What we eat may cause Cardiovascular Disease (CVD), and a healthy diet is a key factor in the prevention of CVD. Promoting healthy diet is challenging, particularly for people with low Socioeconomic Status (SES), because poverty is linked with many risk behaviours such as smoking, unhealthy eating, and obesity. Multiple factors make healthy eating very challenging. Underpinned by critical realism, this study explores the factors that inform Pakistani people of low socio-economic status SES in making decisions on food choices after diagnosis with CVD.
The study was carried out at two Cardiac facilities of Karachi, Pakistan, in which 24 participants (male and female from different ethnic backgrounds), who had received health education, were selected to elicit the facilitators and barriers to healthy diet. The thematic analysis, using an interpretive descriptive approach, the study identified revealed seven major themes: (a) The meaning of food and healthy diet: A social dimension; (b) Poverty and a healthy diet: Not a matter of choice; simply to satisfy hunger; (c) Health promotion is a political issue: Survival is difficult because of political unrest in Karachi (c) Hope for recovery and family support: motivation for dietary change; (d) Family support and family relationships affect diet change (e) Self-control and self-determination; and (f) Culture and family values promote or hinder dietary change.
The cardiovascular risk and disease outcomes for the people of low SES are likely to further escalate if individual and structural barriers are not reduced, using multifactorial approaches.
Cardiovascular disease, Low socioeconomic status, Healthy diet, Economic and social issues in promoting dietary change, Cardiovascular disease in Pakistan
What we eat may cause Cardiovascular Disease (CVD), and a healthy diet is a key factor in the prevention of CVD. Dietary guidelines from the American Heart Association (AHA), European Society of Cardiology (ESC), and other sources are intended to reduce the burden of CVD, particularly in low- and middle-income countries [1-4]. However, direct adherence to these guidelines does not effectively promote healthy eating, particularly in people of Low Socioeconomic Status (SES). Poverty and low SES are considered the major determinants of adverse health outcomes throughout life [5-7]. Promoting healthy eating is challenging, particularly for people of low SES, which is linked with many individuals' values, beliefs, and attitudes and contextual factors such as the environment and health systems and structures. These interrelated factors explain why people of low SES have higher cardiac risk factors, higher rates of readmission, and higher case fatality rates [6,8].
Morbidity and mortality rates due to CVD are increasing in low- and middle-income countries. In recent decades, 30% of deaths worldwide have been due to CVD, and about 80%-86% of these deaths occur in low income and middle-income countries [9,10]. In particular, CVD mortality is rising in South Asian countries, which represent one fifth of the global population [11-13]. Mortality rates due to CVD exceeded 40% in 2008 [14], and the latest data from the WHO show that the age adjusted death rate due to CVD in Pakistan is 23%, 17th highest in the world [15].
Like many other low- and middle-income countries, Pakistan is also challenged to reduce poverty and close the social and economic gaps between the rich and poor. The country continues to face severe challenges with health inequalities, social disparities, and the ever-widening disparities between the rich and poor [16], which has major implications for the availability and sustainability of the resources required for the survival of the people of Pakistan. An investigation is necessary to comprehend the multiple factors that promote or impede healthy eating in Pakistani people of low income because CVD is closely associated with poverty. Therefore, the qualitative research study was conducted to understand the effects of various factors that inform Pakistani people of low SES in making decisions on food choices after diagnosis with CVD. The main research questions were as follows: (a) What are the factors that inform Pakistani people of low SES in making decisions on food choices after diagnosis with CVD? (b) What are the factors that promote or inhibit the consumption of healthy diets in people of low SES who have CVD?
This qualitative study was guided by the main tenets of Critical Realism (CR), which views individual behaviour as a result of the "complex interplay between individual and contextual factors; . . . [it] seeks to explain why people behave as they do” (p. 157) [7]. The theory helps researchers to understand the outcomes that occur in complex, multifaceted natural settings. CR also supports the use of qualitative, flexible, semistructured interviews to uncover the layers of complexity of the phenomenon and helps us to understand the broader social structures such as poverty, sex, race, and so on that exist in society and influence behaviour. People cannot deny the existence of these social realities just because they do not recognise or perceive them as factors that affect their behaviours or actively influence their lifestyle patterns (p. 3) [17].
