Formation of lung abscesses after Covid-19 is a newly emerging complication and superimposed mucormycosis infection is quite rare. We report the case of 62-years-old male who developed a lung abscess after being infected with SARS-COV-2. Because of the unresponsiveness to pharmacological treatment and ongoing lung damage, surgical approach was required.
This is the case of a 62-years-old patient who was transferred to our hospital for the management of a non-resolving lung abscess. He was treated for SARS-CoV-2 infection two months prior to this presentation.
The CT scan showed a well demarcated lesion measuring 9.7/8.2/8 cm, displaying fluid levels, located in the posterior region of the superior right lobe.
The lesion appeared to be communicating with the right upper lobar bronchus and possibly with the right main bronchus. Similar smaller lesions were also identified in the anterior region, base and periphery of the right superior lobe and as well as in the medial lobe.
The rest of the lung parenchyma showed micronodular interstitial ground glass condensations and a tree-in-bud pattern (Figure 1 and Figure 2).
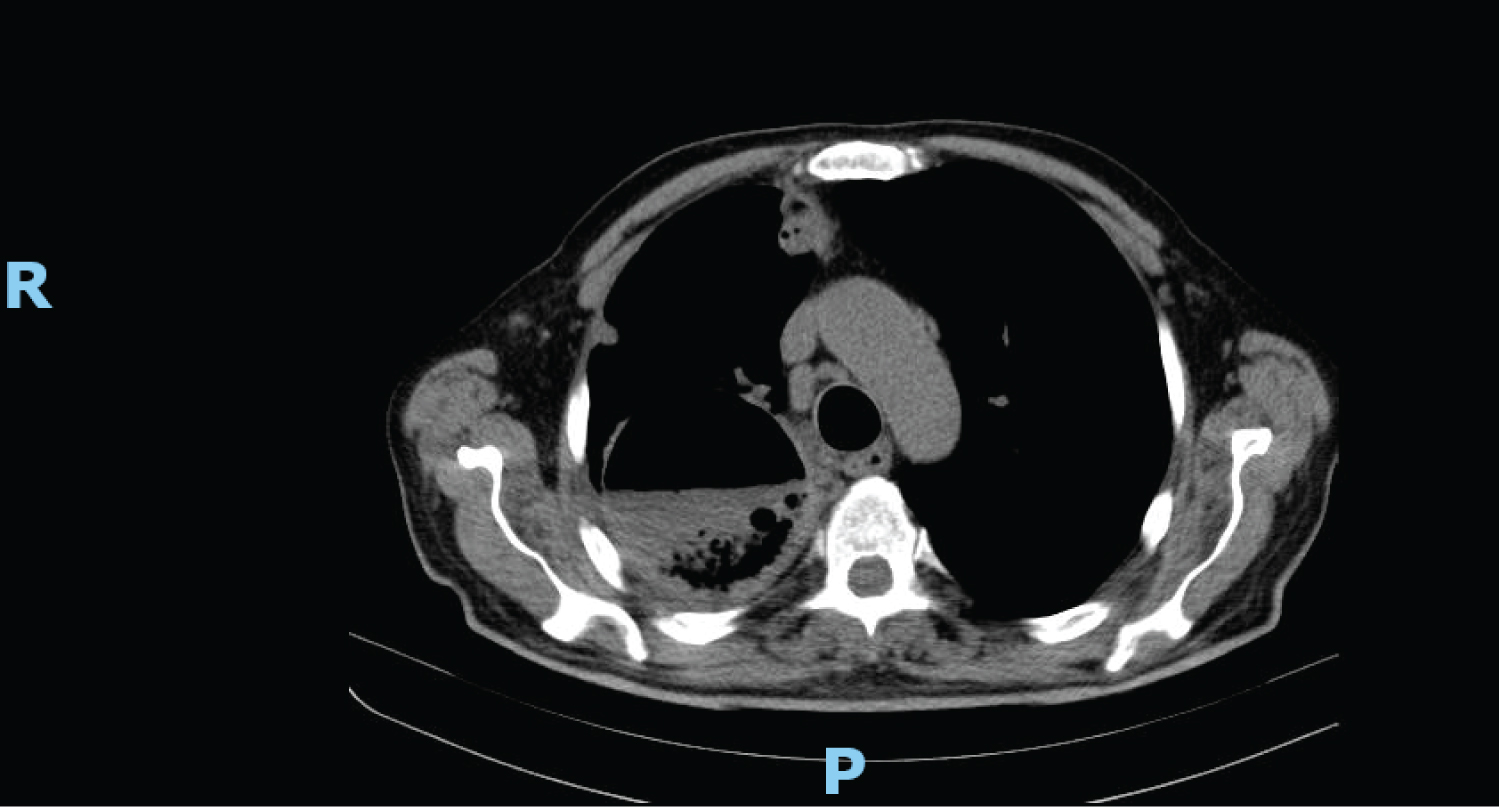 Figure 1: CT scan showing a well demarcated round lesion with gas-liquid level.
