dealing with the COVID-19 related issues, also benefits are to be expected by reopening the schools, such as prevention of harm by learning disability, deprived social contacts, and leisure activities.