Interpretive descriptive methodological approach was used for data collection and data analysis [18]. ID guides researchers through articulating patterns and themes from qualitative data related to various clinical phenomena [19, 20]. Participants were recruited from two cardiac facilities in Karachi, the largest metropolitan city of Pakistan. Many ethnolinguistic groups from all parts of Pakistan reside in Karachi. The inclusion criteria comprised participants who were 30-70 years of age and had a CVD diagnosis (self -reported), had attended any kind of CR programme or received teaching related to secondary prevention, earned CAD$1.25 (Rs113; self-reported) or less based on the poverty line defined by Pakistan's economic analysis, were of any ethnic group or religion, were able to speak English or Urdu (the national language of Pakistan), and were willing to be interviewed.
The study received ethical clearance from the ethical review committees of the University of Alberta, Canada, and the Aga Khan University, Karachi, Pakistan.
We recruited 28 eligible participants, 4 of whom withdrew from the study for personal reasons. We therefore interviewed 24 participants according to an interview schedule. We asked the participants about their knowledge of healthy diets, who decides to purchase food, how they make these decisions, how successful they are in changing their diets, and the difficulties that they face in selecting food. Each interview lasted from 60 to 90 minutes, and the participants determined the length of their interviews. As a token of thanks for their participation, we gave 250 (CAD$3) in cash at the end of each interview.
After completed the interviews, with the help of one of the bilingual research assistants hired for this study, the first author translated and transcribed the recordings To ensure accuracy of the translations and transcriptions, we rechecked the transcripts against the audiotapes and revised them where necessary and then printed a hard copy for the initial coding and identification of themes. The final analysis thus conveys the entire essence of the individual and contextual factors that influenced the participants' dietary decision making (see Table 1 for the step-by-step analysis process).
Table 1: Step-by-Step process of analysis. View Table 1
Twenty-four eligible participants consented to be interviewed, 2 refused to participate because of a city crisis, and 2 others refused for personal reasons. We entered the demographic data of all 24 participants into SPSS V 22 software to obtain a descriptive analysis. Table 2 (Demographic Information on the Study Participants) presents further demographic data on the participants. Pseudonyms were used in all presented data to maintain participant confidentiality.
Table 2: Demographic information on the study participants. View Table 2
The thematic analysis revealed a rich account of the profound meaning, influences, facilitators, and barriers associated with diet change as a result of their disease. Overall, their views on what helps or hinders changes in behaviour were mixed. The participants were greatly concerned about the disease and medication or surgery and wondered how they could further prevent a reoccurrence. They spoke about their limitations and the challenges of reducing the main dietary elements such as salt, spices, and fats. The factors that facilitated diet change include formal and informal support from family members or community resources. We further conceptualise these factors under six major themes that reflect the participants' difficulties and their motivation to change their eating behaviour. Figure 1 illustrates major structural and cultural factors that promote/impede dietary change from the participants' interview. The seven major themes from the Figure 1 are: (a) The meaning of food and healthy diet: A social dimension; (b) Poverty and a healthy diet: Not a matter of choice; simply to satisfy hunger; (c) Health promotion is a political issue: Survival is difficult because of political unrest in Karachi (d) Hope for recovery and family support: Motivation for dietary change; (e) Family support and family relationships affect diet change (f) Self-control and self-determination: Choosing between taste and health; and (g) Culture and family values promote or hinder dietary change. Pseudonyms are used for the participant quotations.
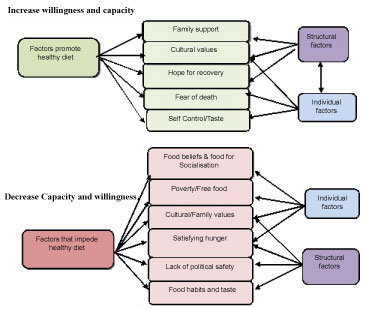 Figure 1: Structural and cultural factors that promote/impede change in low-income CVD patients. View Figure 1
Figure 1: Structural and cultural factors that promote/impede change in low-income CVD patients. View Figure 1
Food has an interesting relationship with humankind and our very diverse belief systems. It is a symbol of culture, religion, and moral and sentimental values. Throughout history food has been used to identify specific communal identities among all age groups. The participants do not simply relate food to their physical health or their disease, but connect it to their culture, attitudes, and beliefs. Their culture and tradition are explicitly expressed in their dietary habits. Under this theme we identified three primary aspects of CVD patients' lifestyle with regard to dietary changes: (i) The concept of perhezi diet, (ii) Food as a symbol of socialisation, and (iii) Food as a blessing from God, These areas are interrelated, and we discuss them separately to ensure clarity [7].
