Context: Bone marrow examination is an important diagnostic tool widely used in various haematological and non-haematological disorders. Bone marrow evaluation may either confirm clinically suspected disease or may provide the previously unsuspected diagnosis.
Objectives: To study the spectrum of lesions, comparison and evaluation of diagnostic efficacy of the bone marrow aspiration and bone marrow biopsy findings in various haematological and non-haematological disorders.
Design: A prospective study on 100 cases of bone marrow aspiration and biopsy was conducted between January 2019 to June 2020.
Results: A total number of 100 cases of bone marrow aspiration and biopsy were studied. Among the 100 cases studied, 92% were haematological disorders followed by 6% were non-haematological disorders and 2% were normal bone marrow. The most common haematological disorder encountered was anemia's (26.09%), followed by plasma cell disorder (23.91%), myeloproliferative neoplasms (17.39%), lympho proliferative neoplasms (13.04%), immune thrombocytopenic purpura (10.86%), myelodysplastic syndrome (3.26%), acute myeloid leukemia, acute myeloid leukemia with myelodysplastic syndrome related changes, haemo-phagocytic syndrome, hyper-eosinophilic syndrome and myelodysplastic syndrome/myeloproliferative neoplasms (1.09%) each. Non-haematological disorders were encountered in 6% of cases, which included granulomatous lesions (50% cases), followed by metastatic solid tumour deposits (33.33%) and infection (16.67%). The diagnostic accuracy was 92% in aspiration and 100% in bone marrow biopsy.
Conclusion: This study concludes that bone marrow aspiration and biopsy are complementary to each other in diagnosing various haematological and non-haematological disorders. Therefore, simultaneous evaluation of both ensures accurate diagnosis, and further management.
Blood is an opaque fluid consists of plasma, a pale-yellow, coagulable fluid, in which different types of blood cells are suspended. These cells include erythrocytes, granulocytes, lymphocytes, monocytes, and platelets [1]. There are numerous blood and blood-related disorders which can be diagnosed by detailed clinical examination and laboratory investigations such as complete blood count, peripheral blood smear along with biochemical analysis and radiological imaging. When peripheral blood smear is not informative, further bone marrow examination and higher investigations such as cytochemistry, immunophenotyping, cytogenetic analysis and molecular genetic studies can aid for arriving at a definitive diagnosis [2].
This study encompasses the spectrum of lesions encountered in bone marrow aspiration and trephine bone marrow biopsy findings in various haematological and non-haematological disorders. The diagnostic efficacy of bone marrow trephine biopsy over the aspiration smear was evaluated.
A prospective, descriptional study was conducted in the department of KS Hedge medical academy, Mangalore between the period of January 2019 to June 2020. A total number of 100 cases were evaluated who underwent both bone marrow aspiration and biopsy. The patients with negative bone marrow aspiration and unsatisfactory bone marrow biopsy were excluded.
The clinical data was recorded including physical examination, relevant haematological, biochemical and radiological investigations.
The posterior superior iliac spine was the most suitable site used for both aspiration and biopsy. The procedure was done under local anesthesia with 2% injection lignocaine.
Bone marrow aspiration slides were stained with Leishman stain and bone marrow biopsy bits were kept for decalcification for 24 hours and then processed and stained with haematoxylin and eosin stains. Special stains were performed when ever required.
Data was analyzed by using statistical tools: SPSS software version 22.0 and CHI-square test to evaluate sensitivity, specificity, positive predictive value and negative predictive value.
Our study enlists the spectrum of lesions encountered in bone marrow aspiration and biopsy findings in various haematological and non-haematological disorders. The diagnostic efficacy of bone marrow trephine biopsy over the aspiration smear was evaluated.
A total of 100 cases were studied. Among the 100 cases studied, 92% were haematological disorders followed by 6% non-haematological disorders and 2% were normal bone marrow. Table 1, shows distribution of various haematological disorders and Table 2, shows various non- haematological lesions.
Table 1: Distribution of various haematological disorders. View Table 1
Table 2: Various non-haematological lesions. View Table 2
The age of the patients ranged from 9 to 85 years, with a mean age of 50.22 years. The most common age group of presentation in our study was 50 to 59 years, which accounted for 23% of the cases. Most of the patients were males accounting for 63% (63 cases), with male to female ratio of 1.7:1. The p- value of both bone marrow aspiration and bone marrow biopsy in relation to sex was found to be statistically significant < 0.05.
The clinical diagnosis at times may need complete blood count, peripheral blood smear for arriving at a final diagnosis. When peripheral blood smear is not informative, further bone marrow examination and higher investigations may be essential for a definitive diagnosis. It is a useful investigative tool to diagnose many haematological and non-haematological disorders and thereby, enabling to formulate an effective treatment, staging and management of malignant lesions.
A total number of hundred (100) cases were studied. The majority of cases encountered were haematological disorders accounting for 92% followed by 6% of non-haematological disorders and 2% were normal bone marrow. These findings were in concordance with various studies by Mahajan, et al. [3], Khatik, et al. [4] and Goyal, et al. [5]. The age range was between 9 to 85 years, with the mean age being 50.22 years. The age distribution was comparable to the studies conducted by Panigrahi, et al. [6], Khan, et al. [7], Tyagi, et al. [8] and Atchyuta, et al. [9].
