Intestinal ganglioneuromatosis is a rare neoplastic disease characterized by an important proliferation of Schwann cells, nerve fibers and ganglion cells in the intestinal wall. We present a case of 36-years-old male who presented with abdominal pain, constipation and vomiting of several days duration. On admission, intestinal occlusion was suspected and urgent laparotomy was done during which numerous nodules were found in the small bowel. Eventually, a segment of the bowel was resected and histopathological examination revealed a diffuse intestinal ganglioneuromatosis. Despite its rarity, this disease should always be considered in the differential diagnosis of intestinal mass in any adult patient.
Intestinal ganglioneuromatosis, Intestinal occlusion, Histopathology
Intestinal ganglioneuromatosis is a neoplastic disease characterized by an important proliferation of Schwann cells, nerve fibers and ganglion cells in the intestinal wall [1-6]. It is a very rare condition that can occur in any part of the gastrointestinal tract [2,5]. The most common parts that can be affected by the disease are the ileum, colon and appendix [2,5]. It is frequently seen in children and found equally in both sexes [6].
This condition was divided into 3 types according to Shekita and Sobin in 1994: Polypoid ganglioneuroma, ganglioneuromatous polyposis, and diffuse ganglioneuromatosis [2,5,6]. The first one can present as a solitary or some small polyps seen mostly in colon and the lesions can be mucosal or submucosal. The second form is located mostly in colon or terminal ileum and characterized by numerous polyps (> 20) with either mucosal or submucosal presentation. This type can be associated with MEN2b, NF1, Cowden disease or juvenile polyposis.
A diffuse intra or transmural lesions with myenteric plexus hyperplasia characterize the last type. This condition can be associated with tuberous sclerosis, Cowden disease, MEN2b, NF1 or juvenile polyposis [2,6].
Intestinal ganglioneuromatosis can present in variable clinical pictures, according to the extent of the lesion and on its location [2,5,6]. The patient can experience abdominal pain, stricture formation, change in bowel habits and can even present with iron deficiency anemia secondary to the ulceration of the mucosa [5].
Here we present the case of a 37-years-old patient, known to have multiple skin lesions reminiscent of neurofibromas as informed by the attending physician, with a clinical presentation of intestinal obstruction who was diagnosed later on with diffuse intestinal ganglioneuromatosis.
A 36-year-old man known to have multiple brown skin lesions reminiscent of neurofibromas presented for abdominal pain, constipation, and vomiting of several days duration. No information is available about the workup done upon admission and the imaging tests performed. Intestinal occlusion was suspected and the patient was referred for urgent laparotomy. During laparotomy patient was found to have numerous nodules in the small bowel causing intestinal obstruction, so resection of a segment of the intestine was performed by the surgeon.
Grossly the resected segment measured 90 × 5 cm. It showed numerous beige serosal and mesenteric nodules the largest of which measured 7 × 3 cm with a tan-beige, focally yellowish, myxoid and fibrous aspect (Figure 1). Cross section revealed a diffusely thick intestinal wall. Mucosa was largely eroded. A perforated area was grossly seen. The mucosa also presented few submucosal lipomas the largest of which measured 2 cm. An appendix was received separately measuring 6.5 × 0.5 cm. Few lymph nodes were dissected.
 Figure 1: (A,B) Intestinal segment showing numerous beige serous and mesenteric nodules the largest of which measures 7 × 3 cm with a myxoid, adipose and fibrous appearance.
View Figure 1
Figure 1: (A,B) Intestinal segment showing numerous beige serous and mesenteric nodules the largest of which measures 7 × 3 cm with a myxoid, adipose and fibrous appearance.
View Figure 1
Microscopic examination showed at the level of the macroscopically described beige nodules a benign, exuberant nodular proliferation made up of nerve fibers, ganglion cells and supporting spindle cells reaching the submucosa, muscularis propria and serosa (Figure 2). The stroma of these nodules is myxoid in some nodules and fibrous in others (Figure 3). Otherwise, the ileal mucosa was largely ulcerated and presented an architectural disorder. The fibrous wall was densified by a chronic active leucocytic exudate reaching the sub-serosa and containing numerous eosinophils and plasma cells (Figure 4). Multiple submucosal nodules formed of adipocytes of varying size lobulated by fine fibrous streaks were noted. The appendix was unremarkable. The lymph nodes exhibited reactive histologic features.