The term "perhezi diet" (patient's diet) is commonly used in many cultures of Pakistan. It refers to the particular diet of sick people-a restricted diet that people do not consider healthy. Most people do not consider it the type of diet that healthy people consume. Perhezi foods do not have a traditional taste; they usually have less oil, salt, and spices and are homemade. The female patients spoke more about perhezi food than about a prescribed diet or healthy food. Particularly those who were recently diagnosed as cardiac patients wanted to talk more about disease prevention. Kulsum, a 40-year-old lady, described the perhezi diet as simple and explained that "those who are suffering from a heart attack or any other heart illness must eat more simple food [perhezi diet], mostly boiled, without salt; avoid animal fats, fried foods, heavy foods, ghee (purified butter). It is difficult" (P7).
The participants consider food a strong symbol of socialisation. Therefore, diet changes and food choices have a great impact on social life. Several participants emphasized the significance of eating fried and spicy food as a social activity. They associate eating with family and getting together with friends as social entertainment and enjoyment and value the traditional taste and different kinds of food, which is more important to them than nutrition. Men are regularly challenged to maintain a balance between social life and healthy diet because it is customary for men in Pakistani culture to socialise with male members of their extended families or with friends and colleagues. Mr. Javed feels isolated and frustrated because diet restrictions have invaded his entire lifestyle. He finds socialising a challenge because social gatherings force him to eat whatever is served, and refusing to eat is considered an insult to the host:
Now I have minimized visiting relatives and adopted a simple lifestyle. I do not enjoy eating; I am prohibited from eating certain meals. I feel isolated and very weak. I do not attend parties and family gatherings any more because they force you to eat, and when you refuse, it looks rude and it is not respectful. To avoid the difficulty of consuming unsafe, harmful foods at parties and restaurants, I force myself to stay home. (P11)
Faith and religion play a central role in managing illness, and religious beliefs are strongly intertwined with eating and other lifestyle activities. Women who attend Madrassa are unable to receive a secular education linked food with religion (Islam). They consider all food a gift from God and believe that they should not categorize food as good or bad or healthy or unhealthy. The participants also perceive their religious obligation to be thankful for their circumstances or whatever troubles they face because disease and suffering are from God and are part of their fate. Thus, the meaning attached to food either facilitates healthy behaviour or acts as a barrier to positive dietary changes.
We asked the participants to describe the difficulties they face in changing their diet, and they lamented their vulnerability and helpless situation. One major problem that they highlighted was the lack of food, followed by the unavailability of desired food and insufficient purchasing power or buying capacity. Their main concern was filling their stomachs to reduce hunger rather than nutrition or choice; the reason is that they do not have sufficient time and money to prepare food for themselves because of their working hours. The participants with knowledge are willing to eat healthy foods; however, the lack of resources and individual capacity hinder changes. This presents real challenges to the healthcare system. Medical staff and healthcare workers unthinkingly prescribe healthy dietary changes but offer no means of doing so. Three sub themes emerge from the data are:
Several participants, particularly those living in large families with two or three wage earners, expressed their desire for free food. These desperate individuals, and often their children as well, attend funerals, where poor people are offered free food (lungar). They also visit religious places such as shrines, where pilgrims and believers are offered free meals. Describing his eating habits, a father of seven children illustrated his vulnerable situation: "I eat whatever is there in lungar [free food offered to the poor]". They work on shrines or religious places, work as guards or house cleaners, or perform religious duties for visitors; the visitors to the religious places usually bring the workers traditional food. As a solution, they choose oily foods rather than remaining hungry.
Even when a few participants struggle to change their dietary patterns to eat suitable homemade food, they all face different problems, such as the unavailability of fresh fruits, lack of a vehicle, and distance to food markets. Their accounts indicate a compendium of problems from the inability to purchase proper food and the additional cost of transportation to the lack of proximity to good food markets. Most of the participants use public transportation to get to work and cannot bear the additional cost of separate transportation to get to fruit and vegetable markets; therefore, they purchase stale food from nearby food outlets. Nearby food outlets have small moving carts for old leftover vegetables and fruits that they sell at cheaper rates. Distance and transportation are important factors; however, patients' willingness and age-related mobility also affect diet changes.