The number of male patients in the present study were 63% and the female patients were 37% with a male to female ratio of 1.7:1. This was in concordance with the studies done by Goyal, et al. [5], Panigrahi, et al. [6], Khan, et al. [7], Atchyuta, et al. [9], and Birare, et al. [10].
Anaemia was seen in 26.09% cases wherein, bone marrow aspiration was satisfactory in 95.83%, whereas, biopsy was satisfactory in 100% cases. However, aspiration was dry tap in 4.17% cases whereas biopsy was cellular. The most common anaemia encountered was megaloblastic anaemia, which was comparable with the studies by Khatik, et al. [4], Atchyuta, et al. [9], Birare, et al. [10], Bashir, et al. [11], and Mehra, et al. [12]. The second commonest anaemia encountered was aplastic anaemia, which was in concordance with the studies by Khatik, et al. [4], Atchyuta, et al. [9], and Mehra, et al. [12]. The incidence of nutritional anaemia noted in the present study, probably because of higher prevalence of nutritional deficiencies.
Plasma cell disorders were encountered in 23.91% of cases. The most common disorder observed was Multiple myeloma (MM) with 86.35% of cases, followed by 4.55% of cases each of Plasma cell leukaemia (PCL), Walder strom macroglobunemia (WM) and Monoclonal gammopathy of undetermined significance (MGUS), which was in concordance with the studies by Atchyuta, et al. [9], Birare, et al. [10], and Vijaymohanan, et al. [13] (Figure 1). The basic panel markers used in myeloma are CD19, CD56, CD38, CD138, CD81, CD27, CD45, cytoplasmic kappa and lambda.
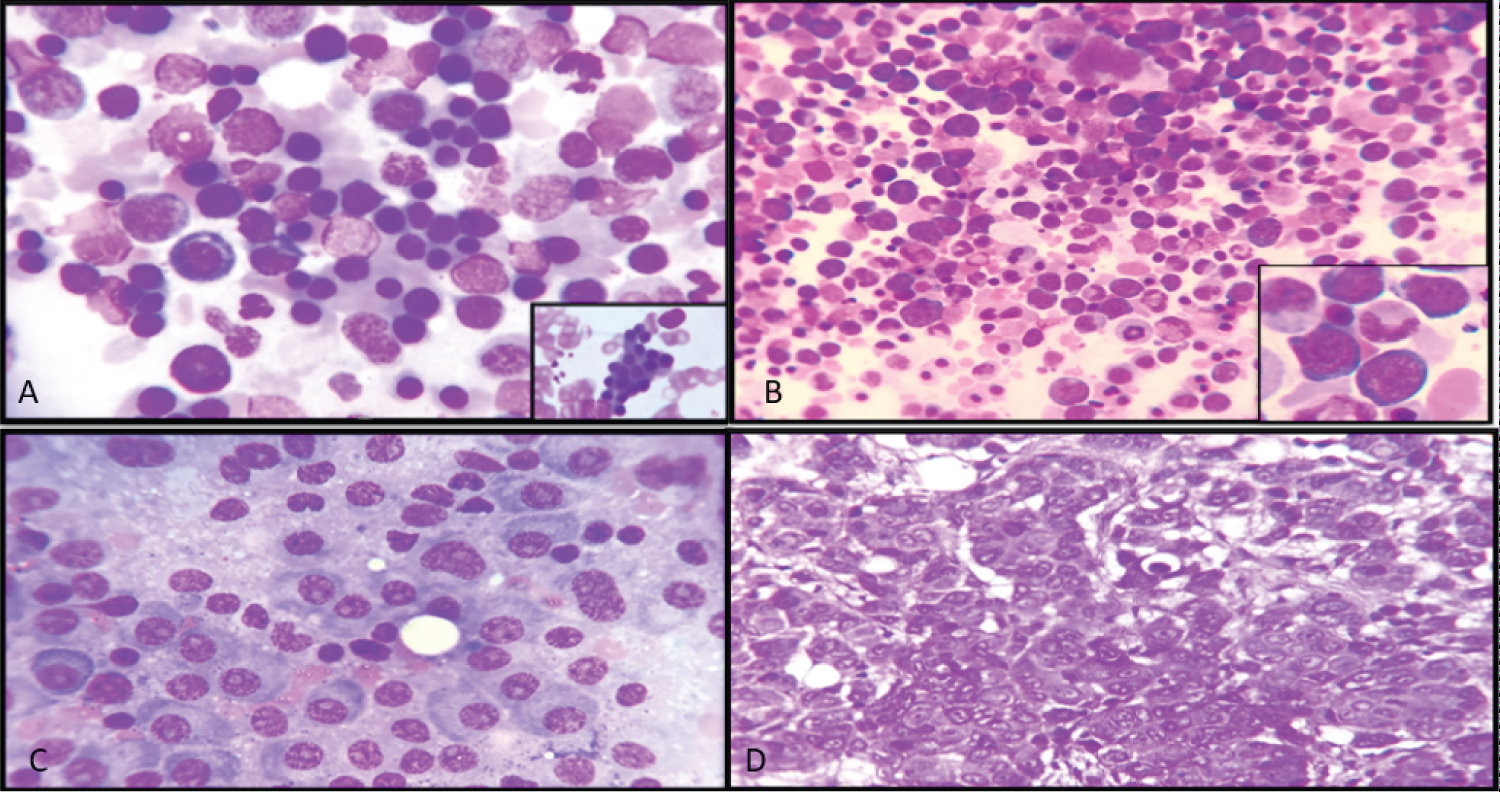 Figure 1: (A) Iron Deficiency Anaemia: Aspiration showing micro-normoblast maturation (100x), inset showing micro-normoblasts; (B) Megaloblastic Anaemia: Aspiration showing megaloblasts displaying sieve-like chromatin of the (40x), inset showing megaloblasts; (C) Multiple Myeloma: Aspiration showing sheets of plasma cells with few binucleated forms [arrow]. (100x); (D) Metastatic Deposits: Biopsy showing pleomorphic tumour cells (H&E 40x).
