Constipation is prevalent in the elderly. Rarely, severe constipation leads to stercoral colitis, a condition which results from fecal impaction in the colon causing increased intraluminal pressure, ulcer formation, and perforation of the colonic tissue. This condition can be fatal if it is not recognized early and promptly treated. Early detection is often difficult as this disease primarily affects elderly patients with history of dementia, stroke, or other neurologic disorders, and can cause altered mental status (AMS). Therefore, AMS in patients at risk for severe constipation should be substantial reasoning to consider stercoral colitis on the list of differentials.
Stercoral colitis, Severe constipation, Colonic perforation, Altered mental status
Constipation is a common gastrointestinal issue marked by slowed colonic transport especially prevalent in the elderly. Infection, dehydration, dietary/fluid intake, decreased levels of physical activity, medications such as opioids, nonsteroidal anti-inflammatories, and tricyclic antidepressants are some of the factors that contribute to constipation [1]. Common side effects of constipation include diverticulosis, hemorrhoids, and rectal fissures however rarely severe constipation can lead to stercoral colitis. It is a serious inflammatory condition which results when unresolved fecal impaction hardens into a fecaloma mass [2]. Fecalomas wedge in discrete areas of the colon causing increased intraluminal pressure, most commonly at the rectosigmoid site of colon as it is the region of the colon that is not only most narrow in diameter, but also where feces is most dehydrated [3]. High pressure on the colonic wall from stagnant fecal material leads to ulcer formation, focal pressure necrosis, and increased risk of bowel perforation [2]. When stercoral colitis is associated with colonic perforation, 35% mortality rate has been reported [4]. Despite high morbidity and mortality associated with this condition, stercoral colitis remains not well studied. Less than 200 cases of this condition have been documented since the first known case in 1894. Given our aging population, the incidence of stercoral colitis is likely to increase [1] therefore, early diagnosis and treatment is crucial to decrease overall morbidity and mortality [5]. Here, we present two cases of stercoral colitis in elderly with altered mental status successfully treated with fecal disimpaction and bowel regimen, thereby avoiding late-stage complications of the disease process.
Patient A: A 85-year-old female presented to the hospital with AMS and abdominal pain. Past medical history was significant for dementia and cerebrovascular accident (CVA). On admission, the patient's family was concerned regarding her acute change in mentation given her history of CVAs. Her vitals were significant for tachycardia to 103 beats per minutes. Her labs revealed leukocytosis of 23.4 thousand/mm3. Given AMS, Computed tomography (CT) head was obtained which revealed no evidence of acute intracerebral event. CT abdomen was also obtained given her abdominal pain which interestingly revealed a large stool ball within the rectum with surrounding inflammation suggesting stercoral colitis (Figure 1). Patient promptly underwent manual disimpaction with a large amount of fecal material removed and was continued on an aggressive bowel regimen to continue clearance of fecal material. Next morning, the patient's mentation returned to her baseline.
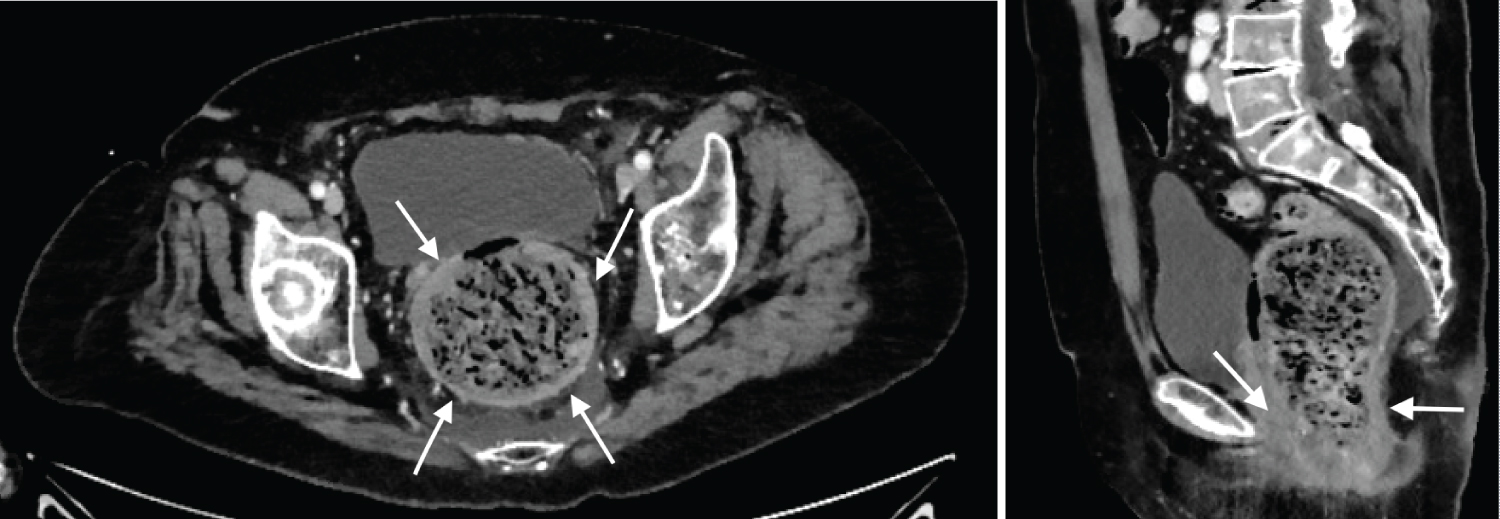 Figure 1: A cross-sectional and sagittal computed tomography image of the abdomen and pelvis showing circumferential wall thickening in patient A with a markedly distended, stool-filled rectosigmoid colon (arrows).