View Figure 1
Figure 1: CT scan showing a well demarcated round lesion with gas-liquid level.
View Figure 1
 Figure 2: CT scan showing the same lesion form the right lung, at an inferior level.
View Figure 2
Figure 2: CT scan showing the same lesion form the right lung, at an inferior level.
View Figure 2
Under the suspicion of damage of right superior lobar bronchus extending to the main right bronchus and after careful evaluation of the patient's physical status and associated pathologies comorbidities (arterial hypertension, diabetes mellitus, arterial flutter and left bundle branch block), a right superior bilobectomy was proposed. During the surgery, a complete right pneumectomy was performed because of the longitudinal bronchial defect with ulceration and necrosis, and the impossibility of performing a tension-free bronchoplasty.
Pathologic evaluation revealed a classic image of bacterial lung abscess with extensive necrotic debris, acute inflammation and few bacterial colonies, surrounded by granulation tissue (Figure 3). Inside the necrotic debris there were broad, non-septate hyphae, irregularly branched at almost 90 degrees (Figure 4), features suggestive of Mucormycosis.
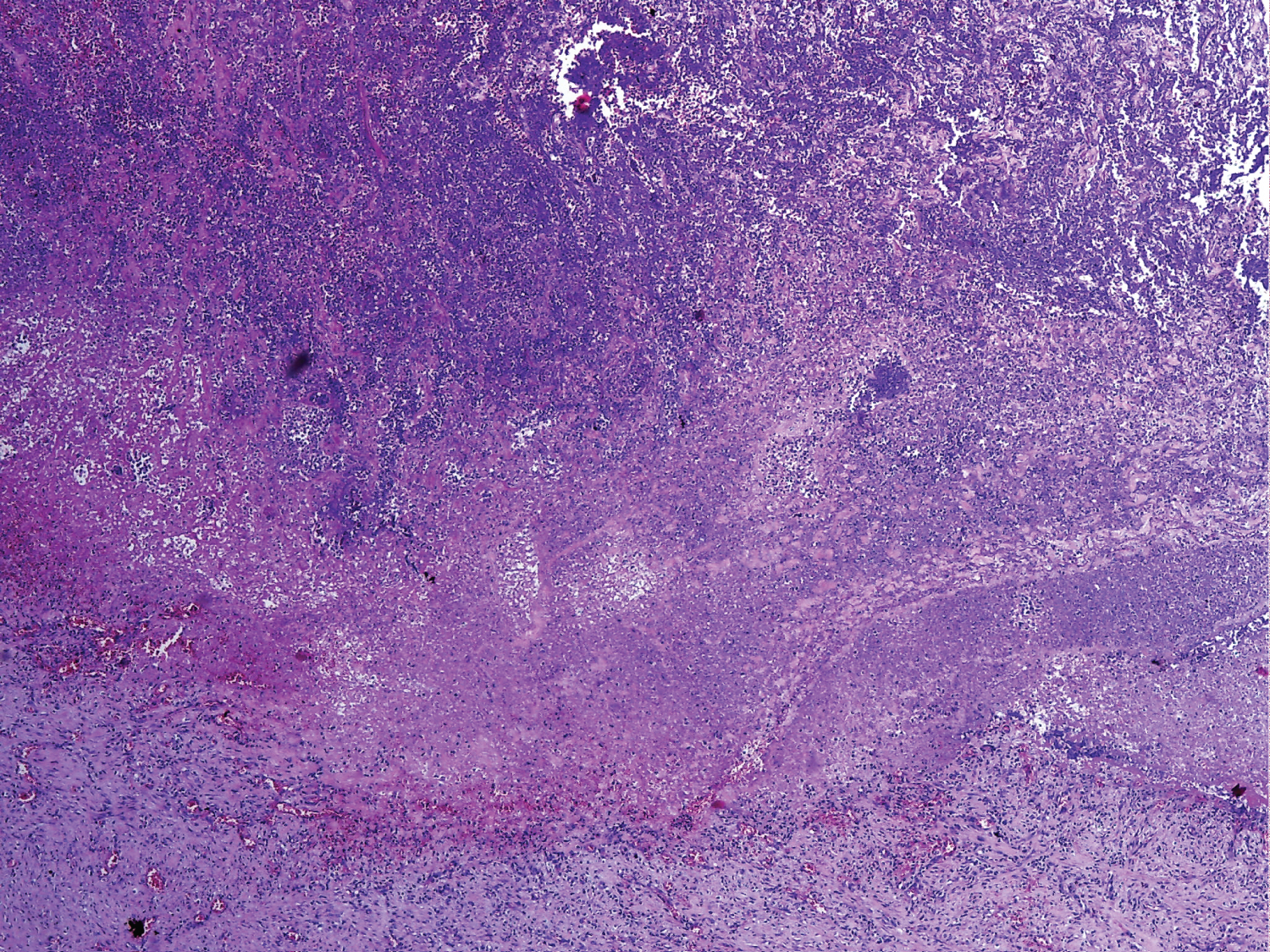 Figure 3: HE x100 section through abscess wall showing extensive necrotic debris in the upper portion, lined by granulation tissue.
View Figure 3
Figure 3: HE x100 section through abscess wall showing extensive necrotic debris in the upper portion, lined by granulation tissue.
View Figure 3
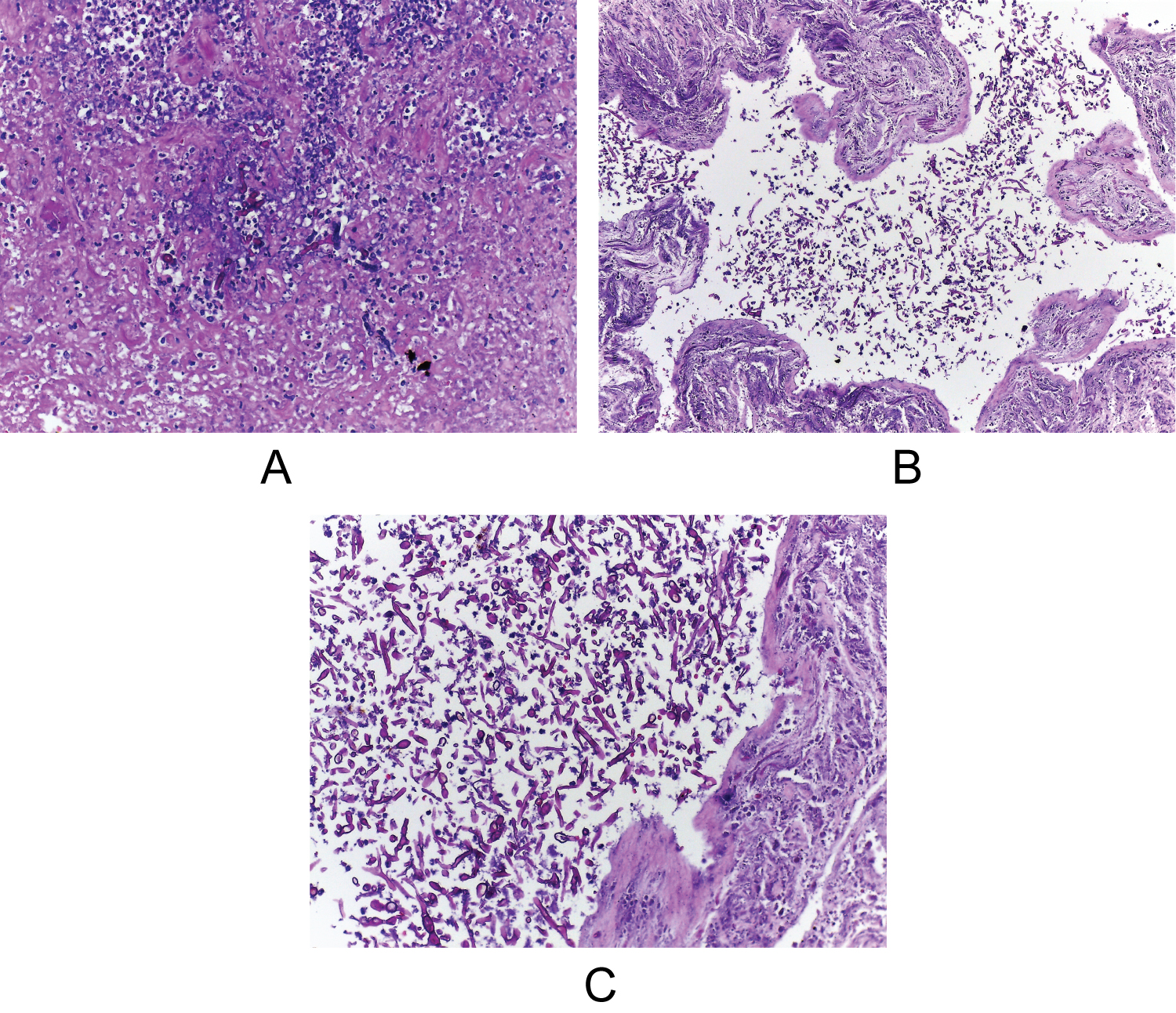 Figure 4: Mucormycosis broad, non-septate, irregularly branched hyphae inside necrotic debris HE x200 (4a); HE x100 (4b); HE x200 (4c).
View Figure 4
Figure 4: Mucormycosis broad, non-septate, irregularly branched hyphae inside necrotic debris HE x200 (4a); HE x100 (4b); HE x200 (4c).
View Figure 4