View Figure 1
Figure 1: (A) Iron Deficiency Anaemia: Aspiration showing micro-normoblast maturation (100x), inset showing micro-normoblasts; (B) Megaloblastic Anaemia: Aspiration showing megaloblasts displaying sieve-like chromatin of the (40x), inset showing megaloblasts; (C) Multiple Myeloma: Aspiration showing sheets of plasma cells with few binucleated forms [arrow]. (100x); (D) Metastatic Deposits: Biopsy showing pleomorphic tumour cells (H&E 40x).
View Figure 1
Among 17.39% of cases of MPNs, bone marrow aspiration was satisfactory in 68.75% of cases, and rest 31.25% were dry tap. The cause of dry tap in MPNs was probably due to increased bone marrow fibrosis or cellularity. Biopsy was satisfactory and cellular in all the cases. Bone marrow biopsy not only helps in differentiation of MPN, but also to assess cellularity, histo-topographic cell distribution, morphology of blasts as well as megakaryocytes and degree of marrow fibrosis. The most common MPN encountered in the present study was Chronic Myeloid Leukaemia (CML) accounting for 62.5% of cases, followed by Polycythaemia Vera (PV) in 18.75% of cases, 6.25% cases each of Essential Thrombocythemia (ET), Myelofibrosis (MF) and Myeloproliferative Neoplasm-unclassified (MPN-U). In the studies conducted by Khatik, et al. [4] and Atchyuta, et al. [9], the most common disorder encountered was CML as in the present study.
Biopsy gives additional information about pattern of involvement and prognosis. The detection of BM involvement virtually always advances lymphoma patients to Stage IV disease. Lymphoproliferative disorders were encountered in 13.04%. Non-Hodgkin's lymphoma was encountered in 50% cases, followed by 33.33% cases of chronic lymphocytic leukaemia/lymphoma, and 16.67% of cases were Hodgkin's lymphoma infiltrating marrow. The basic panel markers used in NHL, and CLL are CD19, CD45, FMC7, CD23, CD200, CD5, CD20, CD22, CD10, CD34, CD7, CD5, CD4, CD3, CD8, ZAP70, surface kappa, surface lambda, CD103, CD123, CD11c, TCR alpha-gamma/gamma-delta, CD26, and CD25. The prognostic markers used in CLL are CD38 and ZAP70 [14,15].
Non-haematological disorders were encountered in 6% of cases. The most common lesions encountered were granulomatous lesions in 50% of cases followed by 33.33% cases of metastatic solid tumour deposits and 16.67% cases of infection. In our study, most common non-haematological disorder encountered was granulomatous lesion followed by metastatic solid tumours which was in concordance with the studies conducted by Khatik, et al. [4], and Vijaymohanan, et al. [13].
The sensitivity of bone marrow aspiration and biopsy was 92% in our study which was comparable with the studies carried out by Khatik, et al. [4], Lukas B, et al. [16], and Chauhan, et al. [17].
The diagnostic accuracy of bone marrow aspiration noted was 92% and biopsy was 100%. The discrepancy rate between bone marrow aspiration and biopsy was 8%. The diagnostic accuracy of bone marrow aspiration was found to be lower as few cases (8 cases) showed unsatisfactory marrow aspirate/dry tap due to faulty technique.
The p-value of bone marrow aspiration and biopsy in relation to diagnosis is significant statistical, the p-value < 0.001 by chi-square method which was comparable with Goyal, et al. [5], Bashir, et al. [11], and Chauhan, et al. [17].
Bone marrow examination is helpful in arriving at final diagnosis of various haematological and non-haematological lesions. It consists of bone marrow aspiration and bone marrow biopsy which can be done in the single sitting. In bone marrow aspiration morphology of the cells are well preserved, whereas cell distribution, tumour infiltration, granuloma cells and storage cells are better appreciated on bone marrow biopsy. The bone marrow biopsy remains the gold standard for the diagnosis in negative aspiration. Simultaneous evaluation of bone marrow aspiration and biopsy show good correlation and increases the efficacy of diagnosis.