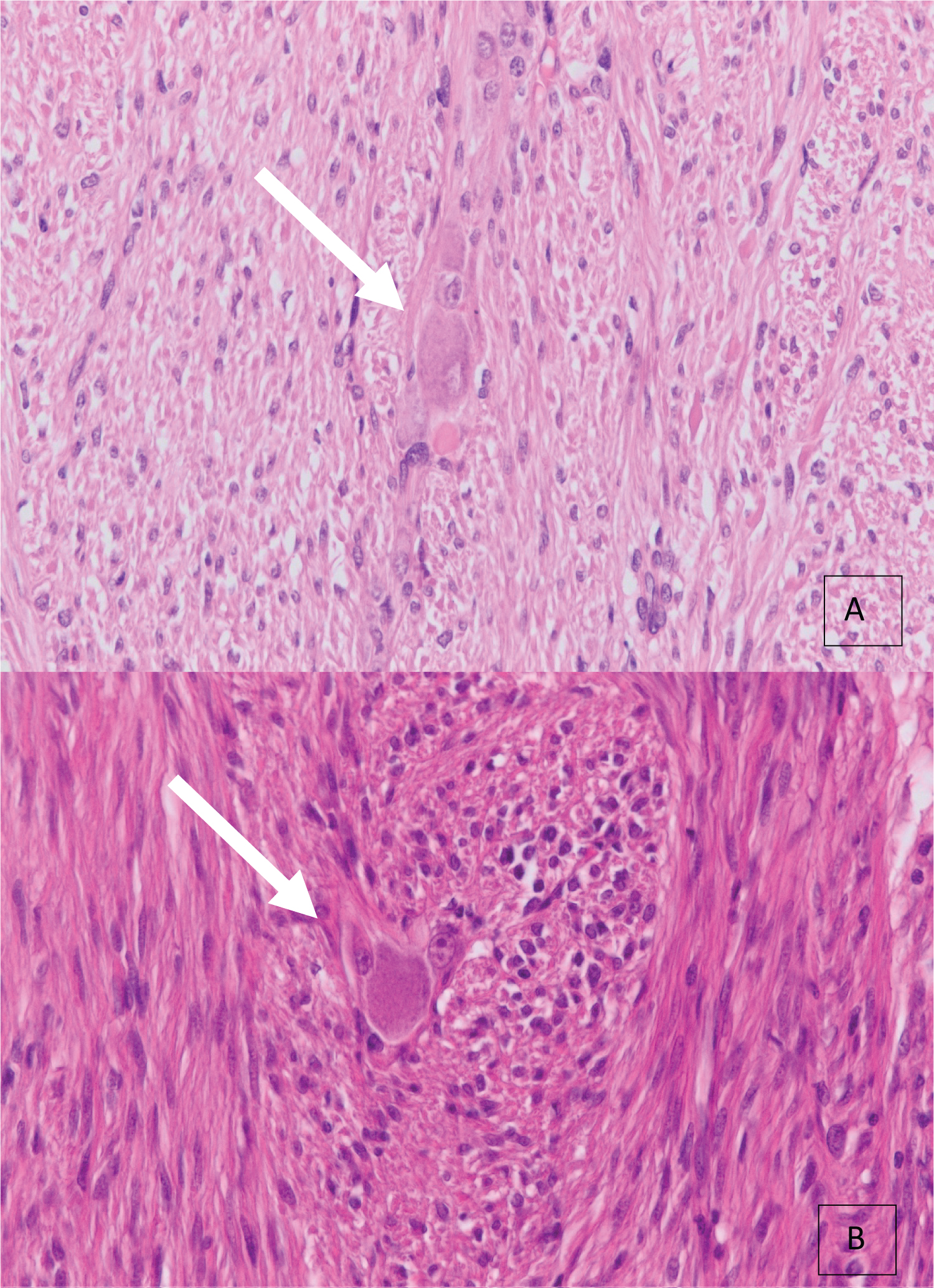 Figure 2: (A,B) Microscopic examination showing a benign proliferation composed of nerve fibers, ganglion cells and supporting spindle cells (H&E X400).
View Figure 2
Figure 2: (A,B) Microscopic examination showing a benign proliferation composed of nerve fibers, ganglion cells and supporting spindle cells (H&E X400).