The fundamental issues that arose in the participants' discussions are related to managing the multiple day-to-day expenses that are a consequence of low SES. A considerable number of participants viewed their socioeconomic context, such as housing, unemployment, and major payments, as a more urgent concern than the purchase of healthy food. They described their difficulties in managing multiple expenses and the requirements of a healthy diet. Mrs Saeeda tries to manage all of the household expenses on her husband's limited income:
My buying capacity is very limited. I have to pay the expenses for the whole month: School fees, transportation, bills, and rent has increased by Rs2000. So I have Rs4000 left over to last another 20 days. I cannot pay for fresh vegetables and fruits and fish or chicken. One kilogram of fish is Rs450, and when I go shopping—usually I do the shopping; my husband gets tired-I have to keep the price range in mind. I go in the evening, and I buy only leftover, rotten things. I always buy open oil, not oil that is healthy. (P15)
Financial constraints greatly affect their decision making with regard to reducing the dietary risk factors and increased food prices based on the world market, which, in addition to the country's poor economy, has resulted in deprivation for the participants and their families. They plunge deeper into crisis with additional expenses such as a family member's sickness or urgent household repairs. During times of economic stress, they have been forced to take out loans and have huge debts that have pushed them into further financial deficit. The participants clearly expressed their guilt feelings, stress, and anxiety related to their disadvantageous economic situation and inability to comply with the requirements for healthy eating. These challenges not only impede their cardiovascular health, but also further deprive them of earning money. It is therefore crucial to break the vicious cycle of ill health and poverty for the people of Pakistan to reduce the burden of CVD and poverty.
Lack of safety and security at the study location also hindered their daily life activities, including food selection and choices. Almost all of the respondents loudly and clearly expressed their deep concerns about the existing political turmoil that influences curative and preventive measures. They lamented that, because the city is in a permanent state of chaos, how could they think of healthy eating and fresh foods when survival is so difficult? Banu, who was unable to attend her doctors' appointment because of her arthritis, discussed the heart-friendly food chart that cardiac patients receive during their first visit, commented:
Eating healthy and heart-friendly food has become a dream. Even being able to get enough food for survival has become questionable when life itself is not safe. In such a frenzied atmosphere, I do not know how we are able to keep on going. In Karachi, rich, poor, all are uncertain of their next breath, Madam. (P22).
Despite the challenges that the participants identified with regard to their inability to change their dietary patterns, a few have been moderately successful in doing so. They reported that certain factors motivate their lifestyle changes, such as the fear of death, hope for recovery, and family support, which they consider major forces in changing their behaviour. The participants were genuinely emotional about their struggle to change their eating habits. Some try to reduce the salt in their diet, use less oil, or boil vegetables; and others are involved in religious activities to reduce the stress. The participants have also been motivated to change their diet out of fear of being a burden on others or being left alone because of their disease. However, changing their diet is possible only to the extent that their purchasing does not exceed their earnings. Few younger participants were concerned about their illnesses, surprisingly not because of death, but because of responsibility: If they die, there will be no one to look after their children.
Another major motivation for the participants to eat the recommended diet is the support of family members, who not only advise and encourage them to eat a less oily, less spicy, and less salty diet, but also change the menu and the food that the family cooks. Customary family practice also determines the food to be consumed, and all family members eat the same food prepared in the house. Thus, many family members eat the food that was prescribed for the participants after their diagnosis of CVD. As a result, the participants eat a healthy diet, but they feel guilty that because of their illness other family members cannot enjoy traditional food.
The support that the participants receive from their families to make this change is encouraging, but it also has a strong negative impact on the family and the cultural norms, particularly when social connections do not understand the importance of dietary change for patients with CVD.
As the analysis progressed, we identified individual factors related to the difficulties in changes in diet. Some participants have shown a lack of willingness despite the favourable environment, whereas others have demonstrated that their willingness and determination have made dietary change possible. However, it is important to note that one cannot assume that individual factors alone can change behaviour. This theme includes the individual characteristics of the participants that influence dietary change, provided that other structural barriers are overcome. Those who do not have a problem accessing and affording food cited personal reasons related to the lack of willpower and determination. For them, the taste of food is more important than their health. The participants spoke of their inability to continue to eat a non traditional diet. They explained that simple food causes a lack of appetite, and they feel sick; it also increases their craving for unhealthy foods. Some personal shortcomings decrease the ability to change diet. People are attached to a traditional diet and cannot avoid unhealthy food. In the interviews they said that they have an "addiction to our food" or "cannot change" their habits: Mr. Mazhar expressed his challenge
Speaking truthfully, I tried but I cannot control sweet things. It seems that I cannot live without sweets. I am always craving them because I am addicted. I feel good if I eat sweets, because I used to eat these foods, but slowly I am controlling [my diet] [19].