The rest of the lung parenchyma showed frequent pus containing bronchioles with granulocytes extending in the neighboring alveolar spaces (Figure 5), alveolar edema, areas with type 2 pneumocyte hyperplasia (Figure 6), areas of organizing and fibrosing diffuse alveolar damage (Figure 7).
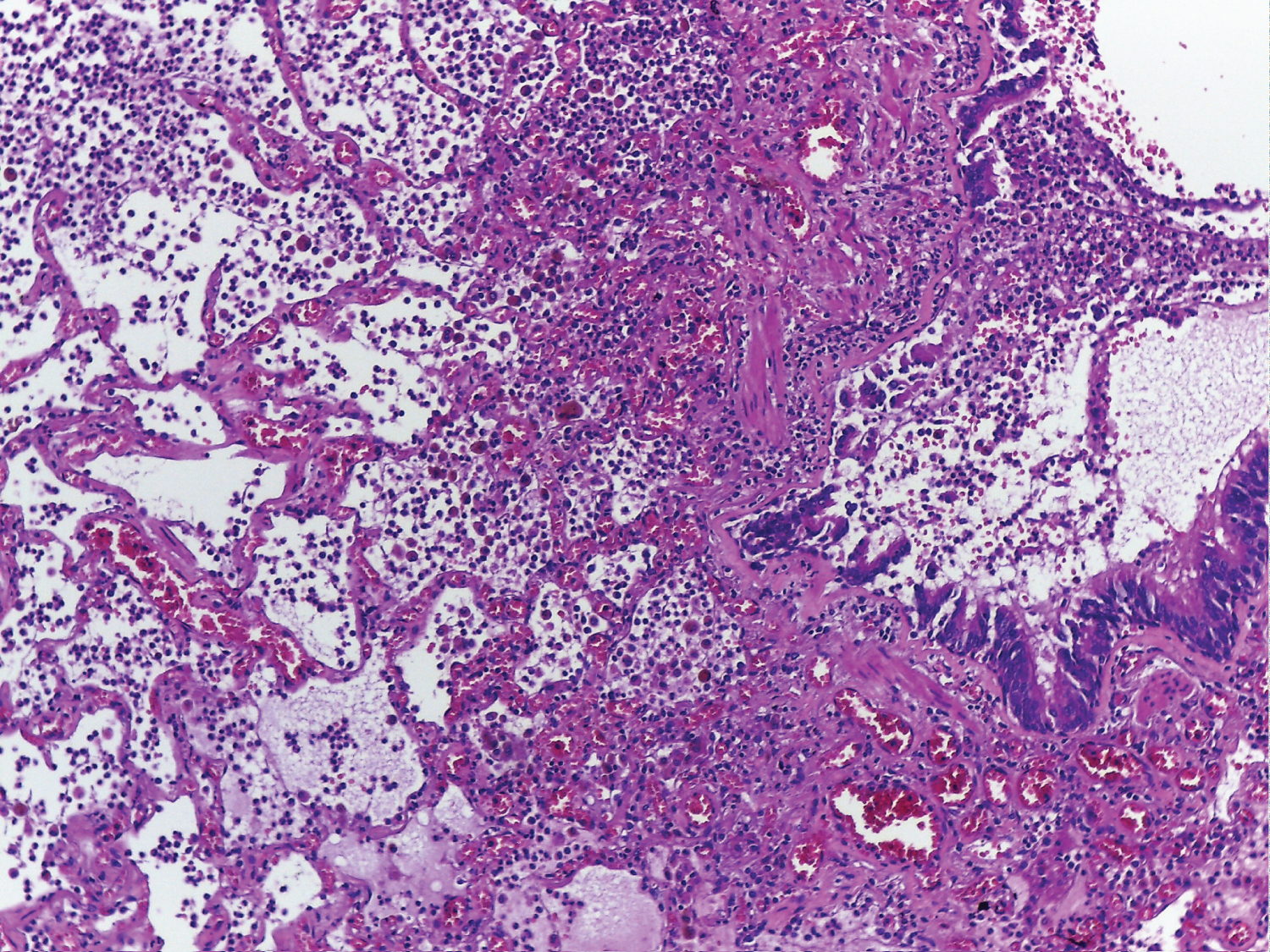 Figure 5: Section through lung parenchyma showing bronchiolitis with granulocytes extending in the neighboring alveolar spaces, edema and congestion, HE x100.
View Figure 5
Figure 5: Section through lung parenchyma showing bronchiolitis with granulocytes extending in the neighboring alveolar spaces, edema and congestion, HE x100.
View Figure 5
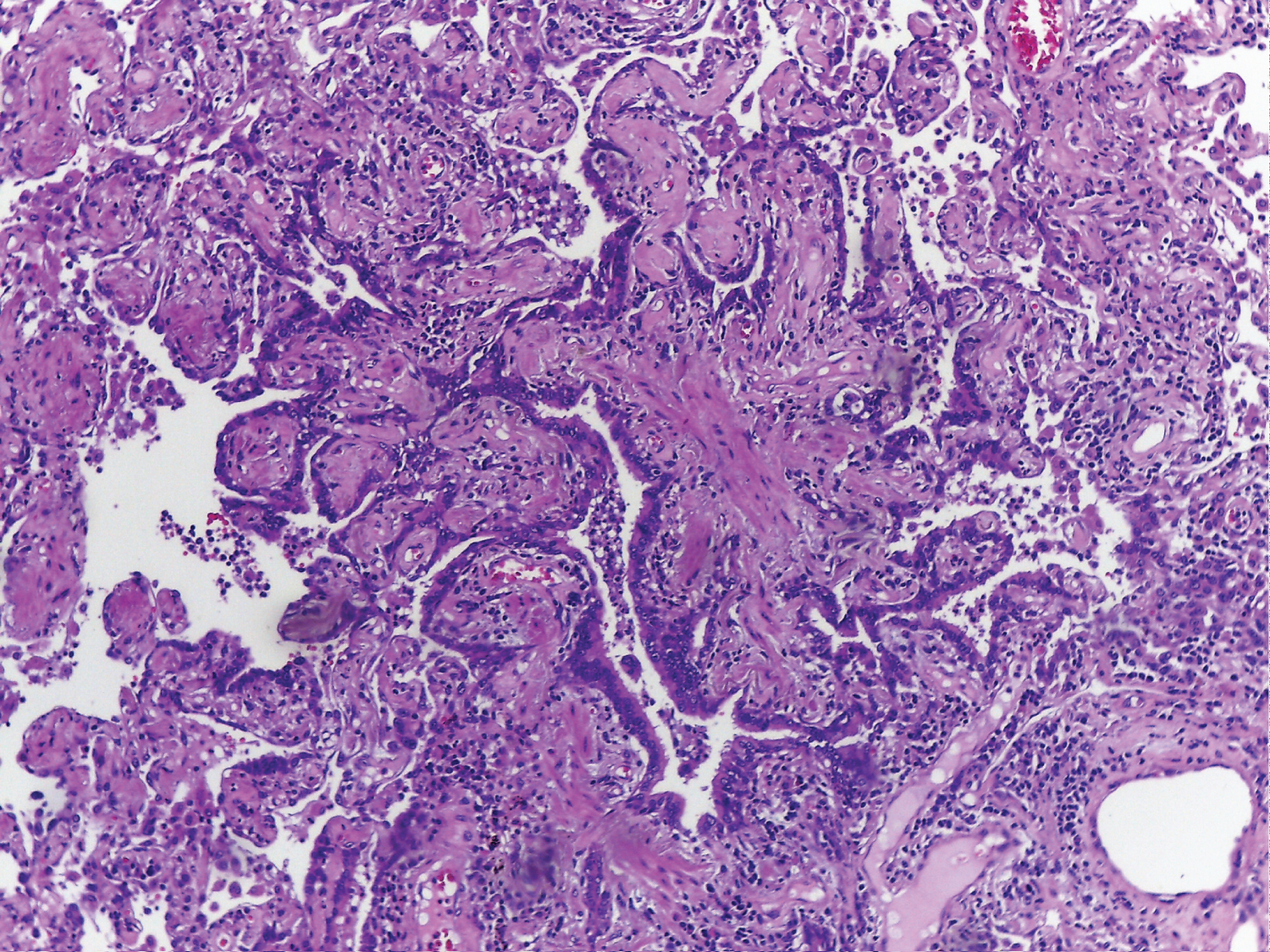 Figure 6: HE x100 lung parenchyma with an area of type 2 pneumocyte hyperplasia and organizing pneumonia.
View Figure 6
Figure 6: HE x100 lung parenchyma with an area of type 2 pneumocyte hyperplasia and organizing pneumonia.
View Figure 6
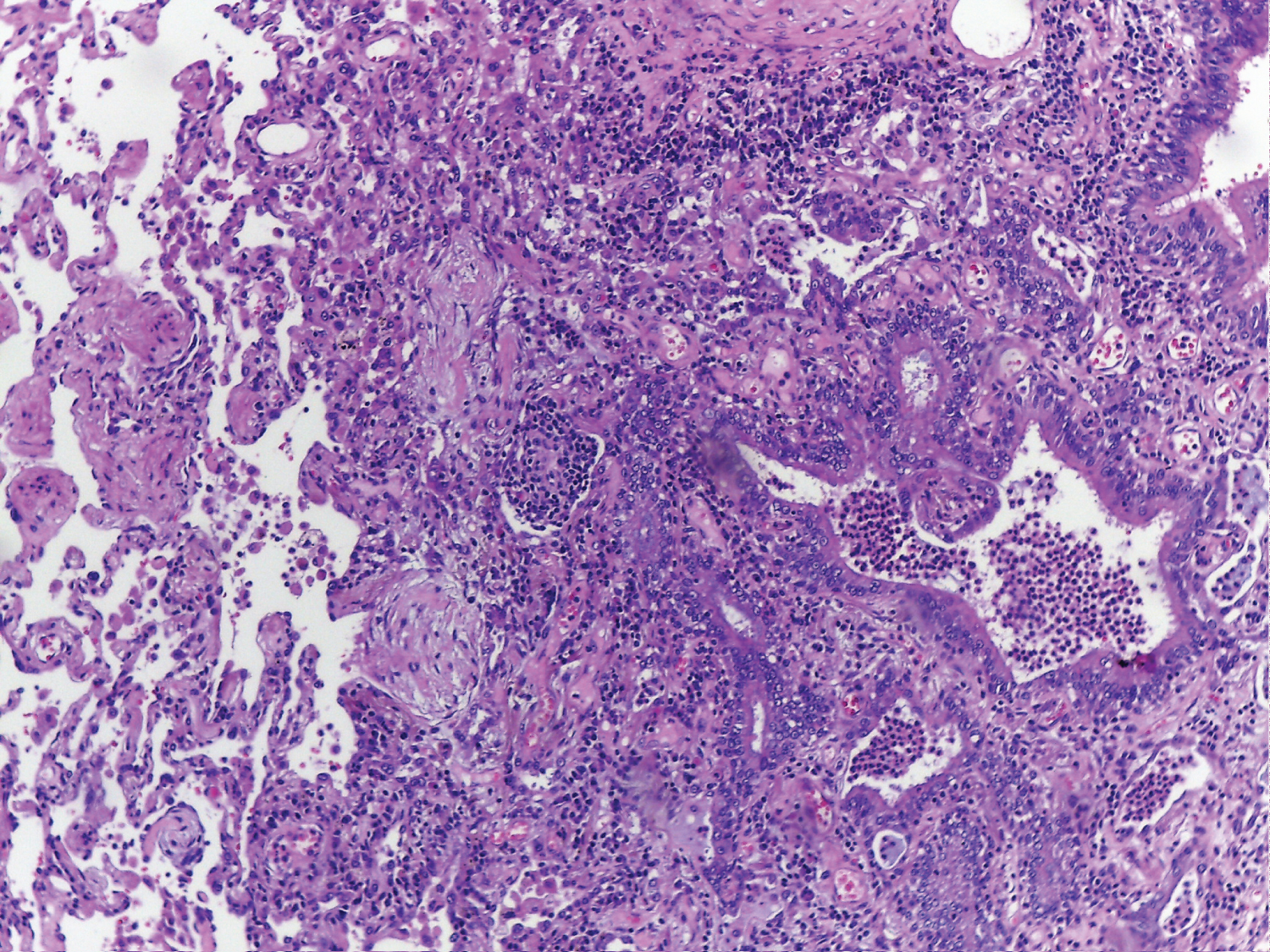 Figure 7: HE x100 section showing areas of organizing and fibrosing diffuse alveolar damage.
View Figure 7