View Figure 2
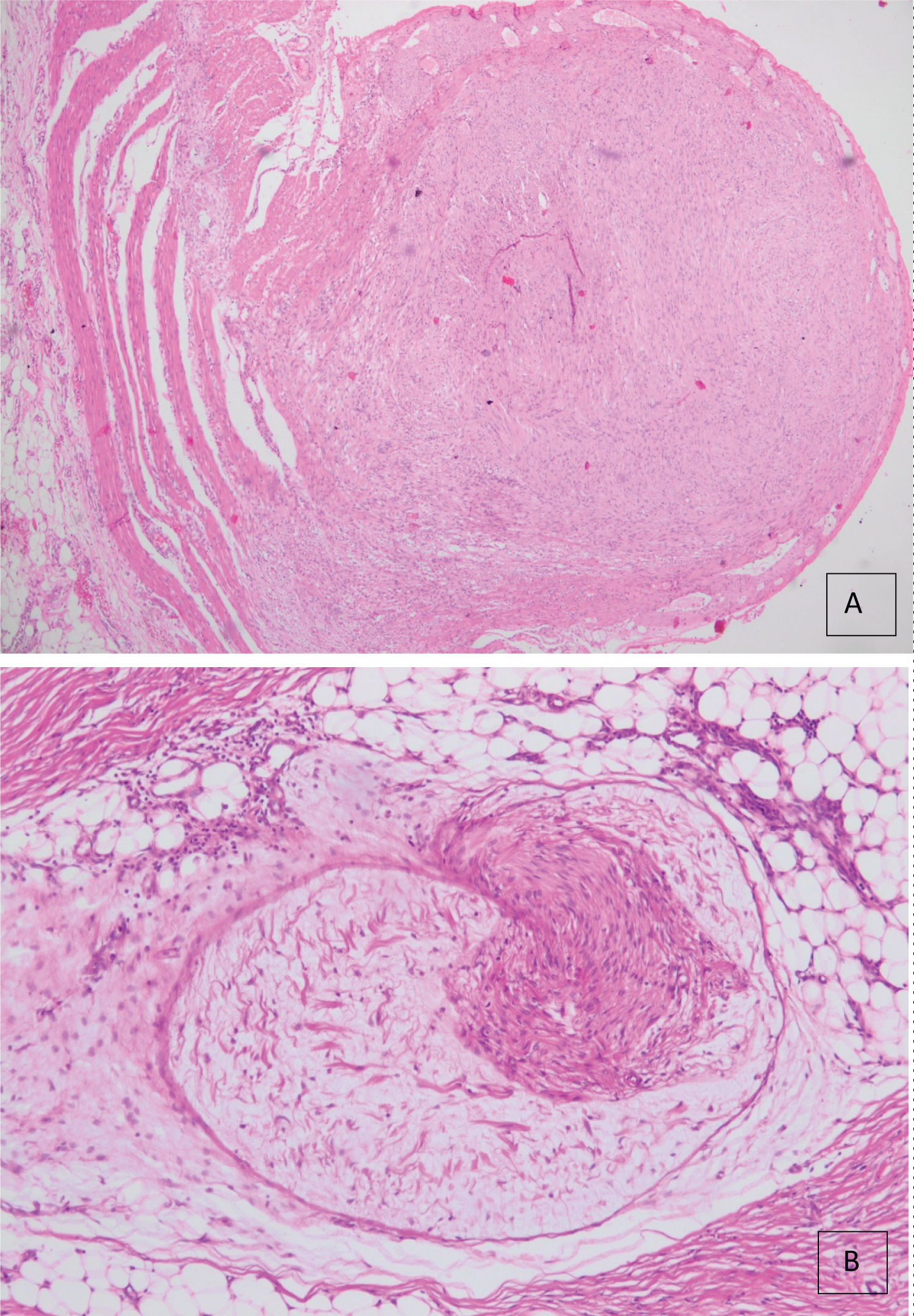 Figure 3: (A,B) Microscopic examination showing a fibrous stroma in some nodules (A) and myxoid in others (B) (H&E X40, X100).
View Figure 3
Figure 3: (A,B) Microscopic examination showing a fibrous stroma in some nodules (A) and myxoid in others (B) (H&E X40, X100).