The relationships between cultural and family values are a standalone important factor in behaviour change. We identified many aspects of culture that affect the participants' choice of food since their diagnosis of heart illness.
Cultural values can be major barriers to changing dietary habits because Pakistani food is known for its flavours and spices, and food in Pakistani culture is a factor in socialising and maintaining relationships. Because strong family bonding is evident in Pakistani culture, the members often sacrifice their health to maintain their role and identity in their family and society. If they do not follow their cultural and religious food traditions, they feel left out of society. Therefore, for the participant with strong family values opt for unhealthy food and give up the required dietary change.
This study presents some of the unique and pertinent factors that influence the consumption of healthy diets for low-income people with CVD. The findings highlight that the meaning of food is connected to cultural, family and religious values. However, the choice of food also highly depends on the availability of scarce resources. Despite the fact that people are aware of healthy and unhealthy food, the difficulty in following recommended dietary regimes results from various interrelated individual and contextual factors [7,21]. People find it difficult to resolve multiple other important life events and problems, such as safety and security and the need to fulfil other responsibilities such as paying rent with scarce resources, and food choice assumes lower priority. They eat food for the sake of satisfying their hunger.
A few studies of low-income groups have identified similar factors that hinder the individual capacity to make recommended changes in diet, such as limited purchasing capacity [9], limited accessibility of healthy food markets, inability to manage multiple financial commitments because of their limited income [7,22-24], and high prices for healthy food. This study and the findings of other studies conducted with low-income groups of people in Canada [9] and immigrants with chronic diseases in South Asia [25] suggest that , unless these issues are addressed, people of low SES will be unable to change their diets, despite their willingness [26-28].
The study data reflect a direct relationship between a peaceful political environment and the ability to buy fresh fruits, vegetables, and other required nutritional goods, as well as regular visits to the hospital. The participants reported that they have felt insecure and anxious and had experienced mental trauma for the last year because of the unstable political conditions and suicide bombings. One of the most important reasons for the failure of CVD preventive programmes is "placing the onus of risk factor reduction on individual responsibility and downplaying contextual factors" (p. 161) [7] such as the management of multiple household needs on a limited income, the persistently high prices of healthy food, and transportation issues. These programmes must also address the social and political situation at the regional and national levels.
Therefore, we make recommendations to reduce the prevalence of CVD at three levels. First, at the individual and family level, we recommend that healthcare providers set realistic goals for low-income patients and not focus solely on education with regard to the list of food items that are prescribed in the current guidelines. Second, we recommend that changes be made at the health-system and structural levels at which poor people receive healthcare; for example, the multifaceted Tawana Pakistan Project [26,29] was developed to address the poor nutritional status of primary-school-age girls in the low-income population. Finally, we recommend that health policies at both the national and the regional level be integrated into other systems such as finance, education, and the social and environmental structures [30,31]. This study demonstrates the most convincing evidence to better understand the challenges that poor people face in changing their eating behaviours, and these individual and contextual barriers should be included in the preventive guidelines.
Consuming a healthy diet is a complex human behaviour and is consequently influenced by many interrelating individual and contextual factors. The results of this study highlight the importance of understanding the factors that strengthen or hinder healthy eating habits. To date no substantial research is available that has fully explored the factors, gender dynamics, and issues related to the consumption of a healthy diet for people of low SES. This study can play a pivotal role in formulating recommendations for government and nongovernment organisations to prevent fragmented services; it might also call for major changes in health and agricultural policies and resource allocation as well as practical improvement in the environments of people of low income.
The authors would like to thank a panel of independent experts of International Development Research Centre (IRDC), Ottawa, Canada for peer-reviewing the protocol. Many thanks to all the participants who agreed to be interviewed and to the staff of the cardiac departments of both institutions for facilitating the process of recruitment and for providing appropriate space to conduct the participants' interviews.
This research received a prestigious IRDC (International Development Research Centre) doctoral award from International Development Research Centre, Ottawa, Canada and was extensively reviewed by a panel of independent experts in the field.
None.