Figure 7: HE x100 section showing areas of organizing and fibrosing diffuse alveolar damage.
View Figure 7
Pulmonary mucormycosis is an uncommon fungal infection caused by the microorganisms form the Mucorales order. This opportunistic pathogen affects mainly immunocompromised patients [1] and in one study it accounted for 8.3%-13% of all fungal infections discovered at autopsy, much rarer than candidiasis or aspergillosis [2,3].
Mucormycosis infection is currently an important issue in India due to its unprecedent surge and high morbidity [4], fatality rates being close to 100% in severe cases [5]. The most involved regions are the head and neck, the respiratory and central nervous systems, the gastrointestinal tract, and other areas [6] rhino-cerebral mucormycosis being the most frequently reported in the literature.
This case presents a COVID-19 positive patient who developed pneumonia complicated by lung cavitations and pulmonary mucormycosis. The potential pathogenic links between those entities are discussed below.
Possible mechanisms through which COVID-19could contribute in the development of pulmonary mucormycosis may include impaired host defense against fungi by viral-induced lymphopenia or the therapeutic use of corticosteroids and/or hydroxychloroquine, both likely to impair phagocytic immune-cell response, which is the major defense mechanism against mucormycosis [1].
SARS-CoV-2 induced pneumonia can uncommonly present as lung cavitation [7]. Although the exact mechanism is unknown, some autopsy reports found diffuse alveolar damage, intra-alveolar hemorrhage and necrosis of parenchymal cells, which may be responsible for cavitation in COVID-19 pneumonia [8].
During the present pandemic, post COVID lung abscess formation has been reported in many countries. In a study realized on 188 French patients, the authors identified lung abscesses in 14% of the cases, which is higher than the 1.4% rate reported in a retrospective study that was not specifically focusing on lung abscess [9,10]. The clinical setting included a latency between 22 days and more than one month after the initially full recovery [11,12].
In our case, mucormycosis suprainfection was the cause for the unresponsiveness to the pharmacological approach and the progression of the lung damage even under treatment.
This fungus was discovered only on histology specimens and it solely involved the lung tissue. To our knowledge this is the first case of a Romanian patient showing a possible link between Covid-19, lung abscess and mucormycosis.
The clinical spectrum of disease secondary to SARS-CoV-2 continues to evolve. Early and late complications associated with COVID-19 are still unknown. Common causes of cavitary lung lesions must be investigated appropriately in all patients. Clinicians must be aware of evolving CT findings of COVID-19 and must arrange appropriate follow-up of convalescent patients with COVID-19 to ensure complete recovery.