View Figure 3
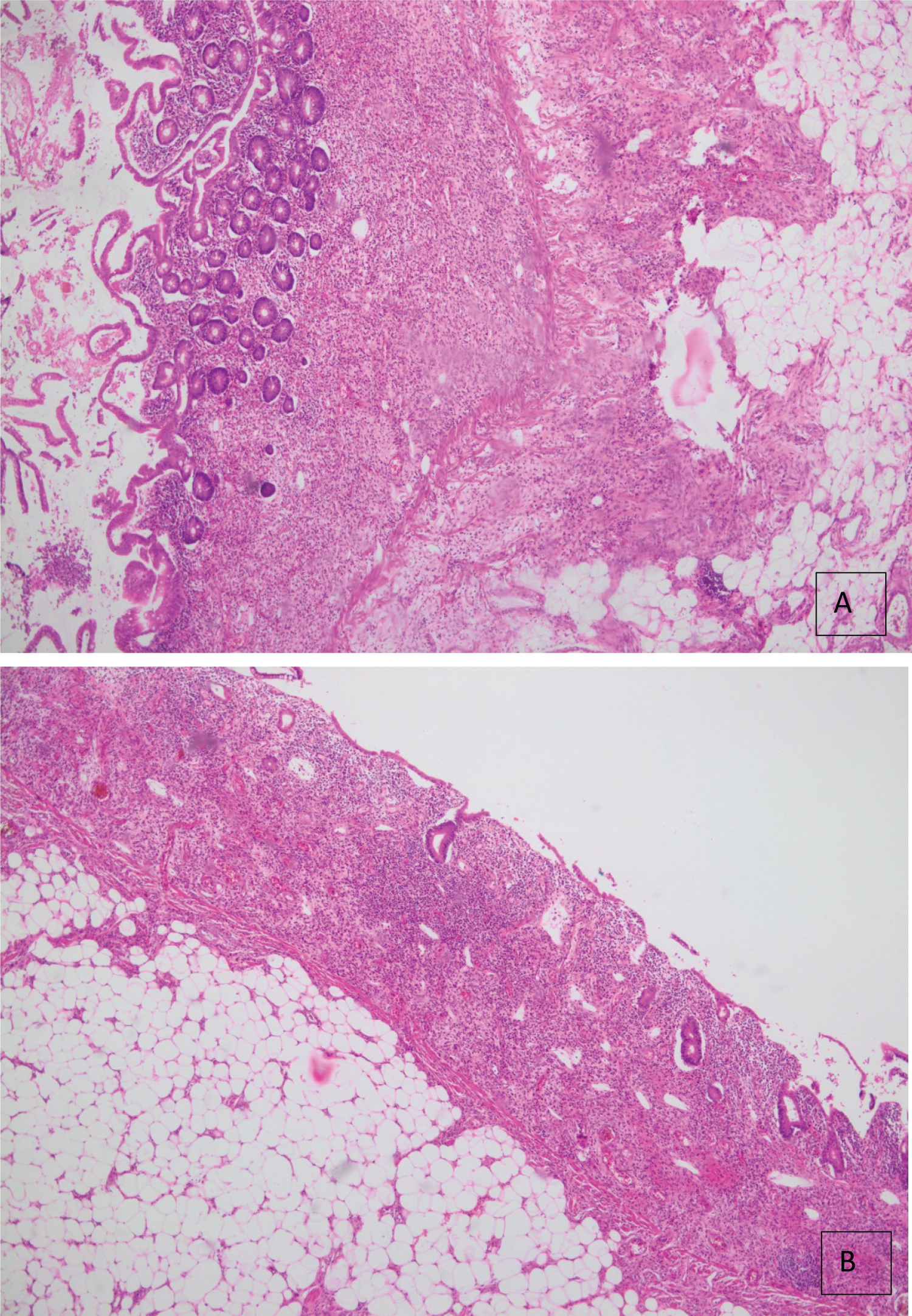 Figure 4: (A,B) Microscopic examination showing a largely ulcerated ileal mucosa exhibiting an architectural disorder. The fibrous wall is densified by a chronic active leukocytic exudate reaching the sub-serosa and containing numerous eosinophils and plasma cells (H&E X40).
View Figure 4
Figure 4: (A,B) Microscopic examination showing a largely ulcerated ileal mucosa exhibiting an architectural disorder. The fibrous wall is densified by a chronic active leukocytic exudate reaching the sub-serosa and containing numerous eosinophils and plasma cells (H&E X40).