View Figure 1
Figure 1: A cross-sectional and sagittal computed tomography image of the abdomen and pelvis showing circumferential wall thickening in patient A with a markedly distended, stool-filled rectosigmoid colon (arrows).
View Figure 1
Patient B: A 73-year-old male presented from a nursing home for AMS. Patient's medical history was significant for severe Alzheimer's dementia and previous bariatric surgery. On presentation he was more altered than his baseline. Abdominal tenderness was noted on physical exam. His vitals and labs were within normal limits. CT head revealed no evidence of acute intracranial processes; however, the abdominal CT revealed a very large rectal stool ball with borderline thickened rectal wall, suggesting stercoral colitis (Figure 2). Manual fecal disimpaction was performed to remove the obstructing stool which released approximately 10 × 10 cm worth of fecal material. The patient was started on an aggressive bowel regimen to further ensure bowel clearance. The next morning, the patient's mentation returned to his baseline. On discharge, the patient was returned to the nursing home with follow up with his primary care physician.
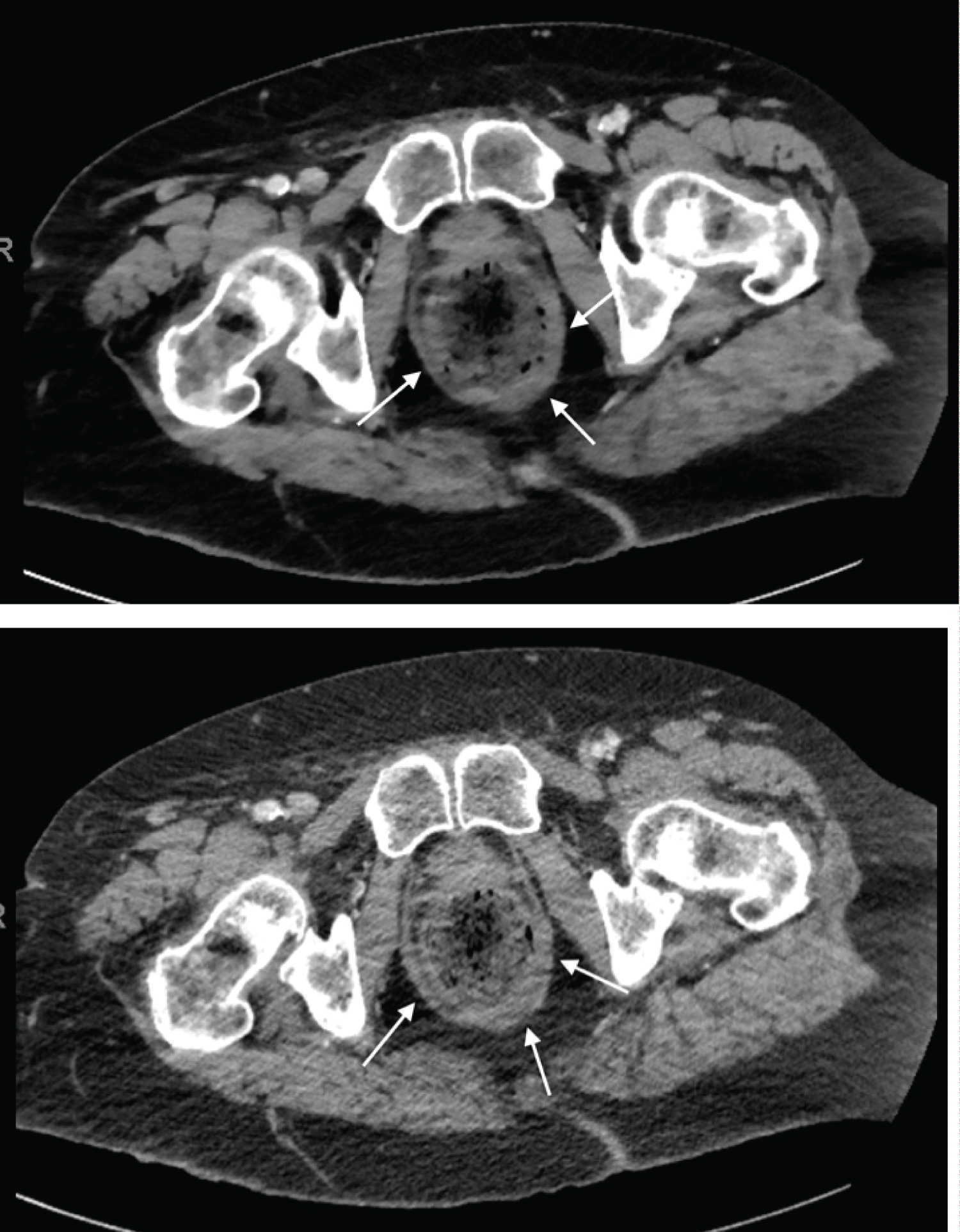 Figure 2: A cross-sectional image of the abdomen and pelvis showing circumferential wall thickening in our patient B with stool-filled rectum colon (arrows).
View Figure 2
Figure 2: A cross-sectional image of the abdomen and pelvis showing circumferential wall thickening in our patient B with stool-filled rectum colon (arrows).
View Figure 2
Stercoral colitis is a rare condition most often seen in elderly patients with history of stroke or dementia. This condition can be fatal if it is not recognized early and promptly treated, thus it is important to be cognizant of current barriers to early diagnosis that exist and address them accordingly. As this disease primarily affects elderly patients who have suffered from dementia, stroke, or other neurologic disorders, the history that is provided by the patient first hand may be limited, somewhat unreliable, or entirely unavailable secondary to altered mental status [2]. Therefore, in patient population most often affected by stercoral colitis, altered mental status serves as a cardinal clue. Acute mental status change is additionally a well-documented feature of infection in elderly patients, and in the context of stercoral colitis, should be considered a useful clinical marker [6]. Thus, in patients with risk factors of constipation, presenting with altered mental status, sterocoral colitis should be on the differential.