View Figure 4
Immunohistochemistry was done and showed a positive staining of calretinin and synaptophysin in neural and ganglion cells. S100 was strongly expressed in the nerve fibers. Smooth muscle actin (SMA) was negative in tumor cells (Figure 5).
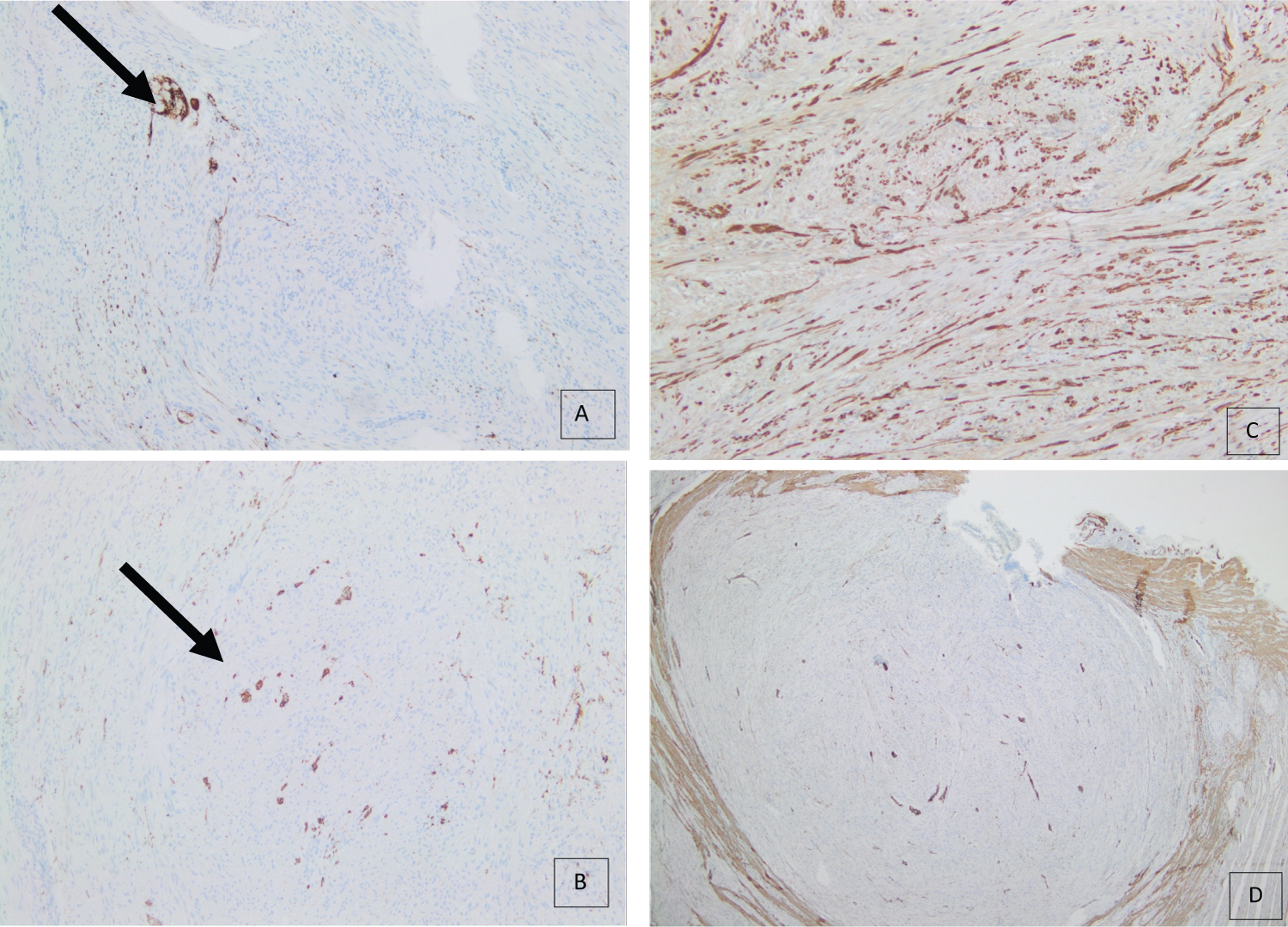 Figure 5: (A,B,C,D) Immunohistochemistry with Calretinin (A) and synaptophysin (B) highlighting the neural and ganglion cells. (C) Nerve fibers show a strong S100 expression. (D) Negative expression of SMA by both nerve fibers and ganglion cells (X100, X100, X100, X40).