Symptoms associated with sterocoral colitis may be variable, but most complain of constipation and abdominal pain. Additional history might be limited given this disease primarily affects elderly patients who have suffered from dementia, stroke, or other neurologic disorders. Classic physical exam findings of sterocoral colitis may include diffuse abdominal tenderness, abdominal distention, and hard stool in the rectal vault on digital exam [2,7]. On CT, imaging often reveals a distended colon with associated mural thickening and the presence of significant fecal impaction. Other findings such as fat stranding, mesenteric hyperemia, and extraluminal gas can also be present in late-stage complications such as ulceration and bowel perforation [8].
Treatment includes prompt fecal disimpaction and aggressive bowel regimen to prevent late-stage complication [9]. Bowel regimen typically includes a combination of oral agents such as senna, docusate, MiraLAX, Dulcolax as well as rectal enemas. Manual disimpaction is extremely effective at decreasing intraluminal pressure within the colon and reducing the risk of ulceration secondary to high pressure placed on colonic walls by a fecaloma mass [5]. More than 50% of stercoral colitis patients can be managed with disimpaction and bowel regimen, whereas those with severe complications and concern for bowel perforation, and peritonitis may require prompt surgical treatment such as colectomy, hemicolectomy, or sigmoidectomy [5,8]. Prompt intervention is important to prevent perforation and further complications such as septic shock and multiorgan failure [2].
As demonstrated with the two cases discussed in this review, altered mental status in the setting of patients at risk for severe constipation should be substantial reasoning to consider stercoral colitis on the list of differentials. Altered mental status at baseline, secondary to prior stroke, dementia, or other neurologic cause, should be considered a risk factor for the development of stercoral colitis. Consideration of this diagnosis is crucial as early treatment, such as manual disimpaction and bowel regimen, can significantly improve clinical outcomes and prevent surgical intervention.
All authors have contributed equally to the case report.
The Authors declare that there is no conflict of interest.
All attempts have been exhausted in trying to contact the patient, next of kin, and/or parent/guardian for informed consent to publish their information, but consent could not be obtained.