View Figure 5
Figure 5: (A,B,C,D) Immunohistochemistry with Calretinin (A) and synaptophysin (B) highlighting the neural and ganglion cells. (C) Nerve fibers show a strong S100 expression. (D) Negative expression of SMA by both nerve fibers and ganglion cells (X100, X100, X100, X40).
View Figure 5
In conclusion the histological and immunohistochemical profile were compatible with diffuse intestinal ganglioneuromatosis associated with chronic active and erosive transparietal inflammation, pathologic findings similar to those seen in patients with Crohn's disease. Multiple submucosal lipomas were also present. The appendix was normal. The lymph nodes were reactive.
Intestinal ganglioneuromatosis is a rare disease of the enteric nerve system, characterized by an abnormal proliferation of ganglion cells, nerve fibers, and Schwann cells. This disease can occur in any part of the gastrointestinal tract. Epidemiologically, it has no sex predilection and it is more frequently seen in children [1]. Clinically, Intestinal ganglioneuromatosis can present with variable symptoms including abdominal pain, diarrhea, change in bowel habits, bleeding, or constipation due to stricture formation in the case of intestinal obstruction. This clinical presentation depends on the location of the lesions, their extent, and their impact on the gastrointestinal motility [2,3]. Similarly the patient in our case presented with abdominal pain, obstipation, and vomiting, thus with the typical clinical presentation of abdominal obstruction.
Intestinal ganglioneuromatosis is a rare benign neoplastic disease that includes a group of pathologic findings [4]. Some patients develop a polypoid form of ganglioneuromas (solitary or multiple) composed of ganglion cells and spindle cells and usually encountered in the colon. Others develop multiple polyps usually in the terminal ileum and the colon, a condition termed "ganglioneuromatosis polyposis". Diffuse intestinal ganglioneuromatosis, as its name implies, is a diffuse form of the disease characterized by myenteric plexus hyperplasia with ill-defined infiltrative proliferation of ganglioneuromatous tissue in the wall of the ileum, colon, and appendix. The latter can be intramural or transmural. Our case is transmural. Diffuse ganglioneuromatosis resembles "ganglioneuromatosis polyposis" by being associated with MEN2b, NF1, juvenile polyposis, tuberous sclerosis, Cowden disease... etc. When affecting the terminal ileum, diffuse intestinal ganglioneuromatosis can lead to pronounced thickening of the bowel wall, nodular submucosal proliferation, and prominent stricture formation, findings that have been reported in the gross description of our specimen [4]. The patient in our case had a diffuse intestinal ganglioneuromatosis possibly associated with neurofibromatosis given the fact that the patient had already had multiple skin lesions reminiscent of neurofibromas as informed by the attending physician.
With the absence of specific clinical presentations and imaging manifestations, the diagnosis of intestinal ganglioneuromatosis remains challenging. Differential diagnosis includes intestinal tuberculosis, inflammatory bowel disease (Crohn disease), intestinal tumors (like adenocarcinoma, GIST, lymphoma, leiomyoma...), NSAIDs enteropathy, Cytomegalovirus infection, and amyloidosis [5]. In the case of our patient, the major differential diagnosis was GIST, as was suggested by pre-operative radiologic findings. However, the definitive diagnosis established by pathologic examination revealed diffuse intestinal ganglioneuromatosis. In fact, GIST and diffuse intestinal ganglioneuromatosis share in common most of their clinical and radiological features i.e both can present with abdominal pain, bleeding, changes in bowel habits, and even intestinal obstruction, and both usually show submucosal soft tissue masses on imaging tests. Therefore, the exact and final diagnosis relies on pathological examination post-operatively. Treatment of diffuse intestinal ganglioneuromatosis remains surgical by resection of the involved intestinal segment in symptomatic cases [6].
As a summary, we report a rare case of a patient with diffuse intestinal ganglioneuromatosis presenting with typical clinical picture and in whom the radiological findings mimicked those of GIST. The final diagnosis was made by referring to the pathological examination of the resected intestine. Given the rarity of the disease along with the non-specific clinical, laboratory, and radiologic findings, physicians can easily miss it. However, it should always be considered in the differential diagnosis of intestinal mass in any adult patient.
The authors declare they have no conflicts of interest.
All authors contributed equally in medical writing and reviewing the manuscript.